Annals of Pediatrics and Child Care
Medullary Ischemic Infarction in an Extreme Premature Newborn
Clara Schori-Fortier1, Corinne Boyer1, Etienne Berard1,2 and Sergio Eleni dit Trolli1*
1Neonatal Intensive Care Unit Archet II Hospital, Nice Universitary Hospital, Nice, France
2University of Nice, Nice, France
Corresponding author: Eleni dit Trolli S, Neonatal Intensive Care Unit, Nice Universitary Hospital Archet II, 151, Route de Saint Antoine de Ginestière, 06200 Nice, France, Tel: +33492036436.
Citation: Schori-Fortier C, Boyer C, Berard E, Eleni dit Trolli S (2019) Medullary Ischemic Infarction in an Extreme Premature Newborn. Ann Pediatr Child Care: APCC-100004.
Received Date: 20 March, 2019; Accepted Date: 11 April, 2019; Published Date: 24 April, 2019
Abstract
A neonate, born at 26 gestational weeks displayed an acute paralysis in his upper body and diaphragm. These symptoms are caused by a medullary infarction, a rare pathology in the premature newborn of undetermined cause.
Keywords: Flaccid paralysis; Ischemic stroke; Preterm; Thoracic spinal cord
Case Report
A premature newborn presented with a sudden acute flaccid paralysis of both arms and diaphragm at 22 days of life. He was born after a spontaneous uneventful bichorial biamniotic twin pregnancy, by cesarean section at 26 weeks of gestation in tertiary perinatal center in a context of premature rupture of the membranes and failure of tocolytic treatment. There was no consanguinity. He weighed 880 g and clinical examination, including neurologic exam, was normal. He was transferred in the NICU for a respiratory distress syndrome requiring double administration of exogenous surfactant and mechanical ventilation assistance. During the first three weeks of life, hemodynamic was stable. He remained under mechanical ventilation because of a patent ductus arteriosus unsuccessfully treated by two courses of Ibuprofen, and progressive evolution towards bronchopulmonary dysplasia. Cerebral ultra-sound performed at day 3, 7 and 21 of life was normal. Suddenly, at 22 days of life, he presented an are flexic flaccid paralysis of both arms and neck, disappearance of suction reflex with tongue fasciculations, and absence of spontaneous respiratory movement. Somesthesic sensibility of both arms was preserved, as well as spontaneous mobility of lower limbs. The next day, brain and medullary MRI scan showed a T1 hypersignal from the inferior extremity of the bulb to the thoracic spine, with an hemorrhagic transformation of an ischemic infarct in the anterior spinal artery territory (Figure 1 and Figure 2). Otherwise no lesion was found on the cerebral parenchyma. There was no coagulation disorder (prothrombin 91%, activating clotting time 1.13 and fibrinogen 4.13 g/L). The cause of this medullary infarction could not be determined. He died 4 days later from cardio-respiratory failure. His sister had an uneventful development.
To our knowledge, only 2 cases of infarction in low cervical spinal cord have been reported in term newborns. First child could not be weaned from the ventilator, and a tracheostomy was performed at 2 months old, he deceased at 5 months old. Second child was discharged from the hospital on nasal oxygen at 6 weeks complicated when 4 months old by an acute respiratory failure and he died just before 5 months old. The autopsy revealed lesions within the anterior and posterior spinal artery such as pseudo-calcification, peri-vascular fibrosis and sclerosis or an obliteration of specific vessels [1].
Some publications report on such pathology in other localisation but in the context of arterial hypotension [2], perinatal anoxo-ischemia [3]. In another case, lower medullar lumbar infarction was related to the use of umbilical arterial catheter and obstruction of the Adamkievicz’s artery [4]. In our observation, vascular steal in ascendant aorta caused by patent ductus arteriosus could be the cause of the medullary infarction.
This research provides a framework for the exploration of this rare lethal pathology in newborn. Medullary infarction must be considered when facing a flaccid paralysis of both arms associated with diaphragmatic paralysis. Such clinical presentation needs a cerebro-spinal MRI to exclude other treatable etiologies of spinal cord lesions.

Figure 1: Cerebro-spinal MRI (sagittal plan): T1 hyper signal of the inferior extremity of bulb to thoracic spine.
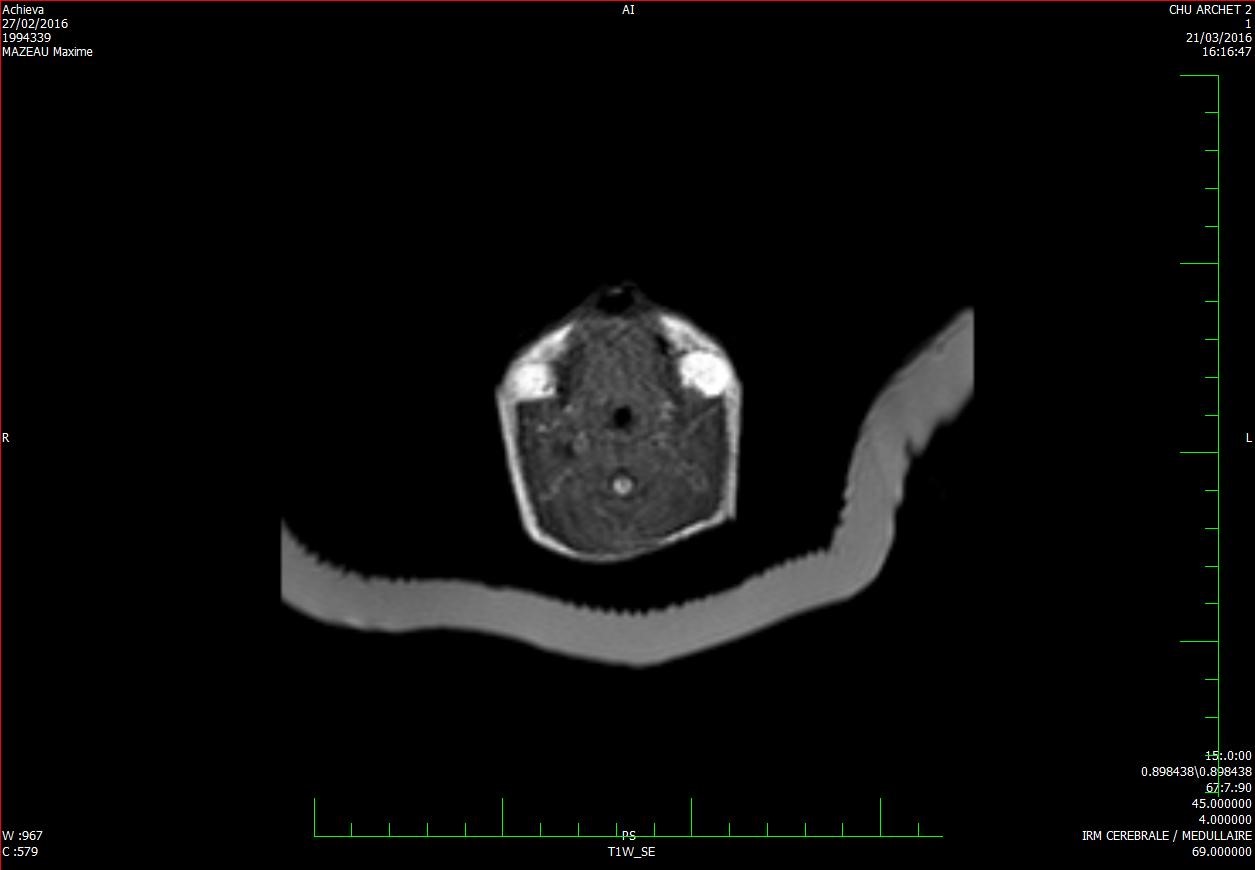
Figure 2: Cerebro-spinal MRI (transverse plane): T1 hyper signal of the bulb.
Citation: Schori-Fortier C, Boyer C, Berard E, Eleni dit Trolli S (2019) Medullary Ischemic Infarction in an Extreme Premature Newborn. Ann Pediatr Child Care: APCC-100004.