Journal of Obstetrics and Gynecological Problems
Review of Literature
The Validity of Ultrasound in Diagnosis Ovarian Masses
Yasamin Hadi Younis, Abeda Ahmed Hamdoon* and Heba Zaid Mohamed
Department of Radiology, Al-Khansaa Teaching Hospital, Iraq
*Corresponding author: Abeda Ahmad Hamdoon, Department of Radiology, Al-Khansaa Teaching Hospital, Iraq, Tel: +9647719338241; Email: abeda.ahmad@yahoo.com
Citation: Abeda Ahmed Hamdoon, Yasamin Hadi Younis, Heba Zaid Mohamed (2019) The Validty of Ultrasound in Diagnosis Ovarian Masses. J Obstet Gynecol Probl: JOGP 100005.
Received date: 16 September, 2019; Accepted date: 10 October, 2019; Published date: 21 October, 2019
Abstract
A total of 200 women examined by sonography detected an ovarian mass 50 of them show spontaneous resolution the reminder 150 women with persist ovarian masses [140] of them under went operation the histopathological result correlate with sonographic morphology found 64.3% are non-neoplastic masses and the most frequent masses are physiological cyst while 35.7% are neoplastic masses 77.7% of these masses are benign tumor and the remainder are malignant The most frequent benign tumor are serous cyst adenoma 28% followed by benign cystic teratoma 18%. Sonography is a valid procedure in the evaluation of ovarian mass and capable in predicting benign lesion with reasonable confidence but the prediction of malignancy is less reliable.
Keywords: Non-neoplastic; Ovarian mass; Tumor
Content
Introduction and review of literatures
Ultra sound screening is a useful diagnostic aid for detecting of ovarian mass [1-5]. Large compendium deals with the overlap in appearance of neoplastic and non-neoplastic mass and sonography can't distinguish malignant from benign neoplastic but give useful information and straight forward observation which can greatly assist the gynecologist in deciding whether surgery indicated so solid mass virtually ensures that an ovarian lesion is neoplastic however solid ovarian mass extremely uncommon [6-10]. But the picture of cystic mass gives a diagnostic problem. This was confused with physiological cystic changes of follicular system or that due to a benign lesion, infection, endometriosis or ovarian pregnancy [11-15].
Ovarian cancer is an alarming disease and a leading cause of death from gynecological malignancy with five survival rate of 31% [16-20]. This poor survival rate needs significant improvement in screening for early detection and dramatic increases in survival [21-25].
The best prognosis of ovarian cancer obtained when the disease confined to the ovaries than in more advanced stages [26-30].
The best prognosis of ovarian cancer obtained when the disease confined to the ovaries than in more advanced stages [31-38].
Anatomy of ovaries: The ovaries are oval, flattened, compressible organs, approximately 3 by 2 cm in size. The normal ovary located lateral to the uterus and fallopian tubes medial to the ovarian vessels and obturator internus muscle and facing superiorly to the levator ani muscle and anteriorly to the internal iliac vessels and ureter. The ovarian artery arises from the abdominal aorta just below the renal artery [39-45]. The ovarian vein begins on each side in the panpiniform plexus which lies between the layers of the broad ligament. Lymphatic drainage, the ovaries have plexus of vessels which drain along the infundibulum pelvic fold to the Para-aortic nodes on both sides of the mid line. On the left these are found around the left renal pedicle. While on the right may be only on node before the lymph flows into thoracic ducts thus rapid early speed of metastatic carcinoma to distant sites [46,47].
Microscopically: The normal ovary consists of an outer germinal epithelium inside which is the mass of stoma embedded in this is the element of the Graffian follicle and corpora lutea consisting of granulosa cells, luteinized cells and theca cells as well as ova [43, 48-50].
Classification of Ovarian Masses
Non Neoplastic (cystic)
Neoplastic ovarian mass
Symptomatology
Evaluation of ovarian mass: The purpose of this study is to analyze those sonographic features of ovarian masses that may help to avoid the surgeon's hand as far as possible, in patients who very likely have benign self-limiting masses. The sonographic appearance of ovarian masses is only one factor that may influence subsequent management. A key issue is symptomatology e.g. Two lesion of identical size and morphology are found in women with sever symptomatology related to the mass, the other is a symptomatic woman surgical excision in favor in patient who acutely symptom. Hormonal status of patient may influence management identical appearing mass found in pre-menopausal & post-menopausal women likely to be agreed with different clinical finding. Sonography has its major benefit when clinical features have not already made the decision in the surgeon's mind [41].
Epidemiology: Ovarian tumor is insidious disease [44], both incidence and death rate from ovarian cancer are on the increase in all countries. During the last 50 years the death rate from ovarian cancer has doubled (office of pop censuses and survey 1981) were as the frequency of diagnosis has increased [12].
Geographic Variation: Ovarian tumor occurs primarily in highly industrialized countries of the world. Sweden has highest death rate in excess of 21 per 100,000 of the population, Denmark, England, USA, Followed Japan less than five per 100000 and low rate in Cuba [27].
Age and social class: Age incidence with age up to the 6th decade. In young benign mass five times more than malignant. More prevalent amongst higher social classes [12].
Asbestos exposure and talc particle
Which is found in soap ponder and deodorants and packaging of condoms and contraceptive diaphragm.
Parity: Ovarian cancer which is less common in women of high parity and pregnancy would be protective (Table ll) [8].
Davidl Manneh
Genetic Factor: Ovarian tumor occurs in, women with strong genetic predisposition [36]. Prodenetal (1989) found high risk families can be defined as those with tumor more close relative affected [12]. Familial ovarian cancer can increase in infrequency [33].
Radiation: Ionizing radiation is carcinogenic [12].
Oral contraceptive pills: Progesterone oral contraceptive pill increase risk of developing functional ovarian cyst. Ovarian abscess associated with I.U.C.D [10,49] often ovarian cancer does not present clinically until the advanced stage and is the first cause of death from gynecological malignancy [16]. In past the presence of any cystic adnexal mass in post-menopausal women was an indication for surgical exploration. Therefore, serial ultrasound follows up without surgical intervention may play a role in the clinical management of such patient.
Review of ultrasonography: Conventional ultrasonic trans-abdominal evaluation of the female pelvis uses a suprapubic approach through a distended urinary bladder. This performed in the past with static sagittal and horizontal images at 1 to 2 cm intervals (B-mode ultrasonography) but this has been largely replaced by real time imaging to allow of inner discrimination of the pelvic structure. Trans-abdominal ultrasonography instrument includes 2.5 to 5 MHz linear array transducer of moderately high frequency typical finding with such system includes adnexal content and presence of ovarian cystic components. Sunden first described the ability to visualize ovarian pathologic characteristics with trans-abdominal ultrasonography 1964, but early sonographer had difficulty distinguishing malignant from benign ovarian cystic masses real time Trans abdominal ultrasonography was correlated with morphologic characteristic and size by Camp belletal in 1982 after which the application of Trans abdominal, ultrasonography for adnexal abnormality began [7].
By mid-1980 report of earl ultrasonography detection of ovarian cancer were seen and they reported in 1989 that ovarian cancer was the fifth leading cause of death in 35-54 rears age range and the fourth leading cause of death in 55-74 years’ age range [45]. The predominant indication of benignity on Trans abdominal ultrasonography was the appearance of a small cyst but Luxman found (2) of (33) Simple cyst <5 in diameter contain malignant ovarian tumor [7].
Ultrasonography of Normal ovary: The ovaries are intra peritoneal structure slung between the lateral pelvic walls, by the suspensory ligament. The result of these attachments is that the ovary is free to swing between the ovarian fossa on the pelvis side wall and the pouch of Douglas [41]. The normal ovary is a uniformly hypoechoic structure, ovoid in shape with a smooth echogenic outline [7]. The adult ovary measure’s 2.5 to 5.0 cm long, 1.5 to 3 cm wide and 0.6 to 1.5 cm thick.
Cohen and colleagues: Measured ovarian volume in menstruating subject ovarian volume was 9.8 cm3 for premenarchal girls was 3.0 cm3 and of post-menopausal patient was 5.8cm3. The ovarian size peaks in the 3rd decade and decline through menopause. A varying number of maturating follicles will be visible as small cystic structures within the ovaries [17].
Trans-vaginal ultrasonography: Using endo-vaginal probes of higher frequency (6.5 to 7.5 MHz) allows much finer discrimination of architecture of the ovary and uterus than that found with trans abdominal ultrasonography and it is performed in empty bladder [17]. High frequency Trans-vaginal ultrasonography can be said to improve characterization of the size and morphological characteristics of the ovaries with better sensitivity that offered by Trans-abdominal ultrasonography.
Doppler evaluation of ovarian mass: There is increasing interest in the Doppler evaluation of ovarian masses to determine whether the lesion is benign or malignant [19]. Ovarian carcinomas are vascular. Tumor angiogenesis result in proliferation of sinusoidal type vessels that lack smooth muscle in the vessel wall result in a law-resistance vascular network. That can be analyzed, with color Doppler imaging and Doppler wave form analysis [41].
Transvaginal color flow imaging: The women had empty bladder and scanned in Lithotomy position with slight reverse trendelenburge tilt to localize free fluid in pouch of Douglas. Premenopausal women scanned during 1 to 8 of menstrual cycle. The ovaries assessed located above the internal iliac vessels, which appear as anechoic Tubular structures with echogenic wall. Ovarian morphology and size, and examined for prominent area of vascularization. These vessels appeared as continuously fluctuating color rather than pulsatile color seen with normal arteries.
Pulsatility index: Is a measure of the impedance to blood flow, a low value indicating decreased impedance and high value increased impedance to blood flow. In normal ovaries high values while in malignancy a low value. Problems arise because inflammatory masses and cropusluteum cyst also demonstrate low resistance to flow as measured by Doppler wave form analysis [45].
Sonographic appearance of different ovarian masses
Follicular ovarian cyst: A well circumscribed thin-walled unilocular cyst usually unilateral occasionally bilateral. Scanning on the other time will demonstrate changes in their appearance or disappearance, if the cyst rupture internal echoes within the cyst occur, free fluid may be seen in Cul-de-sac the finding of an ovarian mass and free fluid mimic ectopic pregnancy and PID [36].
Corpus luteum cyst: Thin wall unilocular and usually unilateral. Hemorrhage into cyst is frequent so there is wall irregularity and variable amount of internal debris even fluid depress level some time the cyst entirely filled with echoes stimulate a solid mass. Rupture of cyst and fluid in Douglas pouch simulate ectopic pregnancy [36].
Theca lutein cyst: Multilocular thin wall, frequently huge associated finding in ovarian hyper stimulation syndrome include ascites, pleural effusion.
Endometriosis (chocolate cyst): Well-circumscribed cyst with slightly thickened wall and uniformly dispersed low level internal echoes. Sometime found echoes in depended portion of cyst or peripherally fluid-debris levels can be demonstrated [4], or they appear as purely cystic mass or containing septation [2]. The presence of round homogenous cyst with low level echoes considered as sonographic diagnosis of ovarian endometriosis [30]. Endometrioma may be bilateral or multiple.
Inflammatory ovarian mass (tubo-ovarian abscess): An echoic masses thick irregular wall and may contain irregular septa, low level echoes tend to layer as clumps of echogenic material.
Ovarian pregnancy (ectopic pregnancy): Diagnosis of ectopic pregnancy based on sonographic visualization of an ectopic gestational sac and of adnexal mass with mixed sonographic pattern with or without free fluid in pouch of Douglas. Pseudo gestational sac that is sonolucent structure resemble gestational sac with or without well-defined border [3].
Poly cystic ovary: Symmetrical bi lateral ovarian enlargement with multiple cysts rang 2-6 mm [30]. or may be uniform in size arrange along the periphery of the ovary unilateral poly cystic ovary can be recognized [13,32].
Neoplastic Ovarian Masses: The diagnosis by ultra sound feature analysis is 80-90% accurate in distinguishing benign from malignant (Table III) [10]. Malignant ovarian carcinoma is the main cause of gynecological cancer death [26].
Serous tumor: 40% of ovarian tumor serous in origin and 50-70% of these are benign serous cyst adenoma and bilateral in 50% of cases.
Sonographicaly: Serous cyst adenoma is large thin walled cystic masses usually unilocular but may contain thin septation. Lobulation of external contour is infrequent. Ascites is uncommon. Serous cyst adenocarcinomas usually multilocular cyst containing papillary projection from the cyst wall and septae(1).Solid material may fill entire loculation neoplastic extension to surrounding organs resulting in fixation of the mass, ascites and abdominal carcinomatosis.
Mucinous tumors: Less frequent than serous and its bilateral in 5% of patients. Mucinous cyst adenoma is frequently massive, internal septa is frequently encountered than in serous cystadenoma and may form a complex pattern. Low level echoes representing mucin maybe seen. Rupture of the cyst gives rise to intraperitoneal spread.
Sonographicaly: Mucinous cyst adeno-carcinoma large multilocular cystic masses containing solid material. Irregularity of the wall and pelvic fixation.
Endometroid carcinoma: Cystic mass with papillary projection or solid with area of necrosis and hemorrhage [24].
Clear cell carcinoma: Sonography nonspecific complex mass with either cystic or solid component pre dominating.
Brenner tumor: Usual sonographic feature echogenic mass contains small cystic spaces.
Germ cell tumor: Approximately 15% of all ovarian rumor are of germ cell variety and of these 95-98% are benign cystic teratoma (dermoids) [20]. Majority of teratoma occur as asymptomatic ovarian mass occasionally will rupture and produce peritoneal reaction.
Cystic teratoma (Dermoid cyst) Sonographicaly: Cystic teratoma does not have predilection for either ovary and bilateral in 8-15% of cases [21, 39]. It is cystic mass containing an echogenic focus that exhibits post acoustic shadowing [2]. Hair is very reflective and responsible for acoustic shadowing is a sonographic marker of ovarian teratoma Shadowing in dermoids also occurs posterior to bone or teeth but in these cases there is a strong echogenicity [1].
Other categories of sonographic presentation of teratoma
Dysgerminoma: Sonographicaly the mass is predominant echogenic with small cystic area of hemorrhage or necrosis.
Endodermal sinus tumor: Is the second most common malignant germ cell tumor occurring primarily in child and young adult [23]. Most ovarian neoplasms associated with pregnancy are benign, but ovarian malignancy occurring in associated with pregnancy is rare [29]. Sonographically is solid mass with cystic spaces due to hemorrhage or necrosis.
Granulosa cell tumor: Is most common in post-menopausal women. The tumor appears as a solid mass unilateral and if large have multi loculated cystic appearances simulated cyst adenoma [36].
Fibroma: Common in menopausal & post-menopausal age group bilateral in 4-8% of patients [36]. Sonography solid mass contains an area of cystic necrosis and hemorrhage· some cases areas of acoustic shadow ate due to calcification.
Lymphoma: Usually bilateral due to dissemination from extra genital sites. Sonography the mass solid hypoechoic in appearance.
Metastatic Tumor Kruken berg tumor: Usually bilateral either genital origin or extra genital sites includes in (stomach and colon) and the Breast [25]. Metastatic carcinoid to the ovary always bilateral.
Sonographically: The mass is solid with cystic areas of necrosis and hemorrhage or multilocular cystic mass [25].
The validity of ultrasound in the diagnosis of ovarian masses
Objective: To assess the validity of trans-abdominal sonography in the diagnosis of different ovarian masses.???????
Settings: Gynecological and obstetric department of Al-batool hospital in Mosul city.
Patient and method: From July 1998 to April 1999 a prospective study of 200 women aged between 20-60-year-old, the mean age (35 years), who attained the hospital with clinical manifestation of amenorrhea, menorrhagia, abdominal pain and pelvic examination is done for them by a good gynecologist who referred them to sonographic screening. Trans-abdominal ultrasonography is performed with a full bladder using a standard technique with a real time sector ultrasound. The sonogram device which used in the examination is Simons with probe 5 MHz.
The examination is done by a good radiologist and sonographic section of both ovaries obtained in transverse and sagittal planes and good observation for the ovarian mass is done measuring its size by both dimension and look very well for its echogenic pattern, also good observation for adjacent structure to show associated spread and whether ascites present or not.
Follow up the patient was done and repeating the scan with 3-4 WK interval and evaluating the lesion whether regress or increase in size. Those women with persistent ovarian mass, who underwent laparotomy the ultra sound morphological characteristic compared with sub sequent histopathological result.
Result: A total of 200 women trans-abdominal ultrasonography were performed for them reveal the presence of an ovarian mass in one or both ovaries. Follow up after 3-4 WK repeats the scan 50 women who have sonographic appearance of cystic mocular mass in the first scan show in the 2nd scan spontaneous regression in size and resolution the remaining 150 women, the mass persists or even increases in size. 140 women of these underwent laparotomy and subsequent histopathological finding which are compared with sonographic finding and revea1 90 women had a non-neoplastic mass while 50 women showing a neoplastic mass.
The morphological sonographic features of each mass with histopathological finding are demonstrated in Table IV-VII.
In correlation of sonographic pattern and a physical examination found that anon-neoplastic masses are frequently seen in menstruating women. But may be seen in post-menopausal women as well. Also it is found the most non neoplastic masses are follicular cysts.
The distribution by age and menstrual status of 200 women examination by trans-abdominal sonogram the distribution of finding 140 women who subsequently underwent operation. A post-operation histopathological result of 140 women in correlation with sonographic finding found a non-neoplastic masses occurrence is 35.7% in Table VIII demonstrate a different neoplastic masses and its occurrence.
A&B tow trans abdominal sonograms of a cystic teratoma. This lesion is small and dose not deform the outer contour of the ovary. The sonographic hollmarks of this lesion (bright echose and shadowing echodensities (arrow). A diagnosis ca be made with confidence.
The distribution of benign serous cyst adenoma according to the age. In the study found a benign neoplasm is the most common neoplasm encountered than malignant.
A&B two trans abdominal sonograms of a solid ovarian mass with our usual differential diagnosis including ovarian carcinoma bremer tumor ovarian fibroma. The mass was a proved ovarian carcinoma.
Discussion
Ultra sonography is superior to the clinical examination and the method of choice in the evaluation of suspected ovarian masses because of the availability and ease obtaining image in several planes [11]. Sonography can reliably identify and differentiate cystic and solid lesion [15]. Most adnexal masses detected by sonography are physiological cysts and recognized by characteristic morphology and changes over time even spontaneous resolution [5]. In our study of 200 women with ovarian masses a non-neoplastic physiological cyst are the most common pathological masses to occur in the ovary and frequently seen in menstruating women but may be seen in post-menopausal women and most of them resolve spontaneously.
The most likely appearance of an ovarian mass will be to identify a thin walled unilocular cyst, the identification of unilocularity important implication for subsequent management.
A unilocular cystic mass is almost universally benign [41]. Hurwitz and associates reported on 52 unilocular cysts in women of all ages. There was no malignancy. Herman and coworker reported on 58 purely cystic neoplasm examination Sonographicaly 10 masses greater than 10 cm in size one of them was malignant. In our study of 60 women it is shown that sonographic appearance of unilocular thin wall cystic masses from which eleven of them proved to be a benign tumor. Morphological criteria alone such as mural modularity, internal echoes or thick septa allow for high sensitive (91 to 100%) although not very specific diagnosis of malignant masses in this study found some cases of sonographic appearance mixed echogenic pattern with thick septa simulate a neoplastic mass but on follow up either the mass disappear or the mass persist and the post-operative histopathological finding reveal a non-neoplastic masses. For distinguishing between benign and malignant ovarian neoplasm sonography is sensitive bur not specific [9].
Approximately 80% of ovarian tumor are benign and the remainder are malignant. In this study of 50 women proved to be neoplastic masses 77.7% are benign and the remainders 22.3% are malignant as shown in table X. In this study benign teratoma and serous cyst adenoma are the most frequent benign tumor. Also in the study of Roy a filly the occurrence of benign teratoma approximately of 15% of all neoplastic masses while serous tumor about 25%. In this study of HB. MEIRE the occurrence of benign teratoma about 15% while serous cyst adenoma 22.5% but the study of Gove and Hertig A.T. the occurrence of teratoma about 18% while serous tumor about 26.6%. In the study of Harilat K.R. and Thanagane the occurrence of teratoma about 18.7 while serous about 20 % [52]. From these 200 women examined, the most frequent malignant ovarian neoplastic detected is serous cyst adenocarcinoma and dysgerminoa which the most frequent in post-menopausal women with large size ovarian masses.
In the study of Roy A. filly serous adenocarcinoma occurrence 4.8% while dysgerminoa about 7% for all ovarian tumor. The same frequency found in the study of H.B. MEIRE were serous cyst adenocarcinoma occurrence 4% while dysgerminoa about 4.5%.
Gove and Hertig study found serous cyst adenocarcinoma about 3.6% while dysgerminoa about 4%. In the study of occur of serous adenocarcinoma about 4.5%. While dysgerminoa 4%.
In the study of Roy, a filly finds tumor more less than 5 cm 3% while tumor over 10 cm size about 16% in the study of H. B. MEIRE tumor of less than 5cm size its occurrence 1%. While 15% the tumor over 10cm in size. Also Gramer B.W. and Cutfer S.J. found tumor over 10 cm in size about 15% occurrences. The same frequency found in the study of Gove and Hertig, and the study as shown in Table XII.
Rulin and Preston found the larger the size of the lesion the higher likelihood of malignancy. The sensitivity and specificity of ultrasound in detecting of ovarian masses is 92% and 71% ultrasound is capable of predicting benign disease, with reasonable confidence but the prediction of malignancy is less reliable [35]. For distinguishing between benign and malignant neoplastic sonography is sensitive but not specific [40]. Trans-abdominal sonography not able to replace second look laparotomy in detection of minimal residual disease in ovarian cancer [41-45].
But vaginal sonography relatively simple test that can detect subtle changes in ovarian size and morphology. The uses of color Doppler and calculation of Resistance index (RI) can improve the specify in some cases [46-51]. In the present technique of trans-vaginal sonography and color Doppler image on measurement of blood flow velocity for distinguishing benign and malignant tumor of suspected adnexal origin improve the diagnostic accuracy and decrease the mortality rate [52].
Conclusion
This prospective study proved that sonography is a valid procedure and superior to physical examination in the evaluation of ovarian masses. Most of adnexal masses detected by sonography are non-neoplastic cyst and the most common are the physiological cysts which recognized by characteristic morphology and changing over time. Unilocular thin wall cystic mass is almost universally benign but some neoplastic mass can be recognized. Benign neoplastic mass occurrence 77.7% while the remainder is malignant.
Benign cystic teratoma and serous cyst adenoma are the most frequent neoplastic masses identified. In post-menopausal women the larger size of lesion the higher likelihood of malignancy. Trans-abdominal sonography is notable to detect minimal residual lesion. With the availability of trans-vaginal sonography and color Doppler image improve the diagnostic accuracy.
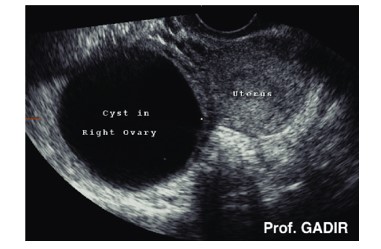
A) Aunilocular cystic.

B) After follow up the mass disappear and show normal ovary.
Figure I: Demonstrate a unilocular cystic mass which show complete resolution after follow up.
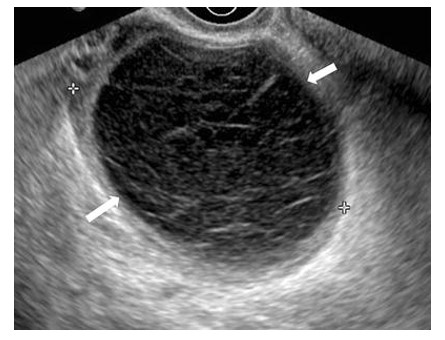
Figure II: ovarian mass with mild thickened wall. Numerous echoes are seen with the mass a small amount of free fluid is seen adjacent to the mass. note the flat margin (arrows) of the internal echoes this typical of layereal clotted blood. The lesion never excised and disappeared within 4WK. it was presumed to be carpus luteurn cyst.

A) Ovarian mass with septaion(arrow) overlap of serous cyst adenoma.

B) After follow up the mass show complete resolution and normal ovary.
Figure III: Small ovarian mass with spetation the mass over laps that of a serous cyst adenoma follow up show complete resolution and normal ovary.
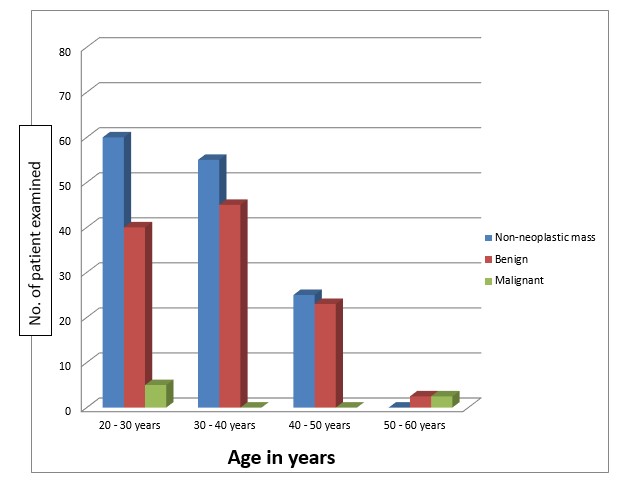
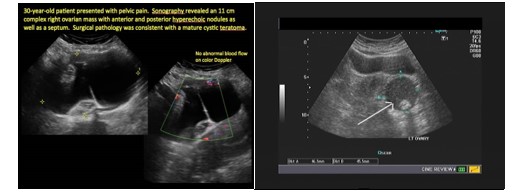
Figure IV: A and B tow sonogram of cystic teratma proved histological.

Figure V: Ovarian mass with septa which prove to be serouse cyst adenoma. This relative large mass (nearly 10 cm) demonstrates athin wall and two thin septa (arrows). This lesion was benign serous cyst adenoma.
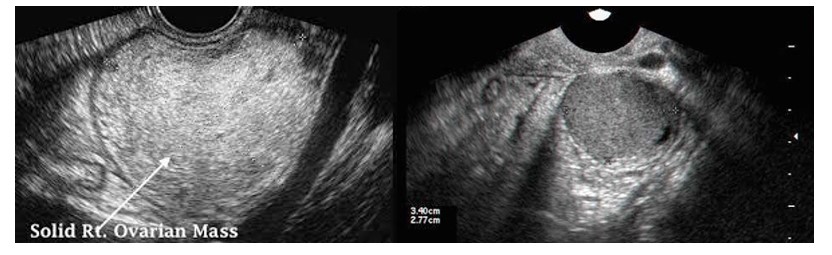
Figure VI: A&B tran abdominal sonogram of a large solid ovarian mass proved to be malignant ovarian mass.
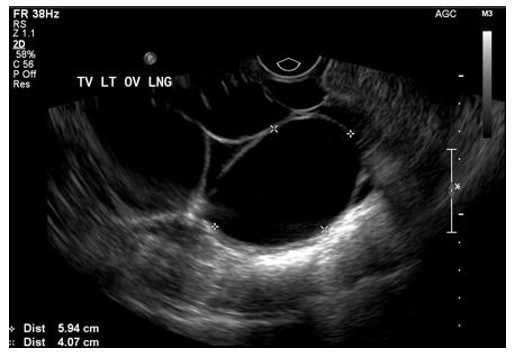
Figure V11: A cystic mass with septation and a large septal nodule (N) is seen. Such lesion highly of serous cyst adenocarcinoma.
|
Subject |
|
List of tables |
|
List of figures |
|
Abstract |
|
Introduction and review of literature |
|
Anatomy of ovaries |
|
Microscopically |
|
Classification of ovarian masses |
|
Symptomology |
|
Epidemiology |
|
Review of sonography |
|
Sonograph of normal ovaries |
|
Trans-vaginal ultrasound |
|
Doppler evaluation of ovarian masses |
|
Sonographic appearance of different ovarian masses |
|
Objective |
|
Setting |
|
Patient and method |
|
Result |
|
Discussion |
|
Conclusion |
|
References |
List of Figures
|
Figures |
Subject |
Pages |
|
I |
Unilocular cyst |
- |
|
II |
Ovarian mass with thick wall and numerous echoes. |
- |
|
|
after follow up 4 wk. later on the mass disappear the mass presumed to be corpus luteum |
- |
|
III |
A- Ovarian mass with septation overlap of serous cyst adenoma. |
- |
|
|
B- After follow up the mass show complete resolution and normal ovary |
- |
|
IV |
A and B two Sonograph of benign cystic teratoma proved histopathologically. |
- |
|
V |
Ovarian mass with septa which proved to be serous cyst adenoma/ |
- |
|
VI |
Trans abdominal Sonograph of a large solid ovarian mass proved to be malignant mass |
- |
|
VII |
Sonographic appearance of ovarian mass which proved to be serous cyst adenocarcinoma. |
- |
List of Tables
|
Table |
Subject |
|
I |
Ovarian tumor staging system (FIGO) |
|
II |
Characteristics of women who develop ovarian tumor |
|
III |
Ovarian tumor benign and malignant features |
|
IV |
Non-neoplastic masses(in 90 women) |
|
V |
Neoplastic masses(in 90 women) |
|
VI |
Unilocular cysts |
|
VII |
The distribution by age and menstrual status of 200 women examine by sonography and distribution of pathological finding in 140 women |
|
VIII |
Different neoplastic masses and it’s occurrence |
|
IX |
Distribution of benign serous cyst adenoma according to age |
|
X |
Ovarian neoplasm occurrence in relation to menstrual status. |
|
XI |
Ovarian tumor size and malignancy |
|
XII |
Comparison between our study and other studies |
|
Table I |
Ovarian tumor staging system FIGO |
|
Stage I |
Growth limited to the ovaries. |
|
Ia |
Growth limited to one ovary, no ascites |
|
i. |
No tumor on the external surface, capsule intact. |
|
ii. |
Tumor on the external surface |
|
Ib. |
Growth limited to both ovaries, no ascites |
|
i. |
No tumor on the external surface, capsule intact. |
|
ii. |
Tumor present on the external surface and or capsule(s) ruptured |
|
Stage II |
Tumor involving one or both ovaries with pelvic extension. |
|
IIa |
Extension and/or metastasis to the uterus and/0r tubes |
|
IIb |
Extension to other pelvic tissue including peritoneum and uterus |
|
IIc |
Staging IIa and IIb with ascites or positive peritoneum |
|
Stage III |
Tumor involving one or both ovaries with metastasis outside the pelvis and / or positive nodes. tumor limited to the pelvis with extension to small bowel |
|
Stage IV |
Tumor involving one or both ovaries with distant metastasis |
Table I: FIGO staging.
|
Primary Tumor |
|
Incidence |
Example |
|
|
I |
|
Epithelial |
65% to 75% |
Serous tumor mucinous tumor endometroid ca. clear cells ca. |
|
II |
|
Germ cell |
10% to 15% |
Teratoma dysgerminoa endo-dermal sinus tumor |
|
III |
|
Sex cord stromal |
5% |
Granulosa cells tumor sertolie leydig tumor the coma |
|
IV |
|
Connective tissue tumor |
5% |
Fibroma lymphoma |
|
V |
|
Metastatic |
10% |
Genital Adeno ca. of endometrium. Extra genital Stomach Colon Breast(36) |
|
Characteristic of women who develop ovarian tumor |
|
|
1 |
A lower mean of pregnancy. |
|
2 |
A large proportion never pregnant. |
|
3 |
A large proportion nulliparous. |
|
4 |
A large proportion of infertility and increased frequency of abortions compared to control. |
|
5 |
A later age at first pregnancy. |
|
6 |
Oral contraceptives. |
|
7 |
Breast carcinoma has twice the standard risk. |
|
8 |
No viral etiology has been suggested as a possible cause. |
|
9 |
Possible protective effect of mumps oopheritis in relationship to the lower incidence of ovarian cancer. |
|
10 |
There is hereditary (familial) factor in the development of ovarian cancer and type of transmission to be autosomal dominant. |
Table II: Ovarian cancer which is less common in women of high parity and pregnancy would be protective.
|
Ovarian Tumor |
|
|
Benign Features |
Malignant Features |
|
Size <10 cm Smooth wall |
Size <10 cm Irregular or poorly defined walls |
|
Unilocular cyst |
Complex cyst with solid component |
|
Multilocular with thin septa |
Debribinous |
|
No debris |
Ascites |
|
Mass effect only |
Metastatic nodules or nodes |
|
Mobile |
Fixation to pelvic side wall or omentum |
Table III: Malignant ovarian carcinoma is the main cause of gynecological cancer death.
|
Histopathological finding |
Sonographic morphology |
|||
|
Unilocular |
Multilocular thin septa |
Mixed echogenic thick septa |
||
|
1 |
Follicular cyst. |
38 |
10 |
- |
|
2 |
Corpus luteum cyst. |
5 |
- |
- |
|
3 |
Chocolate cyst. |
- |
1 |
4 |
|
4 |
Tubo ovarian abscess. |
- |
|
4 |
|
5 |
Hydatid cyst. |
- |
3 |
|
|
6 |
ovarian pregnancy. |
- |
1 |
3 |
|
7 |
HemorThagic cyst. |
- |
3 |
8 |
|
8 |
Simple ovarian cyst |
6 |
4 |
- |
Table IV: Non Neoplastic mass (in 90 women).
|
Histopathological finding |
Sonographic morphology |
||||
|
- |
Unilocular |
Multilocular thin septa |
Mixed echogenic thick septa |
solid |
|
|
1 |
Serous cyst adenoma |
8 |
9 |
6 |
1 |
|
2 |
Mucinous cyst adenoma |
- |
6 |
1 |
- |
|
3 |
Benign cystic teratoma |
- |
1 |
6 |
1 |
|
4 |
Fibro adenoma |
- |
1 |
1 |
|
|
5 |
Para ovarian cyst. |
3 |
- |
1 |
- |
|
6 |
Granulosa cell tumor. |
- |
- |
- |
1 |
|
7 |
Dys germinoma |
- |
- |
- |
2 |
|
8 |
Serous cyst adenocarcinoma |
- |
- |
1 |
1 |
Table V: Non Neoplastic mass (in 50 women).
|
Unilocular cyst |
|
|
Very common |
Follicular cyst. |
|
Corpus luteum cyst. |
|
|
Less common |
Simple cyst. |
|
Serous cyst adenoma. |
|
|
Para-ovarian cyst |
|
|
Uncommon |
Benign cystic teratoma. |
|
Mucinous cyst adenoma. |
|
|
Cyst Adeno fibroma. |
|
|
Rare |
Serous cyst adenoma. |
|
Granulosa cell tumor. |
|
Table VI: In this study found a unilocular cystic mass most frequent sonographic finding and a follicular cyst is the most common one.
|
S.No |
Type of neoplastic mass |
Occurrence |
|
1 |
Serous cyst adenoma |
28% |
|
2 |
Benign cystic teratoma |
18% |
|
3 |
Mucinous cyst adenoma |
15% |
|
4 |
Para ovarian cyst |
10% |
|
5 |
Fibro adenoma |
4.50% |
|
6 |
Dys germinoma |
5% |
|
7 |
Serous cyst adenocarcinoma |
5% |
|
8 |
Granulosa cell tumor |
4.50% |
|
9 |
Metastatic tumor |
5% |
Table VII: The morphological sonographic features of each mass with histopathological.
|
S.NO |
Type of neoplastic mass |
Occurrence |
|
1 |
Serous cyst adenoma |
28% |
|
2 |
Benign cystic teratoma |
18% |
|
3 |
Mucinous cyst adenoma |
15% |
|
4 |
Para ovarian cyst |
10% |
|
5 |
Fibro adenoma |
4.5% |
|
6 |
Dys germinoma |
5% |
|
7 |
Serous cyst adenocarcinoma |
5% |
|
8 |
Granulosa cell tumor |
4.5% |
|
9 |
Metastatic tumor |
5% |
Table VIII: The most common neoplastic masses is serous cyst adenoma and benign cystic teratoma. Serous cyst adenomas are bilateral in 40 %.
|
Age in Year |
Occurrence in % |
|
30-40 |
51% |
|
41-50 |
34.5% |
|
Over 50 |
14.5% |
Table IX: The distribution of benign serous cyst adenoma according to the age.
|
Ovarian Neoplasm |
|
|
Type |
Occurrence |
|
Premenopausal |
75% |
|
|
|
|
Post-menopausal |
25% |
|
Benign |
77.70% |
|
Malignant |
22.30% |
Table X: Demonstrate ovarian neoplasm and it’s occurrence in relation menstrual status.
|
Ovarian tumor size and malignancy |
|||
|
Tumor size |
Total |
Benign |
Malignant |
|
< 5cm |
6 |
6 |
0 |
|
5-10 cm |
19 |
17 |
2 |
|
>10 cm |
25 |
22 |
3 |
Table XI: The tumor size is important in the diagnosis of ovarian masses, in this study found that the larger size of the lesion the higher likelihood of malignancy. As shown in table XI.
|
Comparison between our study and other studies |
||||||||||||
|
Author |
Prevalence of various type of ovarian tumor |
Distribution of benign serous according to age |
Distribution according to menstrual status |
Distribution of tumor according to size |
||||||||
|
Benign |
Malignant |
30-40 Year |
41 -50 Year |
Over 50 year |
Pre-menopausal |
Post-menopausal |
Less than 5 cm |
5-10 cm |
Over 10 cm |
|||
|
Serous cyst adenoma |
Teratoma |
Serous Cyst adenocarcinoma |
Dys germinoma |
|||||||||
|
Roya Filly MD |
25 |
15 |
4.8 |
7 |
40 |
35 |
16 |
75 |
25 |
3 |
11 |
16 |
|
Meire HB |
22 |
15 |
4 |
4.5 |
51 |
34 |
15 |
75 |
25 |
1 |
13 |
15 |
|
Gromer BW and Cutier SJ |
20.5 |
17 |
4 |
6.3 |
52.8 |
33 |
15.2 |
75 |
25 |
0 |
13.5 |
15 |
|
Gove and Hertig AT |
26.6 |
18 |
3.6 |
4 |
48.2
|
35 |
16.8 |
75 |
25 |
0 |
12.5 |
17 |
|
Harilat KR and Thanagane |
20 |
18.7 |
4 |
4 |
49 |
37 |
14 |
76 |
24 |
0.8 |
11.8 |
15.2 |
|
Our Study |
28 |
18 |
5 |
5 |
51 |
34.5 |
14.5 |
75 |
25 |
0 |
10 |
12 |
Table XII: Demonstrate the comparison between our study and the study of previous authors. The distribution of tumor according to size in our study found that more increase in size the more likely hood of malignancy.
Citation: Abeda Ahmed Hamdoon, Yasamin Hadi Younis, Heba Zaid Mohamed (2019) The Validty of Ultrasound in Diagnosis Ovarian Masses. J Obstet Gynecol Probl: JOGP 100005.