Journal of Obstetrics and Gynecological Problems
Case Report
Uterus didelphys in pregnancy: Case report
Silva, JMM 1*, Mendonca, DP 2, Silva, LHFM 3, Sousa, LFPA 4, Cortes, LS 5.
1Department of Gynecology and Obstetrics, University of Brasilia, Darcy Ribeiro University Campus. Email: drjoaomarcosmeneses@ hotmail.com
2Department of Gynecology and Obstetrics, Paranoa Regional Hospital. Email: denisepdm@yahoo.com.br
3Department of Gynecology and Obstetrics, University of Brasilia, Darcy Ribeiro University Campus. Email: draligiahelena@hotmail. com
4 Department of Gynecology and Obstetrics, Fertilcare Human Reproduction Clinic. Email: lucianapotiguara@gmail.com
5 Department of Gynecology and Obstetrics, Paranoa Regional Hospital. Email: lucianasegurado@yahoo.com.br
*Corresponding author: Silva JMM, Department of Gynecology and Obstetrics, University of Brasilia, Darcy Ribeiro University Campus 70910 900 Brasilia, Brazil, Tel: +556133072028; Fax: +556133403385; Email: drjoaomarcosmeneses@hotmail.com
Citation: Silva JMM and Mendonça DP (2019) Uterus Didelphys in Pregnancy: Case Report. J Obstet Gynecol Probl: JOGP-100004.
Received date: 21 August, 2019; Accepted date: 28 August, 2019; Published date: 03 September, 2019
Introduction
Uterine malformations are secondary failure of development, resorption or fusion of Müllerian ducts, whose prevalence is 5-6%.
Failure of Muller ducts to fuse during embryonic development can result in a broad spectrum of malformations of the female reproductive tract, ranging from slight variation in the shape of the uterus to complete absence or duplication of the uterus, cervix and vagina. Müllerian duct anomalies have been associated with increased risk of infertility, loss of pregnancy and adverse pregnancy outcomes, depending on the extent of the abnormality [1].
The European Society for Human Reproduction and Embryology and the European Society for Gynecological Endoscopy (ESHRE / ESGE) proposed a new classification of uterine malformations in 2013, which explains variations in the cervix and vaginal anatomy [2].
When complete failure of Müllerian ducts fusion occurs, an anomaly called uterus didelphys originates, with each uterus receiving only oneuterine tube.
Uterus didelphys is one of the least common anomalies, estimated at 1 in 1000 women, and is classically defined as the presence of two uterus, two cervix, with or without a longitudinal vaginal septum, although there are other variations [1,3].
Congenital anomalies includes septate uterus, bicornuate uterus, unicorn uterus, arched uterus, uterus didelphys, or T-shaped uterus.
Uterus didelphys represents 26% of cases of malformations and the septate uterus seems to be the most frequent anomaly with 30 to 50%.
It is important to identify the anomaly presented by the patient in order to understand the impact on their reproductive health.
Case Report
Patient 25 years old, first pregnancy, gestational age of 39 weeks and 6 days, white race, from Paranoá.
Complaint: Frequent contractions of moderate intensity.
Physical examination: normal uterine tone, uterus dinamics: 1/25’/ 10’. Fetal heart beat: 140 bpm, fetal movement present.
Transvaginal ultrasound: presence of two cérvix, the left one being prominent. Both posterior and imperibles.
Way of delivery: Caesarean section (patient’s wish and suspected Mullerian malformation) on 11/30/18;
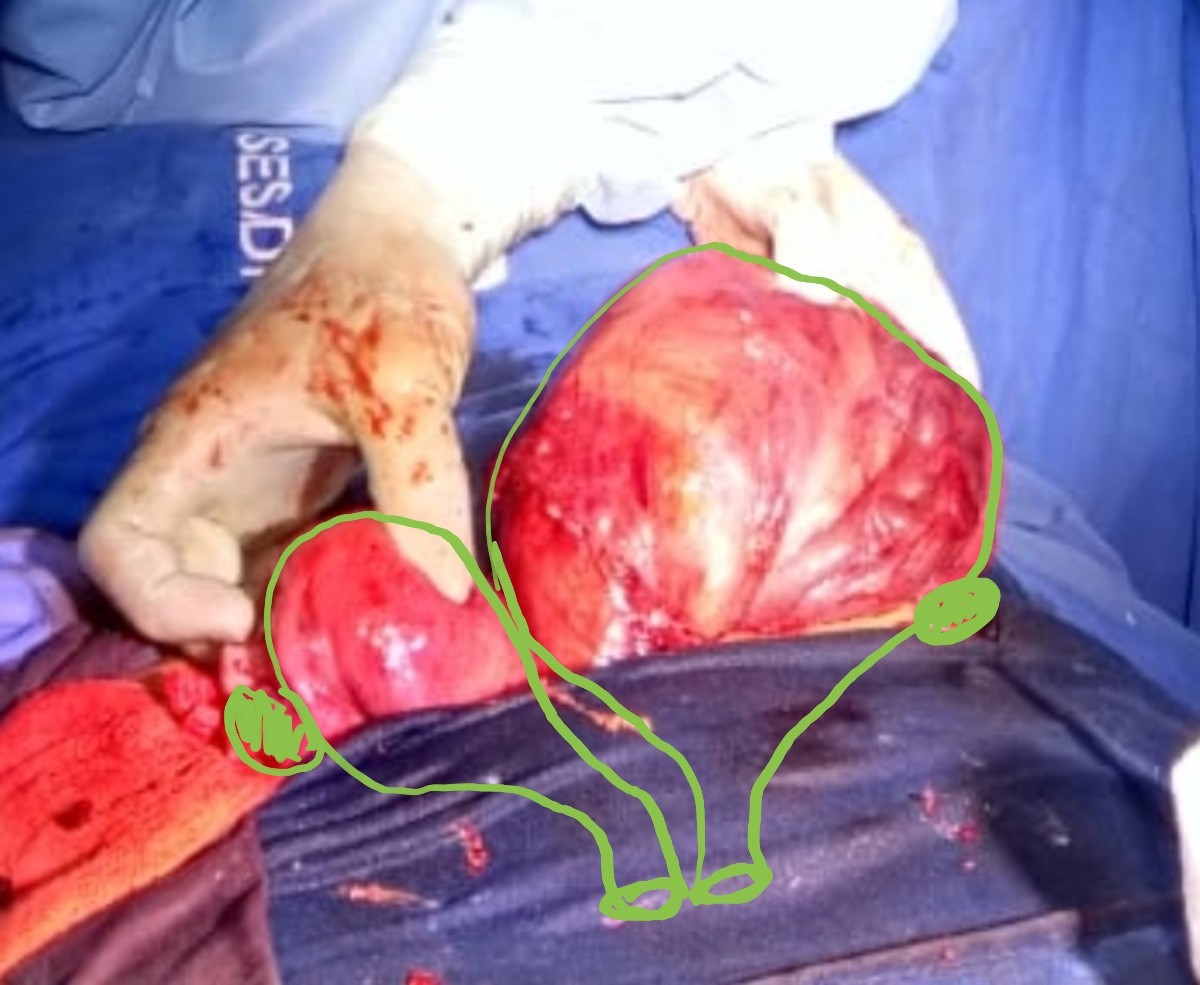
Surgical act: two uterine bodies: gestational left and right with normal dimensions, two tubes, one from each uterine body. Newborn born alive, female, weight: 3245g, apgar: 9/10.
Patient had good reponse in the postoperative period. Hospital discharge on 12/02/2018.
Discussion
Uterus didelphys is an abnormality that accounts for 26% of uterine malformations, but the exact incidence of these malforma- tions is uncertain.
Diagnosis of Muller duct anomalies is not always easily dis- cernible and may require the use of multiple image detection tech- niques or more invasive procedures such as hysterosalpingogra- phy, hysteroscopy, laparoscopy or laparotomy. In addition, uterine abnormalities that do not belong to any of the traditional ASRM classifications, such as uterus didelphys with one cervix, have been reported. More recently, three-dimensional and mutliplanar ultrasound has been used as a noninvasive method to determine uterine anatomy with accurate results [1-4].
These findings are uncommon in clinical gynaecology. These situations reflects the wide variety of presentation and most malformations are not diagnosed before a pregnancy or only diag- nosed after the manifestation of an obstetric problem.
Uterine malformations are responsible for 15% of second trimester gestational losses and are associated with anomalous fe- tal presentation, PPD and IUGR. Spontaneous or elective prematu- rity occurs in 25 to 50% of uterine malformation cases.
Structural changes in the uterus may increase obstetric mor- bidity, causing placental retention, uterine underinvolution, and hemorrhage, generating gynecological complaints including oli- gomenorrhea, dysmenorrhea, dysfunctional uterine bleeding, and dyspareunias.
Despite having a high probability of obstetric complications, the case evolved to an uneventful and term pregnancy.

Citation: Silva JMM and Mendonça DP (2019) Uterus Didelphys in Pregnancy: Case Report. J Obstet Gynecol Probl: JOGP-100004.