Journal of Surgery and Insights
Research Article
Hospital Acquired Surgical Site Infections (SSI) At Al-Jalla teaching Hospital, Benghazi, Libya (2018)
Tajoury O1*, Shekteria A2, El-Jarary A1 and El-Boussefi I1
1Department of general surgery, Libyan International Medical University (LIMU), Libya
2Department of community medicine, University of Benghazi, Libya
*Corresponding author: Othman Tajoury, Department of general surgery, Libyan International Medical University (LIMU), Libya, Tel: +218910911450; Email: otmantaj@limu.edu.ly
Citation: Tajoury O (2019) Hospital Acquired Surgical Site Infections (SSI) At Al-Jalla teaching Hospital, Benghazi, Libya (2018). J Surg Insights: JSI-100009.
Received date: 02 November, 2019; Accepted date: 07 November, 2019; Published date: 14 November, 2019
Abstract
Background: Surgical site infections (SSI’s) are the third most commonly reported nosocomial infections which have an adverse impact on the hospital as well as on the. It's affecting about two million persons each year around the world especially in developing countries by about 16%.WHO pointed to the significance of financial effect and the suffering of patients who got SSI around the world.
Objectives: To find out the prevalence of SSI, risk factors implicated, organisms involved.
Methods: This study conducted in the Departments of Surgery, Al-Jalla teaching hospital, Benghazi, Libya. It is a descriptive-case series study and data of 204 cases who underwent surgery in 2018 are collected retrospectively and analyzed by using SPSS ver. 21.
Results: In this study, analysis of clinical data of 204 patients out of which 14.7% were infected post-surgery. The most common bacteria cause SSI was Staphylococcus aureus. Four statistically significant risk factors for SSI in these patients: prolonged operative time (P= 0.02) extended hospital stay (P=0.000) and urgency of surgery (P=0.007) along with anemia (P=0.007).
Conclusions: In the present study, the infection rate was higher than that in developed countries. Some risk factors have a significant association with an increase in the rate of SSI. Staphylococcus aureus was the most common organism isolated. Other comorbidities did not directly affect the rate of SSI in this study.
Recommendations: Correcting anemia before surgery and decrease the operation period might reduce SSI. Nurses and technicians training in OT & postoperative wards to improve the health care quality. Early nutritional support should begin to improve patient in the hospitalization. Monitoring systems, institutional antiseptic policy, should be developed. Quality control practices should turn into a routine and Medical auditing should be done regularly.
Keywords: Al-Jalla hospital; Prolonged hospital stay; Surgical site infections (SSI’s); Staphylococcus aureus
Abbreviations
HEPA : High-Efficiency Particulate Air.
LIM : Libyan International Medical University.
OT : Operation Theatre.
SPSS : Statistical Package for The Social Sciences.
SSI : Surgical Site Infection.
WHO : World Health Organization.
Introduction
Wound infection was defined as one in which a purulent discharge formed within 14 days of surgery [1-8]. Postoperative surgical site infections (SSI) have already been recognized to increase in duration of hospital stay with a subsequent increase in patient suffering and health care services cost, [1-4] particularly in developing countries where a frequency of about 16% was reported [5] World Health Organization (WHO) announced that hospital- Health-care associated infections are one of the main infectious diseases that are having a crucial financial effect globally [6,7]. Surgical site infections affect about two million persons each year around the world [8,9]. SSI is caused by the bacterial colonies on the patient’s pores and skin at the site of the wound. However gastrointestinal tract and genitourinary tract surgeries are the main sources that lead to SSIs along with the contamination of the equipment in the operation theatre. These infections typically occur within 30 days of operation or within one year if prosthesis or implant placement has been used [10-12].
This commonly happens to inpatients of hospitals but this may vary from hospital to hospital. Furthermore, it's one of the main causes of morbidity and mortality. SSI, is most commonly superficial. But can deeper involving the fascia and muscles while internal organs and body spaces are least involved. Many reports have been designed to estimate the rise in medical center stays, but recently with all the brand-new arrival of modern technology, it is currently possible to search for the procedure- and diagnosis-matched controls for each and every patient with SSI. This study tries to determine the frequency of risk factors for SSI at Al-Jalla hospital, Benghazi, Libya and try to produce a set of recommendations in regard.
Materials and Methods
Study subjects:Two hundred and four cases from four Surgery departments who underwent various surgical procedures in Al-Jalla Hospital, Benghazi were analysed.
Study area: This study was carried out at Al-Jalla teaching Hospital. This hospital is a560 bed hospital with an average daily census of 460 and a monthly admission rate of approximately 1570 Patients. The hospital serves the City of Benghazi with a population of approximately 650, 000 [13]. And is referral hospital for most of the eastern half of Libya. Al-Jalla Hospital is affiliated attached to Benghazi university and Libyan International Medical University (LIMU), Benghazi. Libya. The data collected from the 4 departments.
Study design: This is a descriptive-case series study and data are collected retrospectively.
Sampling and sample size: During the year 2018, 18900 patients underwent surgery at Al-Jalla Hospital, the sample size was calculated by using Epi-info program ver. 7.2. With a margin of error 5% and confidence level of 95%. The systematic random technique was used to select patient records.
The procedure of data collection and analysis: The required data were collected from patients' medical records, using a pre-prepared data collection pro-forma. Data were analyzed using SPSS v 21. Descriptive statistics such as; frequency, percentages, median, were determined. Also, the chi-square test was used to test the differences between proportions. A, P- value of <0.05 was taken as a threshold for significance.
Methods: To study the frequency of Surgical Site Infections (SSI) in the surgical wards of Al-Jalla Hospital, Benghazi. To determine the risk factors which contribute to SSI such as; duration of surgical procedure, duration of hospital stay. To determine the most frequent microorganism causes SSI.
Results
Most of the patients included in this study are fall in the age group between 15 to 30-year-old. The prevalence of SSI is 14.7% in the studied Hospital. The most bacteria were isolated from SSI is Staphylococcus aureus. Most cases were get infected are found in the general surgery department. Open surgery was the main technic that used in the Hospital. Excess hospital stay and length of operation time have a significant effect on the occurrence of SSI. Anemia is one of the most important factors that lead to increase the risk of SSI.
Two hundred and four patients were included in this study, the age ranged from 1month to 85 years, and the median age was 27 years and the most frequent age group was from 15-30 years (Figure 1).
One hundred thirty-five (66.2 %) are male (Figure 2).
(Figure 3), The Equal number of cases were collected from the data bank of 4 surgery departments.
The prevalence of surgical site infection SSI is 14.7%, (Figure 4).
The Culture and sensitivity were available in 72 cases, 42 (20.6%) patient’s test showed no bacterial growth result, while in 30 patient’s culture and sensitivity test showed different types of bacteria (Figure 5), shows the types of isolated bacteria, the most common (53.33% of the cases) was Staphylococcus aureus bacteria, while the E-coli is the least (3.3% of cases).
The Frequency of surgical site infection (SSI) was more common in general surgical wards than Neurosurgery 23.50%, and 15.70% respectively, while the least rate was shown in the plastic surgery ward by 7.80% (Table 1).
The Frequency of surgical site infection was significantly (P<0.05) more among patients who had emergency operations (Table 2).
No significant difference in the occurrence of SSI according to the type of procedure (Table 3).
There was no significant association (P>0.05) between the occurrence of surgical site infection and the history of medical health problems, (Table 4).
Out of 204 patients, 128(62.75%) stayed in the hospital more than the normal admission period which is expected for the uncomplicated cases. It was noted that the Patients with surgical site infection have a significantly (P=0.000) more hospital stay than those who are not infected (Table 5).
The frequency of infection is significantly (P<0.05) more among patients who had surgery duration for more than 2 hours (Table 6).
There was no significant association (P>0.05) between the occurrence of surgical site infection and the history of blood transfusion (Table 7,8).
Table 7: Frequency of the surgical site infection by the history of blood transfusion.
There was no significant association (P>0.05) between the occurrence of surgical site infection and the age group (Table 9).
Discussion
This study was conducted to identify the actual surgical site infection (SSI) rate at Al-Jalla hospital and to determine the risk factors associated with infection, specifically for patients who underwent surgical procedures either in an emergency or elective OT. Surgical site infection (SSI) is still considered the most Significant cause of morbidity and is the most common nosocomial infection in the patients who went through surgery [14-20] this study was carried out using the hospital records the data of 204 patients who were operated either electively or emergently in Al-Jalla hospital Benghazi, Libya. Most of the patients are resident in Benghazi144 (71%), and 60(29%) are from other cities. In addition, (88%) are Libyan, while (12%) are non-Libyan. Majority of the surgeries were performed on head and neck followed by Lower limb, Upper limp, abdominal, vertebral spine, breast, and chest. As in most studies conducted in the developing world, the frequency of SSI in this study was high at 14.7%. On the other hand, the overall SSI rate in mainland China was 4.5% [21] and that in Seoul, South Korea, at 3.3% [22] and that in the US is 2-3% [23]. In Ethiopia, SSI rates were found at 10.6% [24] whereas in a private hospital in Kenya incident rates of 7.0% were found [25] and the overall SSI rate in Nepal and Tanzania was 23% and 26%, respectively [26,27]. The highest rate of SSI in this study was among the cases in the General Surgery ward (23.5%) followed by the Neurosurgery ward (15.7%) then orthopaedic ward (11.8%), and the lowest rate was clearly observed in the Plastic surgery ward (7.8%) (Table 1). Prolonged operative time can increase the risk of SSI; there is a well-known average time for each surgical procedure [28]. In fact, this correlation has been established since 1964 by the Public health laboratory services (PHLS) in England and Wales [29]. Data analysis display a considerable finding which is that a significant relationship between the operation time and the probability of SSI. The rate of SSI for the duration of more than 2 hours is (21.2%), while in time less than 2 hours is (9.65%) (Table 2). As well with an increase of operative time, the patient's incisions are longer exposed to the surroundings, which leads to increase the chance of bacterial infections. In addition, that may lead to a decline in the use of aseptic measures during the surgery. Furthermore, longer surgical period predisposes incisions to tissue desiccation which might increase the chance of contaminants [28, 30,31]. An extended surgical time causes exhaustion and could become associated with intraoperative difficulties. On top of that, a prolonged operative time is often associated with increased loss of blood which leads to tissue hypoxia [32]. In the present study, the higher proportion of SSI was found among the individuals who operated as an emergency case (20%) (Table 3). This is due to the patient’s critical conditions, for example, multiple traumas patient enters a catabolic state which causes low immunity and prone to develop SSI. Use of many instruments and short time of preparation can lead to an inability to maintain sterility during surgical procedures. These kinds of findings reveal deficiencies of adequate care, and poor resource, structural restrictions, and lack of knowledge concerning nosocomial infections. Technical advances in infection control like utilization of high-efficiency particulate air (HEPA) filter systems in theaters to minimize microbial loads remain lacking in the Libyan setting which simply might contribute to the high prevalence of SSI. Consequently, the high measures of healthcare in the developed countries stay as the utmost conceivable explanation for this difference in the rates of infection [32]. Although all the cases of SSI were in the open type of procedure 16.3%, there is no statistical significance between the type of procedure and occurrence of SSI (Table 4). A similar result was found regarding the site of incision which has no statistical significance in the occurrence of SSI according to the site of the incision. In the present study, there is absolutely no effect of gender on the development of SSI, similar to the results reported [33]. On the other hand, a number of studies show that the risk of SSI increases in males (7.4%) compared to (5.1%) in the female [34]. Furthermore, In Aligarh, females (27%) showed a preponderance of SSI than males (18%) [35]. Co-morbid conditions like anemia were the significant risk factors for SSI by (20.5%) (table5). Haemoglobin of 13 and 12 gm% were considered as the cut off points for the diagnosis of anemia in men and women respectively [36]. As shown in recent studies which say that iron may slow down wound healing through its action as a free radical. Elevated free iron and a rise in reactive oxygen species released from neutrophils represent pathologic key steps (via the Fenton reaction) that are considered to be accountable for the prolonged inflammation, increased connective tissue damage, and lipid peroxidation that contributes to the pro-oxidant hostile environment of chronic wounds [37]. Thus, by adding to toxic free radicals, iron may also impair wound healing [38]. In the present study, there is no association between Diabetes and the development of SSI (Table 6). In contrast to the National Academy of Science that reported a higher rate of infection in patients with Diabetes mellitus [39]. Moreover, there is no association between blood transfusion & serology positive& SSIs in the current study, (Table 7) Compared to other studies were done. Blood transfusion was found to be an important risk factor in Determining SSI [40].
A prolonged hospital stay with exposure to the hospital environment has been shown to increase the risk of SSI (Table 8) [41], Comparable findings were found in the present study also reported a higher rate of SSI in patients with a prolonged hospital stay [41,42] protracted hospital stays result in bacterial colonization with antimicrobial resistance, which increases the susceptibility to infection either by reducing host resistance or by providing increased opportunity for ultimate bacterial colonization [43]. Pre-operative antibiotics are known to decrease the incidence of SSI cases [42,29,44] prophylactic antibiotic usage was not a routine in the studied hospital. Only selected patients who had some infection or other risk factor received antibiotic prophylaxis. Staphylococcus aureus was the predominant organism isolated from the surgical sites in the studies hospital followed by Pseudomonas and Klebsiella then pseudomonas with Staphylococcus aureus lastly is E. coli. Staphylococcus aureus forms the bulk of the normal flora of skin and nails [45] The high incidence of gram-positive organisms in SSI can be attributed to being acquired from a patient’s normal endogenous microflora [46] Hence; it is the commonest organism found in most of the SSIs also found a preponderance of Staphylococcus aureus and Pseudomonas SSIs in their studies [41,47] Many studies have reported Staphylococcus aureus as the commonest isolate from the postoperative wound infection [46,48,49]. Other organisms have shown varied preponderance indifferent studies. The ages of study cases that collected ranged between1 month to 85 years. The majority (38.2%) of them belonged to 15-30 years’ group. Out of 78 Patients in this group, 8 (26.7%) got SSI. 45 patients were more than 30 years and among them, 10 (33.3%) developed SSI which is the highest rate among the groups (Table 9). However, there is no statistical difference between the patients in the occurrence of SSI according to the age. On the other hand, 11 patients in the older age group > 63 years, only 2 (6.7%) were have SSI. Therefore, the frequency of SSI doesn’t affect with the age. In contrast to the other studies that found the rate of SSI increases with the increase in the age [43,50-52].
Conclusion
The frequency of SSI among the postoperative patients at Al-Jalla Hospital is high compared to that in the developed world. However, the most significant risk factors for the occurrence of SSI are prolonged operative time, extended hospital stay and urgency of surgery along with anemia were significant for developing SSI, throughout a broad variety of surgical procedures and surgical specialties. Staphylococcus aureus was the most common organism associated with SSI. Overall, data analysis indicated that patients with SSI more porn to stay longer than recommended according to their conditions.
Recommendations
The studied Hospital should concentrate attempts to minimize surgery time, especially in emergency cases. This might consist of preventive strategies including the use of recent technology that will help improve operative efficiency, employment of specialized care teams, making certain operating personnel are not overworked or maybe tired, and then greater preoperative preparation. Training of Nursing staff and technicians in postoperative wards regarding maintenance of strict aseptic environment to improve the health care quality. These types of strategies should be thought about in light of additional possible risk factors for SSI. The trauma patient enters a catabolic state after injury. It is important to monitor the caloric intake of these patients and to be aware of the importance of a positive protein balance both preoperatively and postoperatively. Attempts to maintain nutrition should begin early in the hospitalization. It is important to maintain a high index of suspicion for SSI. Once the suspicion of infection is confirmed, treatment should be prompt and aggressive in an effort to give the patient the best possible outcome. SSI remains a major concern after surgery, particularly in the trauma setting. Awareness of possible risk factors and appropriate antibiotic use may improve outcomes. Furthermore, Monitoring systems, institutional antiseptic policy, should be developed. Quality control practices should turn into a routine and Medical auditing should be done regularly.
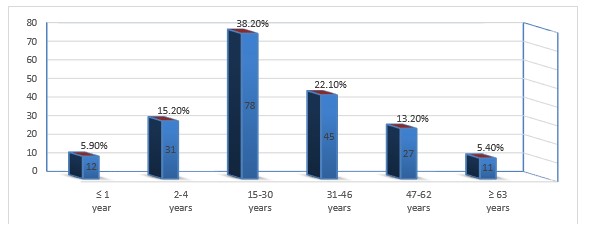
Figure 1: Distribution of the patients according to age groups.
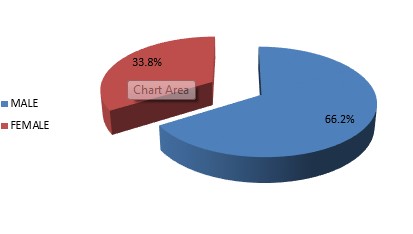
Figure 2: Distribution of the patients according to their gender.
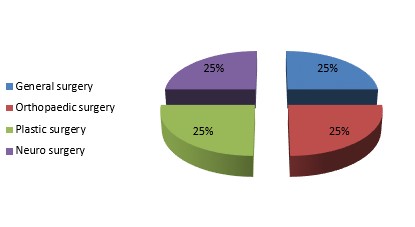
Figure 3: Distribution of the patients according to the hospital wards.

Figure 4: Distribution of the patients according to the data of surgical site infection.
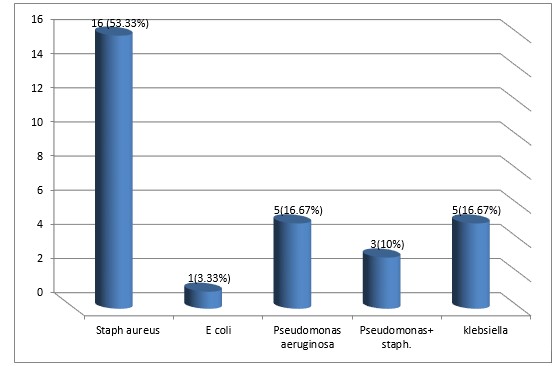
Figure 5: Types of bacteria isolated from the infected wounds.
|
Ward |
Surgical site infection |
|
Total (%) |
|
Yes (%) |
No (%) |
||
|
General surgery |
12 (23.50) |
39(76.50) |
51(100) |
|
Orthopedic surgery |
6 (11.80) |
45(88.20) |
51(100) |
|
Plastic surgery |
4(7.80) |
47(92.20) |
51(100) |
|
Neurosurgery |
8 (15.70) |
34(84.30) |
51(100) |
|
Total |
30 (14.70) |
174(85.30) |
204(100) |
Table 1: The proportion of SSI in every ward.
|
Type of operation |
Surgical site infection |
Total |
X2
|
P
|
|
|
Yes |
No |
||||
|
Elective |
5( 6.3%) |
74 (93.7%) |
79 (100%) |
7.213 |
0.007 |
|
Emergency |
25( 20%) |
100 (80%) |
125 (100%) |
- |
- |
|
Total |
30 (14.70%) |
174 (85.30%) |
204 (100%) |
- |
- |
Table 2: Frequency of the surgical site infection by the type of operation.
|
Type of procedure |
SSI |
Total |
X2 |
P |
|
|
Yes |
No |
||||
|
Open |
30 (16.3%) |
154 (83.7%) |
184 (100%) |
3.82 |
0.148 |
|
Laparoscopic |
0 (0.0%) |
5 (100%) |
5 (100%) |
- |
- |
|
Close1 |
0 (0.0%) |
15(100%) |
15 (100%) |
- |
- |
|
Total |
30 (14.7%) |
174 (85.3%) |
204 (100%) |
- |
- |
|
Note: 1- Fracture long bone is often treated with intramedullary nailing just with stab incision. |
|||||
Table 3: Distribution of the patients by type of procedure and occurrence of SSI.
|
Associated comorbidity |
Surgical site infection |
Total |
X2 |
P |
|
|
Yes |
No |
||||
|
Yes |
14 (16.5%) |
71(83.5%) |
85 (100%) |
0.362 |
0.548 |
|
No |
16 (13.4%) |
103(86.6%) |
119 (100%) |
- |
- |
|
Total |
30 (14.70%) |
174(85.30%) |
204 (100%) |
- |
- |
Table 4: Frequency of the surgical site infection by the history of co-morbidity.
|
Excess hospital stay |
Surgical site infection |
Total
|
X2 |
p
|
|
|
Yes |
No |
||||
|
Yes |
29(22.66%) |
99 (77.34%) |
128 (100%) |
17.314 |
0 |
|
No |
1 (1.32%) |
75 (98.7%) |
76 (100%) |
- |
- |
|
Total |
30 (14.70%) |
174 (85.30%) |
204(100%) |
- |
- |
Table 5: Frequency of the surgical site infection by the history of excess hospital stay.
|
Length of operation |
Surgical site infection |
Total |
X2 |
p |
|
|
Yes |
No |
||||
|
≤ 1hour |
11(9.65%) |
103 (90.35%) |
114 (100%) |
5.268 |
0.02 |
|
≥ 2 hours |
19 (21.1) |
71 (98.9%) |
90 (100%) |
- |
- |
|
Total |
30 (14.70%) |
174 (85.30%) |
204 (100%) |
- |
- |
Table 6: Frequency of the surgical site infection by the length of operation in hours.
|
History of blood transfusion |
Surgical site infection |
Total |
X2 |
p |
|
|
Yes |
No |
||||
|
Yes |
1 (16.66%) |
5 (83.33%) |
6 (100%) |
0.019 |
0.891 |
|
No |
29 (14.65%) |
169 (85.4%) |
198 (100%) |
- |
- |
|
Total |
30 (14.70%) |
174 (85.30%) |
204 (100%) |
- |
- |
Table 7: Frequency of the surgical site infection by the history of blood transfusion.
|
Anemia |
Surgical site infection |
Total |
X2 |
p |
|
|
Yes |
No |
||||
|
Yes |
24 (20.5%) |
93 (79.5%) |
117 (100%) |
7.375 |
0.007 |
|
No |
6(6.9%) |
81 (93.1%) |
87 (100%) |
- |
- |
|
Total |
30 (14.70%) |
174 (85.30%) |
204 (100%) |
- |
- |
Table 8: The frequency of infection is significantly (P<0.000) more among anemic patient.
|
Age groups |
Surgical site infection |
Total |
X2 |
p |
|
|
Yes |
No |
||||
|
≤ 1 year |
1 (3.3%) |
11 (6.3%) |
12 (5.9%) |
4.56 |
0.47 |
|
2 to 14 years |
6 (20.0%) |
25 (14.4%) |
31 (15.2%) |
- |
- |
|
15 to 30 years |
8 (26.7%) |
70 (40.2%) |
78 (38.2%) |
- |
- |
|
31 to 46 years |
10 (33.3%) |
35 (20.1%) |
45 (22.1%) |
- |
- |
|
47 to 62 years |
3 (10.0%) |
24 (13.8%) |
27 (13.2%) |
- |
- |
|
≥ 63 |
2 (6.7%) |
9 (5.2%) |
11 (5.4%) |
- |
- |
|
Total |
30 (100%) |
174 (100%) |
204 (100%) |
- |
- |
Table 9: Frequency of the surgical site infection by the age group.
Citation: Tajoury O (2019) Hospital Acquired Surgical Site Infections (SSI) At Al-Jalla teaching Hospital, Benghazi, Libya (2018). J Surg Insights: JSI-100009.