Clinical Oncology Research Journal
Flattening Filter Free Beams for 3DCRT: Is Shape of the Beam Profile an Added Advantage?
Mundayadan Chandroth M*, Venning A, Hodgson A, Chick B, Waller B
Department of Radiation Oncology, Mid North Coast Cancer Institute, Port Macquarie, NSW, Australia
Corresponding author: Mundayadan Chandroth M, Department of Radiation Oncology, Mid North Coast Cancer Institute, Port Macquarie, NSW, Australia.
Citation: Mundayadan CM, Venning A, Hodgson A, Chick B, Waller B (2019) Flattening Filter Free Beams for 3DCRT: Is Shape of the Beam Profile an Added Advantage?. Clin Oncol Res J: CORJ-100003.
Received Date: 08 April, 2019; Accepted Date: 06 May, 2019; Published Date: 17 May, 2019
Abstract
Megavoltage radiotherapy has proven to be highly effective for the treatment of basal cell carcinoma (BCC) of the nose. A common treatment technique has been 3D conformal, half-beam blocked, lateral, parallel opposed, 6 MV flat beams, using a symmetric wax block to provide uniform dosimetry across the treatment region. One issue we identified with the wax block method is the significant time overhead involved to manufacture and fit the block to the patient’s nose. In this study, we investigated the use of flattening filter free (FFF) beams with thermoplastic bolus used as an alternative to the wax block method, exploiting the wedged shape of a half-beam blocked FFF field. The use of thermoplastic bolus significantly reduces the manufacturing overheads and time required for simulation setup, while improving the patient’s comfort and experience. We acquired a cohort of 10 patient plans for the two techniques, with each plan assessed and approved by a radiation oncologist. We subsequently applied a range of plan evaluation metrics to compare the two techniques for various dosimetric end points. We found that, for the metrics applied, there was no statistically significant difference between the two planning methods. In conclusion, it was found that using 3D conformal FFF planning with thermoplastic bolus provides an efficient method in terms of simulation, maintenance of hygiene, patient comfort, time and cost effectiveness.
Keywords: skin cancer, wax block, flattening filter free
Introduction
Non-melanoma skin cancers are the most common cancers in Australia, with 642 associated deaths recorded in 2015 [1]. Basal cell carcinoma (BCC) accounts for approximately 70% of non-melanoma skin cancers and often has no symptoms. The nose is a very common anatomical site for BCC skin cancer to occur due to the increased exposure to the sun. Radiotherapy is an effective treatment method for these cancers and is often delivered using megavoltage (MV) photon beams. Our Centre has treated nearly 100 patients for BCC of the nose in the last 10 years with radical intent (5000 cGy in 20 fractions) using 3 dimensional conformal radiation therapy (3DCRT). Historically, we have used half-beam blocked, lateral, parallel opposed 6 MV flat beams to treat the nose. In order to compensate for the lack of tissue, and due to the shape of the nose, a custom made square wax block was used to achieve a uniform dose distribution (wax block method). Our Centre uses the Monte Carlo (MC) algorithm of the Monaco® (Elekta AB Stockholm) treatment planning system (TPS) for routine treatment planning. The MC algorithm does not support wedges and hence, we do not use them in our Centre. If a wax block is not used, it can lead to a substantial dose gradient between the nasal tip and the base, compromising the dose coverage, which can be detrimental to the treatment outcome (Figure 1). The manufacture of a wax block requires a high degree of skill and takes hours of mould room work prior to the patient attending simulation. The placement of the wax block onto the patient at simulation can be challenging and requires perfect timing for the wax block to be soft enough to be pushed onto the patient’s nose, making good contact with their regular shape of the protruding anatomical structure. If the wax block is too soft, it can potentially change shape and deform. Alternatively, if the wax block is too hard the pressure placed onto the patient’s nose as it is pushed on can cause significant discomfort and the appointment may require to be re-booked while another wax block is manufactured. Air gaps between the block and the underlying skin can lead to dosimetric errors. Furthermore, we have encountered instances when the physical integrity of the wax block has been compromised during the treatment period forcing the remanufacture of the wax block, which can lead to a delay of treatment in the interim. Maintaining the sanitation of the wax block has also posed challenges. From a patient’s perspective, with possible blisters from the cancer treatment, it is uncomfortable to have a relatively heavy piece of treatment accessory placed on the nose.
Flattening filter free (FFF) beams have been proven to reduce treatment time for stereotactic body radiation therapy (SBRT) due to the higher dose rate [2]. FFF beams are inherently non–flat due to the absence of a flattening filter, with dose falling off steeper laterally. Intensity modulated radiation therapy (IMRT) and volumetric modulated arc therapy (VMAT) segments are usually small in area and hence the shape of the FFF beam is not profound within the segments, particularly on the central axis. Modern day treatment planning systems are highly capable of optimizing the dose distribution of FFF beams for IMRT and VMAT for narrow field off-axis geometry. These features of FFF beams makes it ideal to use with IMRT and VMAT, which increases the efficiency of treatment delivery. The use of FFF beams for conventional 3DCRT has been limited due to the shape of the profile which does not provide a uniform dose distribution across the field. Also, when conventional fractionation regimes are used, increased dose rate does not provide a substantial reduction in treatment time. In order to address the issues related to the wax block method, as a novel approach, FFF beams are used for treatment planning of the nose [3]. The shape of the profile of half-beam blocked FFF beam to some extent compensates the anatomical variation of the nose, which is made use of in this approach. Our Centre uses 6MV FFF beam along with 1 cm thermoplastic bolus for this method of treatment (FFF beam method).This technique aims at achieving an equivalent or superior dose distribution without the use of wax blocks or wedges. This study aims at comparing the dosimetric and practical aspects of the ‘6 MV flat wax block method’ and the ‘6MV FFF 1 cm thermoplastic bolus method’ and thus, providing a guideline for implementing a methodology for improved patient experience.
Methodology
Our Centre is equipped with 6 MV flat and 6MV FFF beams, matched for beam energy and output at 10 cm depth in water for 10 × 10 cm2 field. The existing method of treatment of the nose is the wax block method (Figure 1a) - using the 6 MV flat beam. In this, a wax block is custom made to compensate for the anatomy of the nose and the dosimetry of the flat beam (Figure 2).
This is performed during the CT simulation where due care is taken to avoid any air gaps between the skin of the nose and the wax block. Once the wax block is made, the CT simulation is performed with the wax block in place on the patient. The treatment plan is generated using half-beam blocked, lateral, opposed beam pair beams with 6 MV flat, with the aim to spare dose to the lens of the eyes. The dose prescription is to the midline (5000 cGy in 20 fractions) and the TPS calculates the monitor units (MU) required to achieve the target dose prescription. A secondary MU check program (RadCalc®, LifeLine Software Inc.) is implemented to verify the MU calculated by the TPS. As the MC algorithm in Monaco does not support the use of wedges, this limits the optimisation of the treatment plan.
This leads to the introduction of the new method, which uses half-beam blocked 6MV FFF beams instead of the 6 MV flat beams. The shape of the profile of a half-beam blocked 6MV FFF beam is shown in (Figure 3).
The typical size of the field used to treat the nose is about 5 × 5 cm2 which could be achieved by using a half-beam blocked 10 × 10 cm2 field. The dose reduces to about 60% of the central axis dose at 4.5 cm off-axis as seen in the Figure 3. The advantage of the half-beam blocked beam is that when the isocentre is placed at the posterior border (nasal base) of the target, the shape of the beam profile matches the anatomy of the nose, which leads to a symmetrically uniform dose distribution. This also assists in preventing beam divergence posteriorly thus reducing dose to the organs at risk (OAR).The wax block was replaced with 1 cm thick thermoplastic bolus to provide build up, thereby ensuring sufficient skin dose (Figure 4).
In order to compare the quality of the two treatment techniques, 10 patient plans using each method were analysed for various dosimetric end points. They include monitor units (MU), maximum point dose (Dmax), volume of tissue receiving 105% of the prescription dose (V105) and the percentage difference in MU between Monaco and RadCalc (MUdiff). Student’s paired t-test is used to compare these parameters from the two sets of plans with a p value <0.01 considered statistically significant. Along with the dosimetric outcomes, the easiness of handling the treatment accessories by the radiation therapists and the patient comfort are evaluated qualitatively for the two methods.
Results
In consultation with a radiation oncologist, both techniques employed correct planning methods including the position of the isocentre and prescription point resulted in the generation of treatment plans with clinically acceptable dose distributions. The 6MV FFF plans had an average MU of 219.82 (range 15.51MU) compared to the 219.07 (range 11.35MU) for the 6 MV plans showing no statistically significant difference between the two techniques (p > 0.01), in terms of the MU used to deliver the same dose. This is because the two beams used are similar for their output and energy under reference conditions. The maximum point dose (Dmax) was assessed for the two treatment methods with an average Dmax of 5294.5 cGy (range 297.7 cGy) for 6MV FFF compared to 5310.3 cGy (range 179.0 cGy) for 6 MV flat also showing no statistically significant difference between the two techniques (p > 0.01), in terms of Dmax. The average V105 (cc) for the set of 6MV FFF plans was 0.45cc showing a highly uniform dose distribution within the target area. For the 6 MV set of plans, this is 1.3cc showing no statistically significant difference between the two techniques (p > 0.01). The other parameter used to compare the two techniques was the agreement of the MUs calculated by Monaco to the secondary MU check program (RadCalc), for which both sets of plans were within tolerance on average. For the 6 MV FFF plans, the average agreement was 1.5% (maximum 2.5%) and for 6 MV it was 3.2% (maximum 3.9%), showing a statistically significant difference between the two techniques (p < 0.01). This difference is due to the secondary MU calculation algorithm being better optimised for the 6 MV FFF beam compared to the 6 MV beam. The results are summarized in (Figure 5).
Discussion
Considering the practical aspects of handling treatment accessories, the FFF method quickly gained popularity locally due to two major reasons. Firstly, it is easier to maintain the integrity of the bolus used in the FFF method compared to the wax block [4]. Maintaining the positional accuracy of the wax block over the course of treatment is extremely difficult compared to that of the thermoplastic bolus. Secondly, the bolus method scored higher in terms of maintaining the hygiene compared to the wax block. This is because that wax is inherently difficult to clean and can lose its integrity after wiping it with cleaning solution for a few times. In terms of patient comfort, the thermoplastic bolus method was superior to the wax block method. The elimination of pre-simulation mould room tasks, such as making the wax block shell, half filling it the day before and filling it an hour before simulation all contribute to the radiation therapists preferring the 6MV FFF thermoplastic bolus technique [5]. The greatly reduced simulation appointment time, the elimination of the need to push the wax block onto the nose, and the increased cleanliness all contribute to the patient’s enhanced comfort with the 6MV FFF thermoplastic bolus method.
Conclusion
The introduction of the FFF method in the treatment of nose using 3DCRT enabled our Centre to generate clinically acceptable and comparable plans to the wax block method [6]. The FFF method eliminated the requirement to pre-manufacture and maintain the wax block and reduced simulation set up time. The FFF method is a more cost effective treatment option with less mould room time, reduced overheads of managing and scheduling pre-simulation tasks and reduced use of consumable resources. Whilst the advantages of FFF energies are widely associated with high dose fraction regimes such as SBRT treatments, the local team has demonstrated the benefits in exploiting the unique FFF beam profile for the treatment of the nose in simple conformal beams, substituting the requirement for wedges.
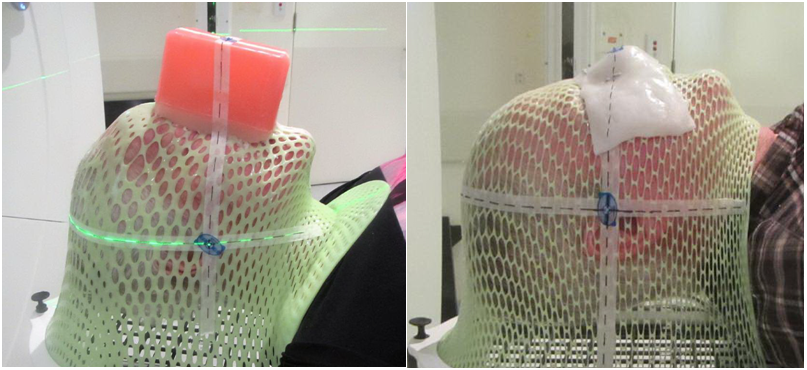
Figure 1: Comparison of the two techniques 1a) Wax block method 1b) FFF beam method
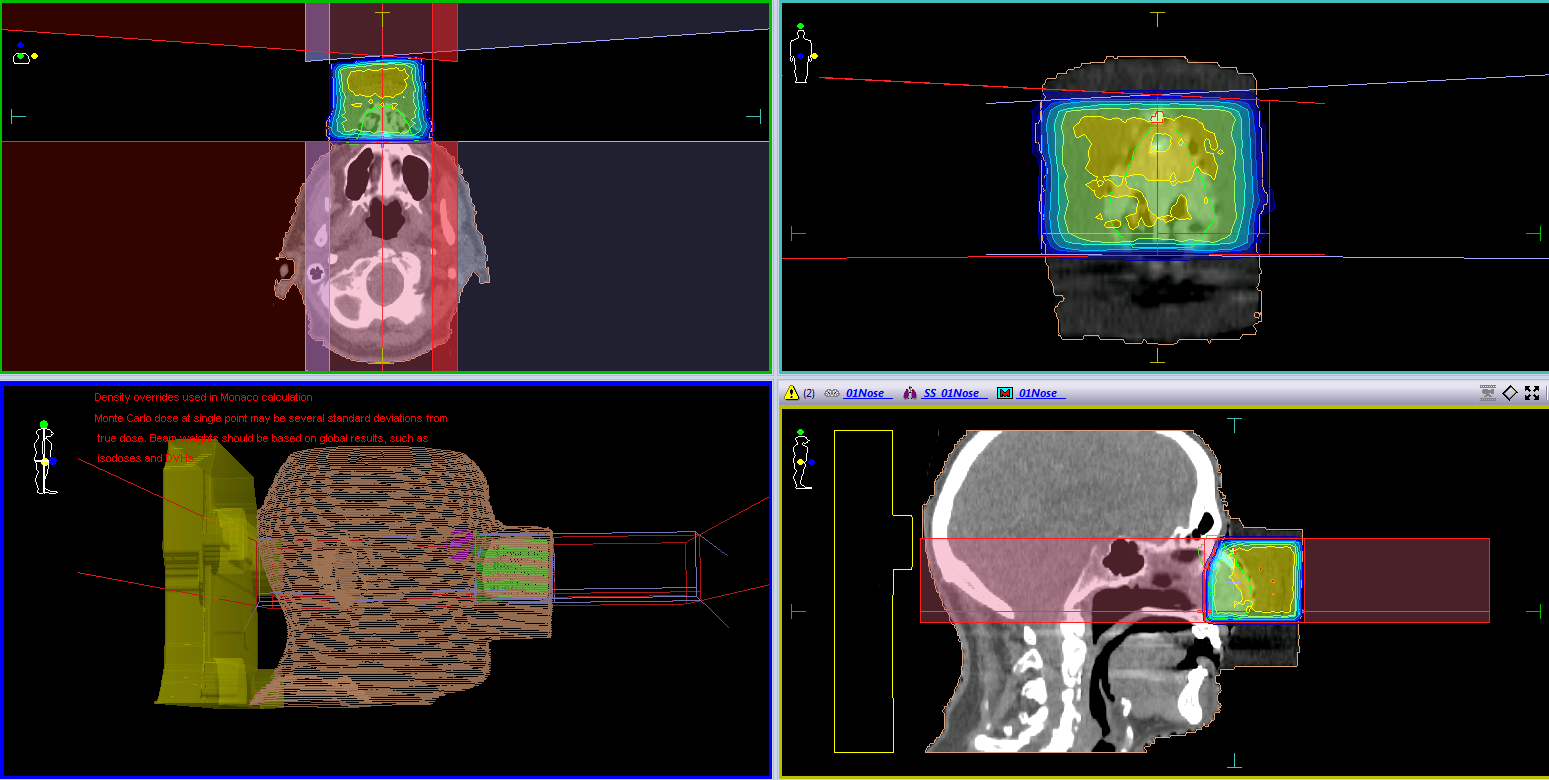
Figure 2: 6 MV flat wax block method
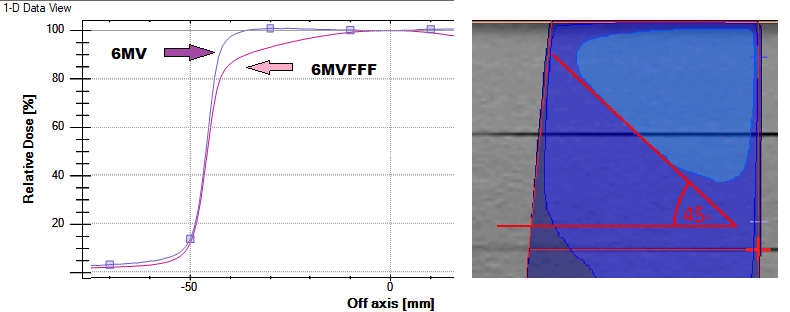
Figure 3: A comparison of 6 MV and 6MV FFF beams for 10x10 cm2 at Dmax
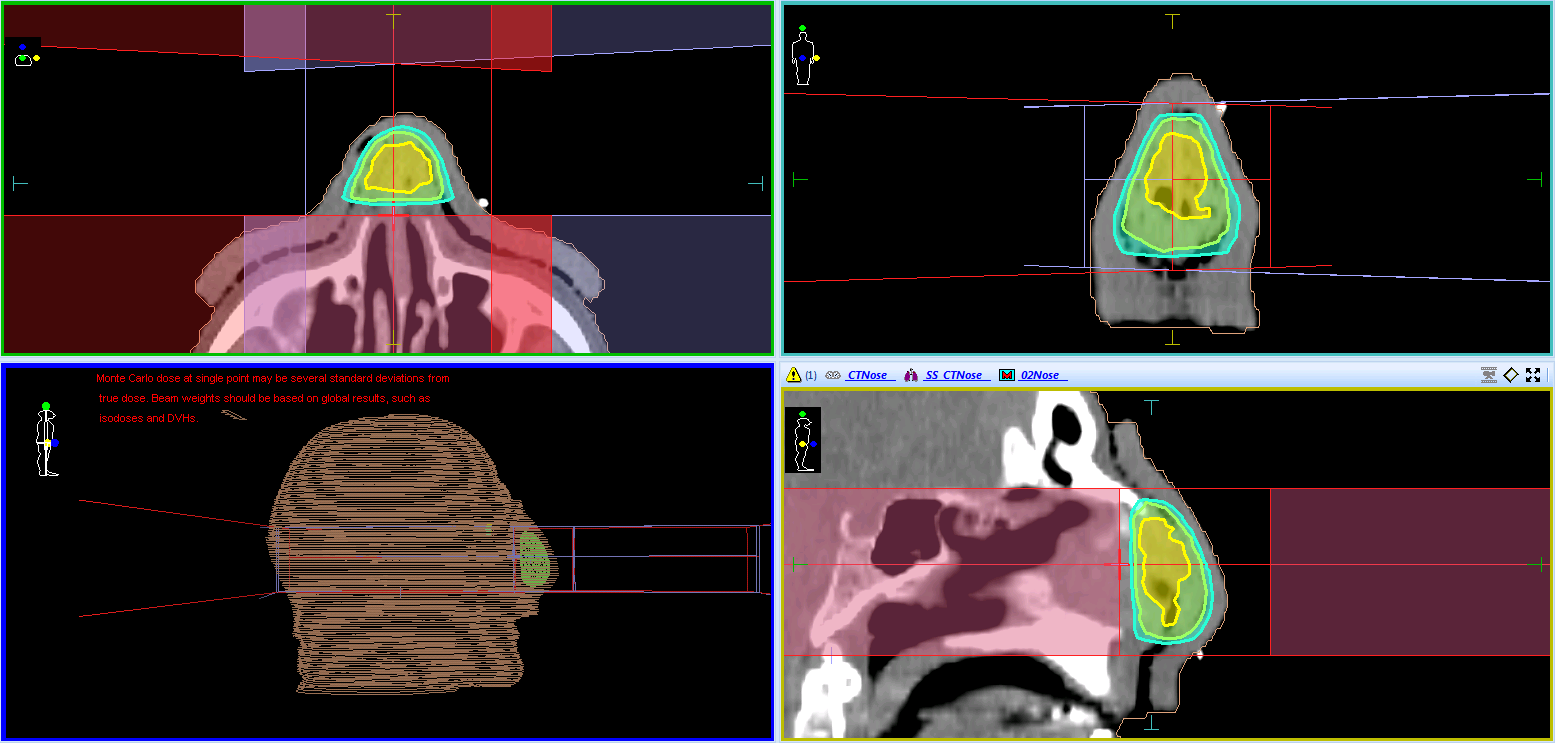
Figure 4: 6MV FFF 1 cm thermoplastic bolus method
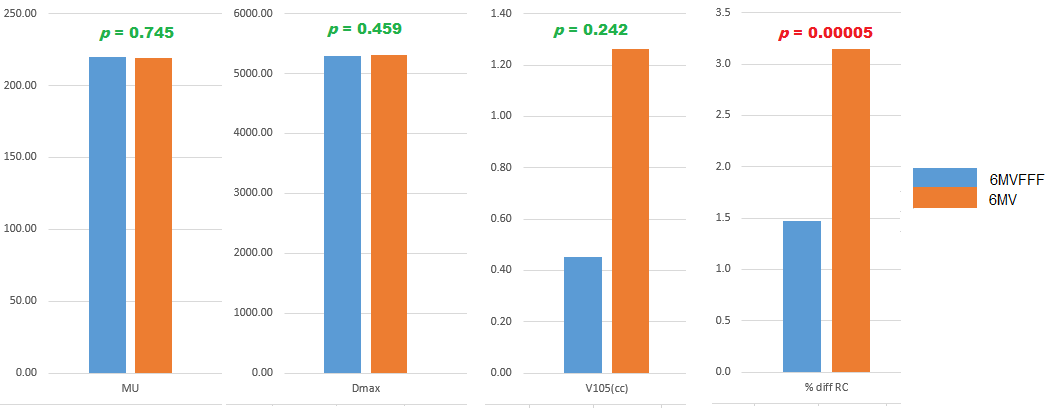
Figure 5: Summary of results
Citation: Mundayadan CM, Venning A, Hodgson A, Chick B, Waller B (2019) Flattening Filter Free Beams for 3DCRT: Is Shape of the Beam Profile an Added Advantage?. Clin Oncol Res J: CORJ-100003.