Annals of Medical & Surgical Case Reports
Mediterranean-Style Diet Co-Supplemented with Synbiotics Improved Quality of Life, Fatigue and Disease Activity in Five Secondary Progressive Multiple Sclerosis Patients
Amir Reza Moravejolahkami1* and Ahmad Chitsaz2
1Department of Clinical Nutrition, School of Nutrition & Food Science, Isfahan University of Medical Sciences, Isfahan, Iran
2Department of Neurology, Isfahan University of Medical Sciences, Isfahan, Iran
*Corresponding author: Amir Reza Moravejolahkami, Department of Clinical Nutrition, School of Nutrition & Food Science, Isfahan University of Medical Sciences, Hezar-Jerib Ave, Isfahan, Iran.
Citation: Moravejolahkami AR and Chitsaz A (2019) Mediterranean-Style Diet Co-Supplemented with Synbiotics Improved Quality of Life, Fatigue and Disease Activity in Five Secondary Progressive Multiple Sclerosis Patients. Ann Med & Surg Case Rep: AMSCR: 100006.
Received Date: 05 May, 2019; Accepted Date: 08 May, 2019; Published Date: 15 May, 2019
Abstract
Backgrounds & Aims: Mediterranean diet and synbiotic supplementation have been considered as important modulators of immune system especially in autoimmune disease like multiple sclerosis (MS), especially in Secondary Progressive MS (SPMS) that deteriorates gradually in functions during the time and has not any specific treatment. So this study was conducted to describe five SPMS patients adhered to Mediterranean-style diet and synbiotic supplementation in a 12-month period.
Methods: A diet enriched with fibers, omega-3 and calorie restricted was designed and trained. In addition, 7 strains of bacteriaand Fructooligosaccharide were given as a capsule two times per day.
Results: Serum inflammatory marker, fatigue and disability were suppressed about 64, 31, and 27 %, respectively; while quality of life was improved by ≈ 23 %.
Conclusions: Mediterranean diet co-supplemented with synbiotics may contribute to MS improvement, especially in SPMS cases that have not any well-known treatment.
Keywords: Disease activity; Mediterranean diet; Multiple sclerosis; Probiotics; Prebiotics; Synbiotics
Introduction
Although there are about 10 disease-modifying therapies to stop the progression of MS, these are not effective in Secondary Progressive MS (SPMS). In autoimmune diseases like this case, the goal of treatment should be focused on controlling inflammatory processes directed bycomplete compliance with Mediterranean diet (MeD) and correcting the gut microbiome by Synbiotics (pre & probiotics) [1].
Most interventions in this area have so far focused on animals. Administration of Bi?dobacteriumbi?dum, Lactobacillus and Streptococcus thermophilus reduced the intensity of EAE (Experimental Autoimmune Encephalomyelitis; animal model of MS) by decreasing Th1 and Th17 (CD4+ cells) and increasing Treg cells in rats [2]. The possible mechanisms are very complex and need more investigations.Shortly, the failure of microbial balance and enhancing the pathogen strains rather than probiotics in the gut microbiota lead to low-grade endotossemia, intestinal and systemic chronic inflammation [1]. On the other hand, Fructooligosaccharides and Galactooligosaccharides (high in MeD) increase the number of Bi?dobacteria and Lactobacillus, and this change in gut microbiota leads to modulation of inflammatory processes [3,4].Theoretically, high values of omega-3 fatty acids and antioxidants in MeD suppresses the activation of nuclear factor-kB (NF-κB) and Activator Protein-1 (AP-1) –two main pro-inflammatory transcription factors involved in T-cell induction –in order to stopping overexpression of pro-inflammatory products in MS [5]. In a recent study, we also observed the positive impacts of MeD on serum hs-CRP levels and the other MS-related clinical manifestations [6].
Here, we reported fiveSPMS patients with high disability who wereadhered to Mediterranean-style diet and received synbiotic supplementation. The positive effects on these patients will be a key point of our discussion.
Case Presentation
FiveSPMS women were visited into MS outpatient clinic on September 11, 2017, and referred to dietitian with a completed consent form. A Mediterranean-style diet consists of 117 mg EPA (Eicosapentaenoic Acid) and 404 mg DHA (Docosahexaenoic Acid) omega-3, 29.16 g Dietary fiber, 6.148 g insoluble fiber, 6.148 g insoluble fiber 768 mg, 7.278 g crude fiber, 13.12 g linoleic fat was designed and trained to patients. Intake of saturated fat was lowered to 16.32 g (9-10% of total fat) and calorie intake was kept on about 1800-1900 kcal (percent of macronutrients: carbohydrate ≈ 45%; protein ≈ 17%; fat ≈ 38%).
At the same time with dietary intervention, we started synbiotic therapy. The administered capsules were contained 7 strains of live bacteria as a probiotic (Lactobacillus casei, Lactobacillus rhamnosus, Streptococcus thermophilus, Bifidobacterium breve, Lactobacillus acidophilus, Bifidobacteriumlongum, Lactobacillus bulgaricus) with dose of 108 CFU and concentrated Fructooligosaccharide (FOS) 100 mg as a prebiotic, which were taken twice a day.
Clinical findings were measured at baseline and intervals of 4/8/12 months after intervention (Table 1). Disability was measured by Extended Disability Status Scale; overall, it dropped by 26.82% in comparison to baseline. In addition, fatigue showed a 31.32% improvement through Fatigue Severity Scale calculation.
Physical and Mental Health Composite (PHCS & MHCS), which are the final scores in the MS Quality Of Life (MSQOL-54 items) questionnaire, generally also rose by 22.68 and 24.56%, respectively. Moreover, the changes in serum high sensitivity C-Reactive Protein (hs-CRP) during 12-month intervention period has been shown in (Figure 1) (63.85 % reduction from baseline).
Discussion
Significant effects of 12-month MeD & synbiotic intervention in five SPMS patients was reported in this case series. Serum inflammation, fatigue severity and disability were dominated and QOL recovered.
SPMS is a rare type of MS with severe consequences that have not any specific treatment, however, our intervention lowered EDSS in these cases. Kouchaki et al. reported a reduction of 0.3 ± 0.6 in EDSS and 1.3 ± 3.5 mg/l hs-CRP; five probiotic (Lactobacillus acidophilus, Lactobacillus casei, Bifidobacteriumbifium and Lactobacillus fermentum, each 2 × 109) were administered for 12 weeks [7]. In another study conducted by Tankou et al., VSL3 containing high dose (900 billion) Lactobacillus, Streptococcus, and Bifidobacterium species twice a day for 2 months decreased frequency of inflammatory markers and corrected dysbiosis [8].
Presence of high-dose prebiotics, as a critical fuel for probiotics, is a key point in MeD [9]. Schwingshackl et al. in a meta-analysis showed that MeD has positive effects on inflammatory markers [10]; a major part of this effect is probably related to efficient omega-3 fatty acids content [11] and calorie restriction [12].
To the best of our knowledge, these cases are first report suggesting the potential effects of long-term MeD & synbiotic supplementation on SPMS disability, however, there are conflicting results to ours too. Riccio et al. in a 7-month clinical trial with four intervention protocol (one of them was MeD) expressed a reduction in systemic inflammation, but they did not see any significant changes in fatigue, EDSS and QOL of MS patients [13].
The synergism effects of MeD and Synbiotics in this report is amazing, so clinical trials would be performed in this format; though the management of SPMS cases is difficult.
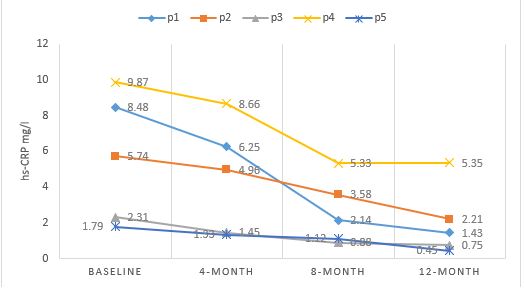
Figure 1: Changes in hs-CRP concentration during intervention (hs-CRP, high sensitivity C-reactive protein; p, patient. As you see, 12-months synbiotic supplementation resulted in a downward trend for hs-CRP concentrations).
|
Patient* |
Medical treatment |
Age (y) |
Disease duration (y) |
EDSS |
FSS |
PHCS |
MHCS |
||||||||||||
|
baseline |
4-month |
8-month |
12-month |
baseline |
4-month |
8-month |
12-month |
baseline |
4-month |
8-month |
12-month |
baseline |
4-month |
8-month |
12-month |
||||
|
1 |
Vit E 100 IU BID Vit D 50000 IU every month B complex tab QD Duloxetine 20 mg QD Celecoxib 200 mg QD Baclofen 10 mg QD |
31 |
12 |
4.5 |
4.5 |
4 |
3.5 |
58 |
43 |
40 |
37 |
33.8 |
39.7 |
51.8 |
56.1 |
50.4 |
59.2 |
63.8 |
67.7 |
|
2 |
36 |
8 |
3.5 |
3.5 |
3.5 |
3 |
46 |
38 |
35 |
35 |
44.8 |
49.8 |
50.1 |
55.5 |
61.3 |
67.4 |
65.8 |
69.7 |
|
|
3 |
37 |
10 |
4 |
4 |
2.5 |
2.5 |
45 |
41 |
34 |
29 |
43.7 |
45.2 |
46.1 |
49.7 |
48.8 |
55.1 |
59.3 |
70.1 |
|
|
4 |
30 |
6 |
5 |
5 |
4.5 |
4 |
40 |
36 |
36 |
33 |
36.3 |
38.4 |
39.2 |
46.6 |
54.1 |
59.2 |
59.6 |
60.5 |
|
|
5 |
39 |
9 |
3.5 |
3.5 |
2.5 |
2 |
60 |
55 |
47 |
39 |
50.7 |
52.4 |
62.8 |
62.8 |
61.4 |
66.6 |
69 |
75.8 |
|
|
*none of patients had not any familial history of MS. 1,2 were male; three others were female. Vit, vitamin; BID, twice a day; QD, once a day; EDSS, extended disability status scale; FSS, fatigue severity scale; PHCS/MHCS, physical/mental health composite score. |
|||||||||||||||||||
Table 1. Clinical findings at baseline and 4/8/12 month after intervention.
Citation: Moravejolahkami AR and Chitsaz A (2019) Mediterranean-Style Diet Co-Supplemented with Synbiotics Improved Quality of Life, Fatigue and Disease Activity in Five Secondary Progressive Multiple Sclerosis Patients. Ann Med & Surg Case Rep: AMSCR: 100006.