Annals of Medical & Surgical Case Reports
Case Report
Ovarian Cancer or Pancreatic Metastasis? A Challenge for the Pathologist
Sarma D1*, Bickley M1, Salmons N2 and Curran F2
1Sandwell and West Birmingham NHS Trust, UK
2Royal Wolverhampton NHS Trust, UK
*Corresponding author: Diwakarryali Sarma, Sandwell and West Birmingham NHS Trust, UK, Tel: +447572370317; Email: diwakar.sarma@nhs.net
Citation: Sarma D, Bickley M, Solomon N and Curran F (2019) Ovarian Cancer or Pancreatic Metastasis? A Challenge for the Pathologist. Ann Med & Surg Case Rep: AMSCR-1000016.
Received date:20 August, 2019; Accepted date: 26 August, 2019; Published date: 03 September, 2019
Abstract
Introduction: Primary mucinous carcinoma of the ovary is very rare. We present a diagnostic dilemma in a patient with a large ovarian tumour who also had a para-aortic mass on CT imaging.
Background: Pancreatic and other upper GI cancers can metastasise to the ovary whilst primary ovarian cancers may demonstrate intestinal differentiation. A number of methods have been described for differentiating between the two sources but they do not account for every presentation. There can still be uncertainty in determining tumour origin.
Aim: We used a combination of previously described algorithms in an attempt to determine the origin of our patient’s cancer.
Conclusions: Despite utilising several methods, we were unable to decide with certainty the precise site of origin of this cancer. We conclude that further research is needed to enable accurate classification of these tumours.
Keywords: Metastatic cancer; Ovarian malignancy; Pancreatic cancer; Palliation
Case Report
A 70-year-old lady presented via the gynaecology fast track clinic with a two-month history of excessive vaginal discharge. She also complained of bloating, abdominal discomfort and anorexia for 18 months. There had been two stone unintentional weight loss over 16 weeks. She recalled one episode of post-coital per-vaginal bleeding 12 months previously. She had been vomiting for three days. Medical history included a right oophorectomy for a benign ovarian cyst 40 years earlier, a right hip replacement, hypertension and gastritis [1].
On examination, she was cachectic and dehydrated with a distended tender abdomen. Bowel obstruction was suspected. On bimanual examination, a mass was palpable in the pouch of Douglas. She was treated with intravenous fluids, nasogastric aspiration and analgesia [2].
Ultrasound scan showed an 11.0 × 6.5 × 9.5cm multicystic lesion in the left adnexa of varying echogenicity, along with a small amount of free fluid. CT scan showed a 12.0 × 12.0 × 9.1cm multicystic pelvic mass posterior to the uterus, which was compressing and displacing the rectosigmoid to the left (Figure 1). Also noted was a 4.0 × 3.3cm irregular para-aortic nodal mass in the superior abdomen. Gynaecology MDT discussion concluded that the ovarian mass was unsuitable for primary debulking and that she should undergo chemotherapy prior to resection. An opinion was requested from the upper GI MDT regarding the para-aortic mass. In contrast to the gynaecology opinion, the upper GI MDT thought the patient may have had a pancreatic tumour with local node involvement, invasion of the jejunum and a metastasis in the ovary [3].
An ultrasound guided transvaginal parasacral biopsy of the pelvic mass was taken, revealing the lesion to be mainly cystic in nature with very little solid component. During this period, there was on-going vomiting and high nasogastric aspirates. Parenteral nutrition was commenced. She subsequently underwent palliative gastrojejunostomy, drainage of ascites, mesenteric biopsy, and left oophorectomy. Following this, she was able to maintain an adequate oral intake [4].
Histology of the resected ovary showed a well-to-moderately differentiated mucinous adenocarcinoma (Figure 3A-C). The mesenteric biopsy consisted offibroconnective tissue, extensively infiltrated by a moderately differentiated adenocarcinoma, with loss of mucinous differentiation compared to that found in the ovarian tumour. The samples were positive for CK7, CK20, PR, and CDX-2, but were PA × 8, Ca125, and ER negative. Staining was later performed for Ca19-9 which showed patchy positivity throughout. After further MDT discussion it was agreed that her presenting symptoms were more in keeping with ovarian than pancreatic malignancy. Outpatient chemotherapy appropriate for ovarian carcinoma (carboplatin, taxol) was commenced but her condition rapidly deteriorated. She died during the first treatment cycle [5].
Discussion
Differentiation between a primary mucinous ovarian malignancy and an extra-ovarian primary with metastasis to the ovary, has long been something of a dark art. Histologically, cancers of the upper GI tract can appear very similar to primary mucinous ovarian tumours; this can pose a challenge when considering which treatments to initiate. Over the years, various authors have suggested algorithms to determine the origin of these tumours using size and laterality of the ovarian mass (Table 1).
The resected ovary was described in the pathological report to be 10.5 × 9.0 × 6.0 cm with defects in the capsule (Figure 2), and a multiloculated cystic structure (Figure 2). Immunohistochemistry showed positive staining for markers favouring intestinal differentiation. Ca19-9, positive in places within the ovarian mass (Figure 3D).
Despite the immune histochemical profile favouring pancreatic metastasis, it was not possible to definitively differentiate between primary ovarian adenocarcinoma showing intestinal differentiation which can recapitulate all the same immune histochemical markers, or metastasis from an upper GI tract origin based on histology alone. The 18-month history of symptoms favoured an ovarian origin with the pancreatic involvement being secondary to invasion via an affected lymph node. Therefore, the final MDT decision was to treat this patient for a primary ovarian cancer.
Conclusion
The final oncological decision was to treat it as a primary ovarian cancer with invasion of the pancreas via an affected lymph node. We conclude that further research is needed to enable accurate classification of these tumours.
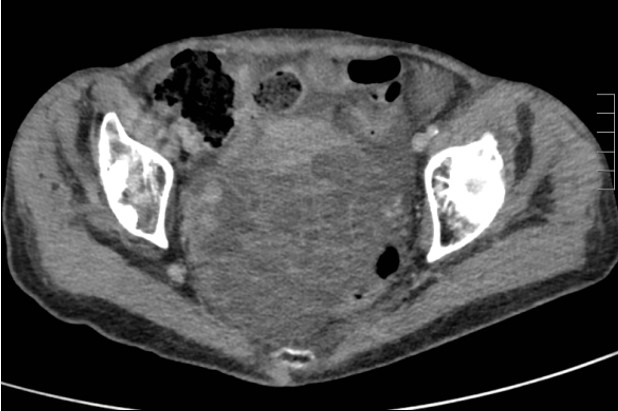
Figure 1: A 12 × 12 × 9.1cm multicystic pelvic mass with enhancing septations.

Figure 2: Macro photo (unopened specimen) with disrupted capsular surface of ovarian mass.
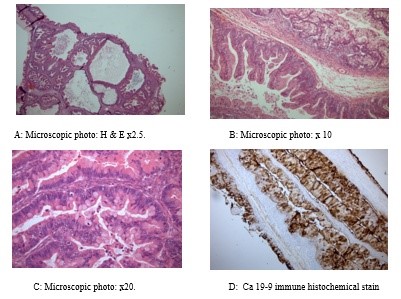
Figure 3: Histology of ovarian specimen
|
Author name |
Ovarian |
Metastatic |
|
Seidman, et al. |
Unilateral >10cm |
Bilateral or unilateral <10cm |
|
Yemelyanova, et al. |
Unilateral >13cm |
Bilateral or unilateral <13cm |
|
Hu, et al. |
Unilateral >10cm PA × 8 positive |
Bilateral or unilateral <10cm PA × 8 negative |
Table 1: Over the years, various authors have suggested algorithms to determine the origin of these tumours using size and laterality of the ovarian mass.
Citation: Sarma D, Bickley M, Salmons N and Curran F (2019) Ovarian Cancer or Pancreatic Metastasis? A Challenge for the Pathologist. Ann Med & Surg Case Rep: AMSCR-1000016.