Annals of Medical & Surgical Case Reports
Short Communication
A Misdiagnosed Case of PCOS: Cushing's Disease
Vinuta Mohan, MD1* Robert Lind, MD2
*Corresponding author: Vinuta Mohan, Department of Endocrinology, SaintFrancis Medical Center, 601 Hamilton Ave, Trenton, NJ 08629, USA, Tel: +16095995435, Email: vmohan@stfrancismedical.org
Citation: Mohan V (2019)A Misdiagnosed Case of PCOS: Cushing's Disease. Ann Med &Surg Case Rep: AMSCR: 100010
Received Date: 29 May, 2019; Accepted Date: 01 June; Published Date: 07 June, 2019
INTRODUCTION
A 33-year-old Hispanic female presented to the medical clinic with complaints of oligomenorrhea and infertility for 1 year. She had a 12 year old son whom she conceived without difficulty and desired another child. She had no previous significant medical or surgical history and was not on any medications. She did not smoke, did not drink and denied any recreational drugs. She had a strong history of type 2 diabetes in her family. On review of symptoms she reported a 10-pound weight gain over the past few years. Her physical exam was remarkable for obesity with a body mass index of 30. Her blood pressure was 132/84 mmHg and her pulse were 78 bpm. Her skin exam was remarkable for hirsutism but there were no abdominal striae, moon facies or buffalo hump. Laboratory testing revealed a negative bhCG, TSH of 2.65 mIU/L (0.4-4), prolactin of 18.3 ng/mL (2-20), fasting glucose of 83 mg/dl (70-99) and an elevated testosterone of 71 ng/dl (2-45). Pelvic ultrasound revealed her ovaries were within normal limits for size and echogenicity. However, bilateral ovarian cysts were noted (Figures 1 and 2), so her primary care physician presumptively diagnosed her with polycystic ovarian syndrome (PCOS). She was started on metformin therapy and treated for 2 years with no improvement of her menstrual cycle, so she was then referred to an endocrinologist for further evaluation.
On further examination and history, the patient was found to have supraclavicular fat and reported a previous non-traumatic rib fracture which had healed. A dual energy x-ray absorptiometry (DEXA) was remarkable for osteopenia of the lumbar spine with a t-score of -1.7 and a z score of -1.9.Twenty-four-hour urine cortisol was elevated at 173 mcg (4-50). A simultaneous morning ACTH and cortisol were 133 pg/mL (6-50) and 22 mcg/dL (4-20) respectively, consistent with ACTH-dependent Cushing's syndrome (CS).1milligram dexamethasone testing was done and her cortisol failed to suppress (8.1 mcg/dl). A pituitary MRI with contrast revealed a 5mm adenoma (Figures 3 and 4)and she underwent transphenoidalresection for Cushing's disease. Pathology confirmed a 5 × 5 × 3mm tumor that was positive for chromogranin and ACTH immunostaining, consistent with her diagnosis. She was weaned off all steroid therapy within 2 months. Approximately 4 months after surgery, her menses resumed and she reported regular cycles.
DISCUSSION
CS is an extremely rare disease with an annual incidence of 1 to three cases per million people per year, whereas PCOS is a much more common condition, affecting approximately 10% of women of reproductive age. CS is a potentially a curable condition, whereas PCOS is mostly managed by healthy lifestyle and medications to treat the symptoms. Female patients with CS and PCOS may share signs and symptoms of hyperandrogenism as well as have similar findings on ovarian ultrasound. Therefore, CS patients are unfortunately often misdiagnosed, resulting in prolonged health risks of hypercortisolemia such as osteoporosis, hypertension, diabetes and cardiovascular disease. It is very important that clinicians remember that PCOS is a diagnosis of exclusion. Other causes need to be considered and ruled out before making the diagnosis of PCOS. A high clinical suspicion remains the cornerstone of a CS diagnosis [1,2].
Learning Points/Take Home Messages
1. PCOS is one of the most common endocrine causes for oligomenorrhea, affecting up to 10% of women of reproductive age, but it is a diagnosis of exclusion.
2. Women with Cushing's syndrome may also present with menstrual irregularities, mimicking PCOS.
3. It is critical to perform a detailed history and physical exam when evaluating women with these symptoms so as not to make the wrong diagnosis.
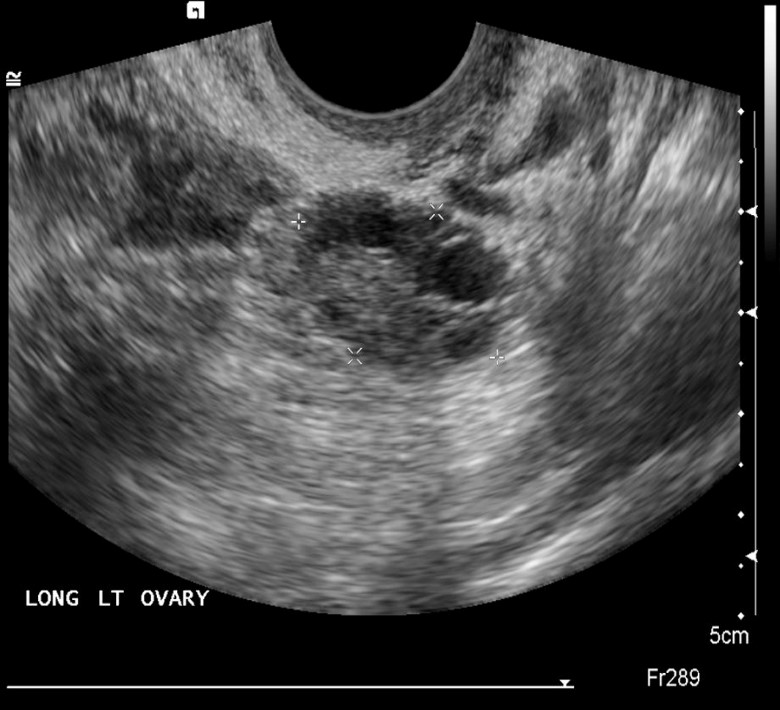
Figure 1: US of left ovary with multiple cysts.
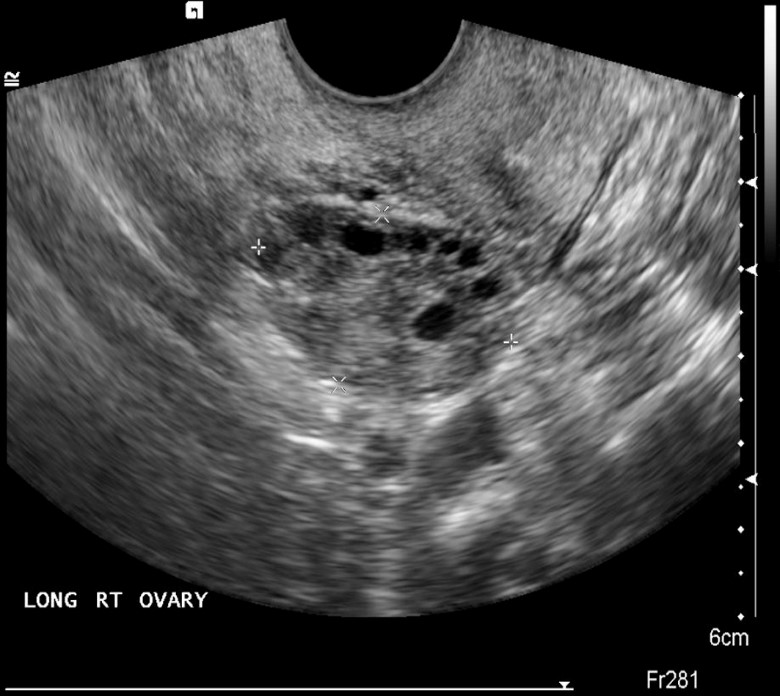
Figure 2: US of right ovary with multiple cysts.
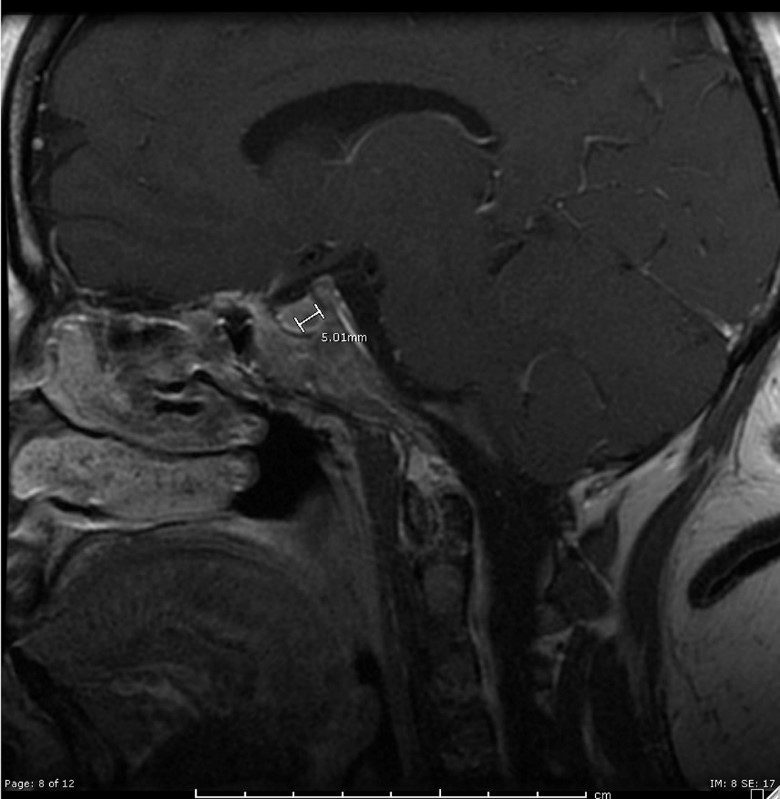
Figure3: Pituitary MRI, sagittal view.

Figure4: Pituitary MRI, coronal view.
Citation: Mohan V (2019)A Misdiagnosed Case of PCOS: Cushing's Disease. Ann Med &Surg Case Rep: AMSCR: 100010