Insights of Cardiology Open Access
Geographical Diversities in Symptoms, Actions and Prehospital Delay Times in Swedish ST-Elevation Myocardial Infarction
(STEMI) Patients: A Descriptive Multicenter Cross-Sectional Survey Study
Isaksson RM1,2*, Sederholm-Lawesson S2, Thylen I2, Swahn E2, Hellström Ängerud K3, Karlsson J-E2,4
1Department of Research, Region Norrbotten County, Luleå, Sweden, and Division of Nursing Sciences, Department of Medical and Health Sciences, Linköping University, Sweden.
2Department of Cardiology and Department of Medical and Health Sciences, Linköping University, Linköping Sweden
3Department of Cardiology, Heart Centre and Department of Nursing, Umeå University, Umeå, Sweden
4Department of Internal Medicine, Region Jönköping County, Jönköping, Sweden
*Corresponding author: Rose-Marie Isaksson, Department of Research, Region Norrbotten County, Luleå, Sweden, and Division of Nursing Sciences, Department of Medical and Health Sciences, Linköping University,
Robertsviksgatan 7, S-971 89 Luleå, Sweden, Tel: +4613281000.
Citation: Isaksson RM, Sederholm-Lawesson S, Thylen I, Swahn E, Hellström Ängerud K, et al. (2019) Geographical Diversities in Symptoms, Actions and Prehospital Delay Times in Swedish ST-Elevation Myocardial Infarction (STEMI) Patients: A Descriptive Multicenter Cross-Sectional Survey Study. Insights Cardiol Open Acc: ICOA-100001.
Received date: 20 February, 2019; Accepted date: 11 March, 2019; Published date: 18 March, 2019
Abstract
Background: Geographical variations in cardiovascular mortality have been reported in Sweden as well as in other countries. Little attention has been given to possible variations in symptoms, actions and pre-hospital delay times in ST-elevation myocardial infarction (STEMI) patients, as a reason for this diversity. We aimed to study whether STEMI patients from the northern and southern parts of Sweden differ in symptoms and actions that may affect the pre-hospital delay times.
Methods: SymTime was a multicentre cross-sectional survey study where STEMI patients admitted to the coronary care unit completed a validated questionnaire within 24 hours after admission. In total, 531 patients were included, 357 in the southern and 174 in the northern part of Sweden.
Results: There were no significant differences in age. However, patients in the north had more often hypertension (52 vs 42%, p=0.02) or other concomitant comorbidities (24 vs 14%, p=0.01). Patients in the south experienced more anxiety (14 vs. 7%, p=0.01) and fear (23 vs. 14%, p=0.02) and more often contacted the emergency medical services (EMS) as first medical contact (FMC) (54 vs 44%, p=0.05). There were no differences in other main or associated symptoms or in pre-hospital delay times.
Conclusions: Patients with STEMI in the southern vs. the northern part of Sweden had more anxiety and fear, despite that they were less often alone at onset of symptoms. There were no differences in pre-hospital delay times. Although patients from the southern region contacted EMS as their FMC more frequently, it is still worrying that too few patients utilize the EMS.
Keywords: Actions; Geography; Pre-hospital delay; Symptoms; ST-elevation myocardial infarction.
Abbreviations
CAD : Coronary Artery Disease;
EMS : Emergency Medical Service;
FMC : first medical contact;
IQR : Inter Quartile Rate;
MI : Myocardial Infarction;
NRS : Numeric Rate Scale;
NSTEMI : Non ST-Elevation MI;
PPCI : Primary Percutaneous Coronary Intervention;
STEMI : ST-Elevation Myocardial Infarction.
Background
In Sweden, as in most other western countries, coronary artery disease (CAD) is the leading cause of death [1,2]. It is well known that the rapid identification and treatment in ST-elevation myocardial infarction (STEMI) reduces mortality and morbidity and improves cardiac function [3]. Patients who are treated within preferably 60 minutes, and at the latest within 90 minutes from onset of symptoms, have considerably lower mortality rates and reduction in infarct size compared with those treated later [3]. Consequently, the importance of seeking medical treatment promptly is crucial for patients experiencing a STEMI [4].
Different factors have been associated with prolonged pre-hospital delay, such as different sociodemographic-, clinical-, situational- and psychological factors [5-8].The pre-hospital actions also depend on the individual’s beliefs and attitudes to symptoms. Therefore, it is crucial that patients interpret symptoms correctly, as delays will affect care-seeking behavior and jeopardize early revascularization.
Geographical variations in cardiovascular risk factors and mortality have been reported in Sweden as well as in other countries [9-13]. However, little attention has been given to possible geographical variations in symptoms, actions and pre-hospital delay times in STEMI patients, as a possible reason for the geographical diversity in geographical cardiovascular mortality. Therefore, further studies are needed to investigate if there are differences in patients’ interpretations of symptoms, patients’ actions, pre-hospital delay times and start of prompt and effective reperfusion therapy in relation to whether patients live in urban or rural areas. The aim of this study was to study whether patients with STEMI from the northern part vs. the southern part of Sweden differ in respect to symptoms and actions that may affect the pre-hospital delay times.
Methods
Setting
Sweden has a population of 10 million and an area of 400000 km2. This study covers geographically large parts of Sweden. Northern Sweden covers more than half of Sweden but contains only 1/9 of the population, where there are a few large population centers by the coast with huge, sparsely populated areas in the inland [10]. As shown in Figure 1, the southern part is much more densely populated. Out of 69 hospitals in Sweden with acute MI care, 28 have catheterization laboratory facilities. Primary percutaneous coronary intervention (PPCI) is the reperfusion therapy chosen in 93% of STEMI patients. Thrombolysis is still used in rural areas with long transport distances as in northern Sweden [9,13].
Material and Methods
This Swedish multicenter study (SymTime) is described in detail in a previous publication [14]. To summarize, acute STEMI patients were included at the coronary care unit within 24 hours after admission during the time period November 2012 to January 2014. Two university hospitals and three county hospitals, all with catheterization facilities, included patients. The hospitals were selected to represent a wide geographical distribution and different types of hospitals.
Inclusion criteria were: (1) STEMI diagnosis according to ESC guidelines [15]. (2) Ability to fill in the questionnaire (3) Willingness to participate. Patients having difficulties reading and speaking Swedish were excluded. Patients were free from pain and hemodynamically stable when they were asked to participate. A previously validated self-administered questionnaire was used to access self-reported data. That questionnaire has both multiple choices and yes or no answers and has been described previously [14]. In addition, the staff nurse in charge obtained clinical data e.g. information on diagnosis, important time point measurements, culprit-lesion, first medical contact (FMC) and comorbidities from the medical records. FMC was defined as the time point when the patient first contacted the health care system. The FMC includes Emergency Medical Service (EMS), the primary health care center or emergency room. In Sweden [16], as in other European countries [17], the general public has the opportunity to receive healthcare advice via telephone staffed by an advisement nurse 24/7. This service number, however, is intended for self-care advice and non-emergency illnesses. Patient´s pre-hospital delay was defined as the interval between “time of onset of symptoms” until FMC.
Statistical Analysis
Frequencies and proportions were used to describe the history of patients’ characteristics, clinical and contextual variables. Comparisons between patients from the northern vs. the southern part of Sweden were done with chi-square tests for categorical dichotomous variables, and with Student-T-test or Mann-Whitney test for continuous variables depending upon if they were normally distributed or not. Continuous variables were reported as means ± SD or median (25th-75th percentile) as appropriate. Logistic regression analyses were performed to explore the impact of distance and geography on the dependent variables. Statistical analyses were performed using SPSS software, V.22.0 (SPPS Inc, Chicago Illinois, USA) for Windows.
Results
According to the national quality register for myocardial infarction care, SWEDEHEART [18], 942STEMI patients were treated at the three hospitals in the southern region and 531 patients were treated at the two hospitals in the northern region during the study period. Out of these 357 patients (38%) were included in the SymTime study in the southern region and 174 patients (33%) in the northern region.
Baseline characteristics
There was no difference in mean age between the participants in the southern and northern regions (65.9 vs. 65.0 years). The majority of patients were male, 76% and 77%, respectively. Most patients had less than 50 km distance to hospital, 85% in the south and 79% in the north (p=0.08). The two populations differed to some degree with respect to comorbidities: patients in the north had more hypertension (52 vs. 41%, p=0.02), higher prevalence of serious concomitant disease (24 vs. 14%, p=0.01), but lower prevalence of previous MI (8 vs. 15%, p=0.01) and chronic heart failure (0.6 vs. 4%, p=0.04). (Table 1)
Symptoms
There were no differences between patients from the two Swedish regions in main complaints where chest/thoracic pain was the most common symptom (88 vs. 90%, p=0.7). However, patients from the southern region experienced more anxiety (14 vs. 7%, p=0.02) and fear (23 vs. 14%, p=0.02). Symptom burden and intensity assessed by the questionnaire showed no differences between the two geographical regions. (Table 2)
Course of events
STEMI patients from the northern region were more often alone at onset of symptoms compared with patients from the southern part (34 vs. 23%, p=0.01). Self-medication with painkillers was more common in the south (20 vs. 11%, p=0.02). There were no differences between the regions with respect to FMC and main reason to go to hospital, but patients from the southern region contacted the EMS more frequently (54 vs. 44%, p=0.05). (Table 3)
Delay times
There were no differences in delay times from onset of symptoms to FMC between the southern and northern region (75 vs. 70 minutes, p=0.8) or to diagnosis (27 vs. 31 minutes, p=0.1). STEMI patients from the northern region more often received fibrinolysis therapy (30%) than patients in the south (<1%, p<0.001). (Table 4)
Discussion
The present study shows no differences in main or associated symptoms, or in pre-hospital delay times. It is well established that early diagnosis and reperfusion treatment of patients with STEMI is of utmost importance to reduce mortality and improve prognosis. Due to long distances in the north region thrombolysis is still used to follow guidelines. However, this body of research lacks detailed information on symptoms, and actions in relation to living in diverse geographical areas with different distances to hospital. In a recently published study from the northern part of Sweden, cholesterol levels were higher as well as body mass index (BMI) in the rural compared to the urban populations [9]. In the current study we could not see any differences in baseline characteristics between the northern and southern parts of Sweden, in spite of the southern part being more densely populated. However, we have no information about education, lifestyle, or the socioeconomic and cultural context.
Differences in MI symptoms in regard to gender, age and different co-morbidities have been found previously [19-22], but there is a lack of studies, which describe if symptom presentation differs based on the geographic area where the patient lives. In a recently published study from Germany, fear of death was more common in men than in women and shortened the pre-hospital delay in STEMI patients [23]. However, that study did not compare symptoms and actions from different geographical regions. In the present study we found that the most frequently reported symptom of STEMI was chest discomfort/pain, and it was equally common in patients in the two geographical regions. There were no major differences in associated symptoms except for anxiety and fear, which were more common among patients in the southern region. This was found despite the fact that patients in the northern region more often were alone at onset of symptoms. It is an interesting finding, but as this (to our knowledge) has never been described before we can only speculate that patients living alone in a rural part of Sweden feel more confident than those living in an urban area. Maybe because many people in the north live farther from medical services and thus are more used to taking care of themselves and hence feel more secure, even when they suffer from acute illness.
As shown in the annual report from the Swedish national quality register SWEDEHEART [13], the pre-hospital delay times are rather short. In the present study there were no differences in delay times from onset of symptoms to FMC and to diagnosis between the northern and southern parts of the country, in spite of the longer distance from the inhabitants to nearest hospital in the northern part of Sweden. This is in agreement with a study from Greece consisting of 348 patients with MI where there was no difference in decision time before seeking medical help for patients from urban vs. rural areas [24]. However, in that study both STEMI and non ST-elevation MI (NSTEMI) patients were included, which might make it difficult to compare the results. On the other hand, a study based on the GRACE registry suggested wide geographic variation in pre-hospital delay times in patients with STEMI [25]. Patients from South America had the longest delay times, 3.1 hours, whereas patients in North America and Australia/New Zealand had the shortest, 2.0 hours [25]. These results are similar to a study in Korea on factors associated with hospital arrival time in patients with ischemic stroke. The researchers found that patients who resided in rural areas were more likely to delay seeking medical help, and the longer decision time was associated with the failure to recognize symptoms as being serious [26].
One important difference in action was found in the present study. Patients from the southern region of Sweden contacted the EMS as FMC more frequently than those in the northern region (54 vs. 44%, p=0.05). However, there is cause for concern that in general, sofew patients called the EMS as their FMC. A prompt diagnosis with pre-hospital ECG and transfer to a primary PCI center is connected with a reduction in total ischemic time [27,28]. In Sweden, the general public has the opportunity to obtain healthcare advice via telephone, internet or a self-care guide booklet, and this national service number (1177) is provided by the county councils and regions [29]. Bray and coworkers have recently presented how mass media campaigns influence the pre-hospital behavior and result in shorter pre-hospital delay times [30]. In Sweden media campaigns have informed the general public about the possibility to contact 1177 instead of seeking immediate care at the EMS for non-life-threatening symptoms. This is worrying as we have shown in a previous study that STEMI patients who turned to Swedish Healthcare Direct (SHD) as FMC had 38 minutes longer delay from symptom onset to diagnosis than patients who called EMS [14].
We can only speculate about the reasons why STEMI patients in the southern region contacted EMS more frequently than those in the northern region. Patients in the southern region experienced more anxiety and fear and therefore contacted the EMS more frequently. Perhaps the county councils and regions in the south give more information to the citizens and/or have more media campaigns about SHD, which increases the patients’ fear and therefore affects the patients’ FMC. We must emphasize immediate contact with EMS to save lives in STEMI patients.
Limitations
The study has some limitations which may limit the generalizability of our results. Some patients were not hemodynamically stabilized and pain-free within 24 hours and were therefore not included in the study; this probably excluded the sickest patients. In addition, the questionnaire was only available in Swedish, which excluded non Swedish-speaking immigrants and could make comparisons with other studies difficult. Despite these limitations this study offers a new insight into whether STEMI patients from different geographical areas may differ in in symptoms and actions that might affect pre-hospital delay times.
Conclusions
Patients with STEMI in the southern part of Sweden had more anxiety and fear and contacted the EMS as FMC more frequently compared with patients in the northern part of Sweden, but there were no differences in other symptoms or pre-hospital delay times. It is worth noting that there were no differences in pre-hospital delay times despite long distances to hospitals in northern Sweden. However, delay in seeking medical care is still a problem among STEMI patients, and further improvement is required. Patients from the southern region contacted EMS as FMC more frequently, although too few patients used EMS as FMC.
Declarations
Ethics, consent and permissions
Permission for the study was obtained from the regional Ethical Review Board, Linköping, Sweden (D-nr 2012/201-31) and complied with the Declaration of Helsinki 17. Informed consent was obtained from all included patients.
Consent for publication
Not applicable.
Availability of data and material
All data generated or analysed during this study are included in this published article and its supplementary information files.
Competing interests
The authors declare that they have no competing interests
Funding
This work was supported by the Medical Research Council of Southeast Sweden (FORSS, grant number 161061), the Faculties of Medicine, Linköping and Umeå Universities. The Region of Norrbotten.
Author’s contributions
RMI, SSL, IT, ES and KHÄ contributed to the study planning, design, preparation, validation of the slightly modified questionnaire. RMI, KHÄ and SSL contributed to the data collection. SSL and JEK carried out statistical analysis. RMI drafted the initial manuscript. RMI and JEK revised the manuscript. All authors read and approved the final manuscript.
Acknowledgement
The authors hereby acknowledge all participating patients and the staff att all participating hospitals who included patients on daily bases. We especially acknowledge Elisabeth Logander the highly skilled nurse at Linköping University Hospital who supported the study group throughout the project.
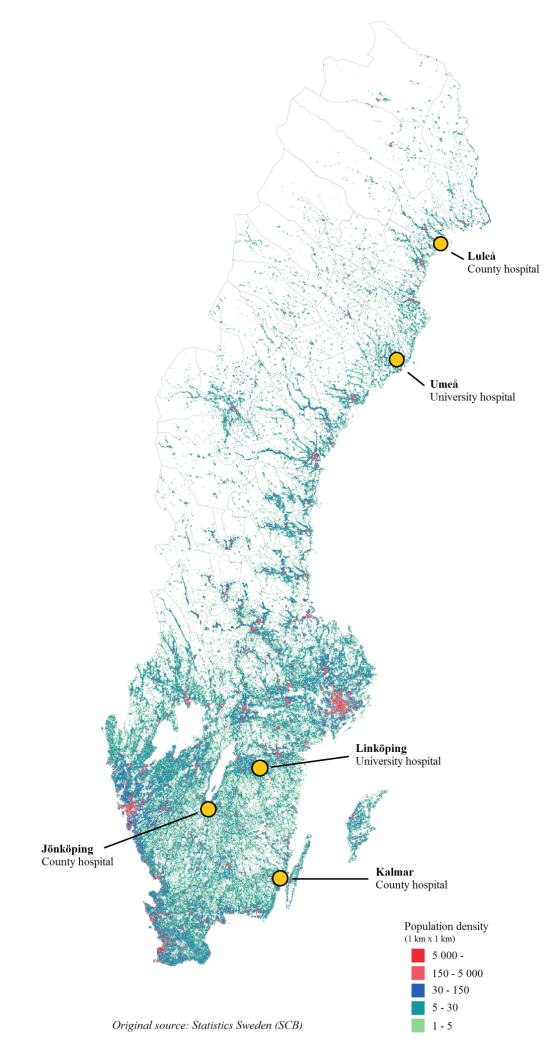
Figure 1: Population density with the five PCI-centres marked on the map.
|
|
South n=357 |
North n=174 |
p-values |
|
Demographics |
|||
|
Age, mean * |
65.9 (11.5) |
65.0 (1.0) |
0.4 |
|
Gender, male |
271(76) |
134 (77) |
0.8 |
|
Distance to hospital, ≥50?km |
52 (15) |
36 (21) |
0.08 |
|
Marital status |
|||
|
Single |
84 (24) |
38 (22) |
0.7 |
|
Educational level |
|||
|
Compulsory school |
145 (41) |
62 (36) |
0.5 |
|
Smoking habits |
|||
|
Current Smoker |
86 (24) |
39 (22) |
0.3 |
|
Clinical history |
|||
|
Hypertension |
148 (42) |
91 (52) |
0.02 |
|
Diabetes |
45 (13) |
29 (17) |
0.2 |
|
Previous myocardial infarction |
56 (16) |
14 (8) |
0.01 |
|
Previous stroke |
9 (3) |
4 (2) |
0.9 |
|
Atrial Fibrillation |
17 (5) |
9 (5) |
0.9 |
|
Chronic Heart Failure |
13 (4) |
1 (1) |
0.04 |
|
Angina Pectoris |
51 (15) |
19 (11) |
0.3 |
|
Other serious concomitant disease, like renal failure and rheumatic diseases |
50 (14) |
41 (24) |
0.01 |
|
Data are presented as numbers (percentages) if not otherwise indicated. *Data are presented as mean (SD). |
|||
Table 1: Baseline characteristics
|
|
South n=357 |
North n=174 |
p-values |
|
Main complaint, pain/discomfort |
|||
|
Chest/thorax |
315 (88) |
156 (90) |
0.7 |
|
Throat/neck |
76 (21) |
38 (22) |
0.9 |
|
Cheek/teeth |
43 (12) |
27 (16) |
0.3 |
|
Back |
52 (15) |
32 (18) |
0.3 |
|
Stomach |
31 (9) |
12 (7) |
0.6 |
|
Shoulders |
61 (17) |
41 (24) |
0.1 |
|
Arms/hands |
190 (53) |
106 (61) |
0.1 |
|
Associated symptoms |
|||
|
Tiredness/fatigue |
120 (34) |
58 (33) |
1.0 |
|
Weakness |
143 (40) |
68 (39) |
0.9 |
|
Dyspnea |
113 (32) |
58 (33) |
0.7 |
|
Vertigo/pre-syncope/syncope |
89 (25) |
48 (28) |
0.5 |
|
Nausea/vomiting |
116 (33) |
63 (36) |
0.4 |
|
Diaphoresis |
214 (60) |
115 (66) |
0.2 |
|
Anxiety |
51 (14) |
12 (7) |
0.01 |
|
Fear |
83 (23) |
25 (14) |
0.02 |
|
Symptom burden and intensity |
|||
|
Pain intensity, NRS, median (IQR)* |
7 (6-8) |
7 (6-8) |
0.3 |
|
Symptom burden, chief complaint, median (IQR)* |
2 (1-3) |
2 (1-3) |
0.1 |
|
Symptom burden, associated symptoms, median (IQR)* |
3 (2-4) |
3 (2-4) |
0.7 |
|
Interpretation of symptoms |
|||
|
Believed that symptoms came from the heart |
248 (69) |
107 (62) |
0.1 |
|
If answered yes – why? |
|||
|
Had a previous MI |
47 (19) |
13 (12) |
0.1 |
|
Had previous angina pectoris |
34 (14) |
9 (8) |
0.2 |
|
A friend/neighbor had MI |
35 (14) |
21 (20) |
0.2 |
|
A relative had MI |
81 (33) |
44 (41) |
0.1 |
|
Had read about MI |
88 (36) |
37 (35) |
0.9 |
|
Had got information in media about MI |
90 (37) |
41 (38) |
0.8 |
|
Informed by medical staff about MI symptoms |
27 (11) |
14 (13) |
0.6 |
|
Other source of information |
30 (12) |
19 (18) |
0.2 |
|
Data are presented as numbers (percentages) if not otherwise indicated. *NRS = Numeric Rate Scale (0-10). IQR = Inter Quartile Rate. |
|||
Table 2: Symptoms and interpretation of symptoms.
|
|
South n=357 |
North n=174 |
p-values |
|
Contextual factors |
|||
|
At home at onset of symptoms |
282 (79) |
125 (72) |
0.08 |
|
Alone at onset |
81 (23) |
59 (34) |
0.01 |
|
Self-medication |
|||
|
Aspirin |
23 (6) |
13 (7) |
0.7 |
|
Painkillers |
70 (20) |
20 (11) |
0.02 |
|
Nitroglycerin |
55 (15) |
18 (10) |
0.1 |
|
First consultation |
|||
|
Contact with relatives |
264 (74) |
131 (75) |
0.7 |
|
Contact with healthcare |
59 (17) |
25 (14) |
0.5 |
|
Main reason to go to hospital |
|||
|
Severe symptoms |
132 (37) |
72 (41) |
0.3 |
|
“thought I had a heart attack” |
83 (23) |
33 (19) |
0.3 |
|
“thought I suffered from a serious illness” |
9 (3) |
3 (2) |
0.6 |
|
“wasinstructed toseekmedical carefrom another person” |
67 (19) |
34 (20) |
0.8 |
|
Heard about reperfusion therapy |
331 (93) |
162 (93) |
0.6 |
|
First Medical Contact |
|||
|
Emergency Medical Services |
162 (54) |
64 (44) |
0.05 |
|
Swedish Healthcare Direct |
60 (20) |
33 (23) |
0.5 |
|
Primary Healthcare Centre (direct) |
23 (8) |
15 (10) |
0.3 |
|
Primary Healthcare Centre (telephone) |
16 (5) |
10 (7) |
0.5 |
|
Emergency room |
38 (13) |
23 (16) |
0.4 |
|
Transportation to hospital |
|||
|
Arriving by ambulance |
310 (87) |
133 (76) |
0.004 |
|
Prehospital reperfusion therapy |
|||
|
Fibrinolytic treatment |
1 (<1) |
52 (30) |
<0.001 |
|
Data are presented as numbers (percentages) if not otherwise indicated. |
|||
Table 3: Course of events
|
|
South n=357 |
North n=174 |
p-values |
|
|
|||
|
Patient delay time |
n=278 |
n=140 |
|
|
Symptoms onset to FMC |
75 (34 – 182) |
70 (32 – 176) |
0.8 |
|
|
|||
|
System delay time |
n=273 |
n=143 |
|
|
FMC to diagnosis |
27 (15 – 48) |
31 (16 – 63) |
0.1 |
|
|
|||
|
Total delay time |
n=341 |
n=169 |
|
|
Symptom onset to diagnosis |
108 (64 – 246) |
120 (68 – 233) |
0.5 |
|
FMC = First Medical Contact. Exact times are not available for all patients and therefore the numbers of patients differ between the groups. |
|||
Table 4: Delay times in minutes (25th – 75th percentiles)
Citation: Isaksson RM, Sederholm-Lawesson S, Thylen I, Swahn E, Hellström Ängerud K, et al. (2019) Geographical Diversities in Symptoms, Actions and Prehospital Delay Times in Swedish ST-Elevation Myocardial Infarction (STEMI) Patients: A Descriptive Multicenter Cross-Sectional Survey Study. Insights Cardiol Open Acc: ICOA-100001.