Annals of Medical & Surgical Case Reports
Senescence, Keratinisation, Latency: Seborrheic Keratosis
Anubha Bajaji
Histopathologist in AB Diagnostics, New Delhi, India
*Corresponding author: Anubha Bajaji, Histopathologist in A.B. Diagnostics, New Delhi, India.
Citation: Bajaji A (2019) Senescence, Keratinisation, Latency: Seborrheic Keratosis. Ann Med & Surg Case Rep: AMSCR: 100002
Received Date: 02 February, 2019; Accepted Date: 28 February, 2019; Published Date: 11 March, 2019
Preface: A benign epidermal tumour occurring primarily in the head and neck region, inter-scapular zone of the trunk, lateral area of the neck, face andextremities with the exception of palm and solescharacterizes the condition of seborrheic keratosis [1]. The terminology “Seborrheic” connotes lesions which appear waxy with a rough exterior surface. An estimated one fifth (20%) of the Caucasians above 50 years of age are implicated by the frequent disorder. Seborrheic keratosis incriminates the genders equally with a slight male predominance [1,2]. Subcategories of seborrheic keratosis depict the following order of appearance: a flat seborrheic keratosis (49%), dermatosis papulosanigra (42%) and the Leser Trelat sign (12%). Frequency of seborreheic keratosis concurs with location of the lesion. Theface (77.4%) is commonly implicated followed byback (32.3%) andabdomen (25.8%). An estimated one fifth (17%) individuals elucidate itching witha familial presentation of seborrheic keratosis(20%). Approximately three fourths (75%) instances clinicallydepicta skin photo type III [1,2]. The variant of dermatosis papulosanigra commonly implicates Fitz Patrick skin type VI [3].
Disease Characteristics: The disorder is of obscure origin, although lesions emerge with in sun exposed areas. Since the lesions are located within the intertriginous regions such as axillae and/or abdominal folds, exposure to sunlight is not culpable for each instance of seborrheic keratosis. Potential agents such as viruses, particularly Human PapillomaVirus (HPV) and genetic mutations additionally initiate the lesions [2,3]. A seven-point check list isemployedin order to evaluate the severity of lesions and it assigns specific scores to distinctive morphological attributes. Three crucial parameters for assessing a malignant conversion are a) modification within the dimensions of the lesion, b) an in constant perimeter and c) fluctuating pigmentation, where each of the parameter is assigned a score of 2 points. Minor factors such as inflammation, pruritus, a lesion magnitude of greater than 7 centimetres and crusting of lesion is assigned one point each. Acumulative score of greater than 3mandates a referral to a dermatologist. Scores as assessed with the check list depict a sensitivity of 73.3% and a specificity of 57.1% [3].
Clinical Elucidation: Lesions of seborrheic keratosis are composed of accumulated, senescent epidermal cells with an arrest in gap 1(G1) phase of the cell cycle. Apoptosis of squamous epidermal cells of seborrheic keratosis is inhibited by p16 (a cyclin dependent kinase inhibitor) [2,3]. Lesions classically represent as well-defined, round to oval, mildly elevated, thickened, flesh coloured to gray, light to brown or black patches and plaques. Several benign or malignant lesions or inflammatory eruptions emerge as thematic variations of seborrheic keratosis.As a technically benign disorder, determination of seborrheic keratosis requires a concordant histological confirmation. Lesions are pruritic, erythematous or generally irritating to the individual [4,5].
Morphological Patterns: Variable histology mandates the applicability of a diverse nomenclature such as a basal cell acanthoma, basal cell papilloma, benign acanthokeratoma, veruccaseborrhoica (seborrheic wart) and verruca senilis (senilewart). Brownish lesion selucidate averuccous surface with a distinct perimeter and minimally raised edges, in contrastto the surrounding skinand depict a typical “stuck on or coin like” configuration [1,2]. A plethora of histological patterns are delineated particularly theirritated type, adenoid or reticulated type, clonal, melano-acanthoma, inverted follicular keratosis and benign squamous keratosis. A targetoid appearance is exceptional. The subtypes comprehensively exhibit hyperkeratosis, acanthosis and papillomatosis. Seborrheic keratosisin frequently exhibits a sebaceous differentiation. Seborrheic keratosis depicts the following morphological subcategories:
Histological Elucidation: Basaloid cells with admixed, variable quantities of squamoid cells are exemplified. Surface invaginations with impacted keratinand miniature cysts (horn cysts) are frequently discerned. An estimated one third (33%) of lesions appear to be hyper-pigmented. Histological variations of seborrheic keratosisarenumerous with categoricalsubtypes. Acanthotic, hyperkeratotic, adenoid, reticulated, clonal, irritated, desmoplastic, inverted follicular keratosis andmelano-acanthoma subcategories are encountered on histology [1,2]. Microscopic attributes of hyperkeratosis, acanthosis and papillomatosis are elucidated within the subclasses. Focal trichilemmal differentiation along with glycogen rich cells, acantholysis with basal clear cells and foci of sebaceous differentiation comprise of exceptional variations. Additionally, pseudo-rosettes and adamantinoid subtypes configure as contemporary variants of seborrheic keratosis [6,7] (Figure 1-12).
Molecular modifications: Genetic modifications are incriminated in the evolution of seborrheic keratosis. Fibroblast growth factor receptor3 (FGFR3) is crucial for the progression of lesions. Mutations of FGFR3 gene are elucidated in majority (85%) of instances. Germ-line mutations of FGFR3 gene accompany malformations such as craniosynostoses and skeletal dysplasia [2,3]. PIK3CA gene with oncogenic properties are adjunctively associated with the disorder. Malignant tumours of colon, breast and bladder alternatively exhibit the PIK3CA gene. An estimated half (45%) of the lesions of seborrheic keratosis depict greater than one genetic mutation, commonly situated in oncogenes such as FGFR3, PIK3CA, KRAS or EGFR.Lesions may concur with the receptor tyrosine kinase/ phosphatidyl inositol -3- kinase / Akt signalling cascade, a pathway which is frequently elucidated with squamous cell carcinoma. Immobilization of Akt signalling pathway induces a cellular demise within seborrheic keratosis and eradicates the lesions [7,20].
Differential Diagnosis: Seborrheic keratosis necessitates a demarcation from several benign disorders such as papilloma, senile keratosis, keratoacanthoma and veruccous epidermal hyperplasia besides malignant lesions such as basal cell carcinoma or squamous cell carcinoma. Conversion toan in-situ squamous cell carcinoma (Bowenoid transformation) is an exceptional occurrence [8,21]. Sebaceous differentiation with in lesions of seborrheic keratosis is rare. Thus, a distinction from a sebaceoma with superficial alterations of verruca or classic seborrheic keratosis is required. Differentiation from associated tumours with sebaceous differentiation such as Trichoblastoma with sebaceous differentiation, sebocrine adenoma (apocrine poroma with sebaceous differentiation), superficial epithelioma with sebaceous differentiation, low grade sebaceous carcinoma and basal cell carcinoma with sebaceous differentiation is a pre-requisite [1,2].
Variant of sebaceoma with superficial verruca or seborrheic keratosis like alterations depicts a proliferation of in fundibular keratinocytes (basaloid cells or squamous cells) and is accompanied with focal hypergranulosis and segments of cornified cells (simulating verruca or a seborrheic keratosis) and intermittently admixed sebaceous cells. A sebaceoma is impinged upon upper ormid dermiswith augmented quantification of sebaceous cells instead of basal cells [20,21]. Thus, location and cellular composition of sebaceoma appears to be in contrast toseborrheic keratosis.
An appropriate contemporary terminology of “Sebomatricoma” isapplicable for benign neoplasm with sebaceous differentiation inclusive of seborrheic keratosis with sebaceous differentiation [1].A sebaceoma infrequently emerges in combination with seborrheic keratosis where lesions are constituted of dual and distinct, abutting tumours. A fore said components include seborrheic keratosis with hyperkeratosis, acanthosis and intermittent, irregular proliferation of seemingly benign basaloid and squamous keratinocytes along with miniature horn pseudo-cystsalong with a constituent of sebaceoma with characteristic multiple and varying lobules of immature sebocytes, commingled with solitary or assembled mature sebaceous cell units [21,22].
A trichoblastoma with sebaceous differentiation displays a multiplication of follicular germinative cells interspersed within a markedly fibrotic stroma and peripheral cellular palisade, contrary to the classic seborrheic keratosis. Mature sebocytes and sebaceous duct like structures are detected within basaloid aggregates [1].An apocrine poroma with sebaceous differentiation (sebocrine adenoma) illustrates a benign, cutaneous adnexal neoplasm, differentiating along the direction of sebaceous and apocrine glands. Sebaceous differentiation is manifested by singularly dispersed or aggregates of sebocytes and sebaceous ducts. Apocrine differentiation is discerned within basaloid clusters comprising of poroid and cuticular cells with accompanying tubular configurations [1,2].
Superficial epithelioma with sebaceous differentiation is an exceptional benign neoplasm. The histological variant occurs as multitudinous or solitary lesion emerging on the face, neck andtrunk ofgeriatric individuals. Circumscribed, well defined, plate like dissemination of basaloid cells are elucidated with several, extended adhesions to superficial epidermis. Tumour cells eventually blend with cellular epidermal covering, particularly at dermo-epidermal junction. Sebaceous cells are dispersed as miniature aggregates within the basal segment oftumour lobules. Minimal keratin filled cystic configurations are delineated with a lining of squamous epithelium, arising from epidermal or sebaceous ducts. Cellular peripheral palisade or retraction artefact from surrounding tissue is absent [21,22].
Low grade sebaceous carcinoma morphologically displays tumour cells of specific cytology with enlarged, compact, vesicular and pleomorphic nuclei containing conspicuous nucleoli. Particular cytological features are lacking in lesions of seborrheic keratosis. Exceptionally, basal cell carcinoma depicts foci of sebaceous differentiation. The tumefaction is distinguished from seborrheic keratosis by typical configuration of a cellular peripheral palisade accompanied by characteristic tumour cell cytology simulating a basal cell carcinoma. Stratified squamous epithelial hyperplasia is demonstrated along with acanthosis and basal cell proliferation besides interspersed keratin engendered horn and pseudo-horncysts andsebaceous differentiation confined to the deep seated lesions. The percentage of sebaceous cells are minimal, in contrast to basaloid cells, when compared to sebaceoma. Prominent fibrotic stroma devoid of a cellular peripheral palisade, duct like articulation orproliferation of basaloid cells recapitulating plate like configuration is enunciated. Exclusion of a forementioned entities is mandated in order to arrive at a diagnosis of seborrheic keratosis with sebaceous differentiation [23,24].
Although seborrheic keratosis with sebaceous differentiation does not conventionally elucidate the exceptional “Muir Torre Syndrome”, a benign, predominantly sebaceous or transitional squamous-sebaceous neoplasm is probably representative of the syndrome [1,2]. Malignant Manifestations: An abrupt emergence of innumerable lesions of seborrheic keratosis is scripted as a “Leser Trelat” sign. Leser Trelat sign indicates an internal malignancy, frequently an adeno-carcinoma of the stomach. Emergence of adjunctive malignancies such asacute or chronic leukaemia, bronchogenic carcinoma, breast carcinoma, colorectal carcinoma, renal cellcarcinoma, transitional cell carcinoma or anaplastic ependymoma is collated. Occasionally, Leser Trelat signiselucidated in the absence of an internal malignancy [2,3].
Multiple lesions of seborrheic keratosisare associated withan enhanced probability of innate or intrinsicmalignancy. Thus, conventional screening and consistent follow up of the implicated individuals is mandated. Leser Trelat sign is considered as a para-neoplastic sign. It typically manifests with an abrupt appearance and /or amplification of quantifiable seborrheic keratosis lesions. Leser Trelat sign is considered as an index of coexistent, underlying stomach, ovary, uterus or breast carcinoma and occasional instances of bladder, lung or laryngeal carcinoma [24,25]. Seborrheic keratosis is concordant with malignant disorders such as basal cell carcinoma, malignant melanoma, squamous cell carcinoma, keratoacanthoma, Bowen’s disease and eccrinecarcinoma. An estimated 5.3% subjects demonstrate the emergence of non-melanoma skin cancers with roughly 4.4% individuals depicting an intra-epidermal or squamous cell carcinomain situ followed by basal cell carcinoma (2.3%), invasive squamous cell carcinoma (2.3%) and malignant melanoma (2.3%) [26]. Malignant conversion cogitated in seborrehic keratosis with in situ and invasive tumefaction are induced on account of exposure to excessive sunlight or minimal quantities of chronic radiation or viruses such as Human Papilloma Virus (HPV). Bowenoid transformation may concur. Additionally, genetic mutation and over-expression of fibroblastic growth factor receptor 3 (FGFR3) are enunciated. Thus, activation of FGFR3 signalling pathway is contemplated as a cogent aspect of tumour induction [26]. Retrospective assay of previously diagnosed seborrheic keratosis enunciates a cumulative proportion of 6.4% of freshly detected malignant tumours. An early detection of seborrheic keratosis is crucial in order to achieve a reduced mortality. Investigative Protocol: Anaked eye, visual observation with appropriate illumination andfeeling the lesions imparts critical information. Suitably defined lesions with a flat, waxy, rough or verrucous surface are delineated [3,4].
A dermo scope is employed to confirm the appropriate diagnosis. Dermatoscopy is a precise modality to as certain the disorder with an estimated four times or greater sensitivity than a visual examination. TriageAmalgamated Dermatoscopic Algorithm (TADA) technique markedly enhances the percentage of confirmed diagnosis of benign lesions. A properly timed histological examination isa superior modality of demarcating betwixtbenign or malignant disorders. Dermatoscope was introduced in the year 1998 and exhibits a procedural sensitivity of 95.7% with a specificity is 78.3%. A blue black sign is diagnostic of malignant melanoma and demarcates it from seborrheic keratosis [3].
Therapeutic indications: Treatment is indicated for lesions which are inflamed, irritated, itchy or exceptionally painful on account of friction with clothes, razors or jewellery. Therapy is beneficial in an estimated one fifth (19%) of irritated lesions, cosmetic reasons (43%) and medical manifestations. Females patients and exposed lesions such as those on the face and/or neck necessitate therapeutic interventions [3,4]. Therapy is pre-requisite in suspected malignancy, concomitant with evaluation of site of lesion, pigmentation of lesion along with thickness and magnitude of lesion. Lesions situated in cosmetically sensitive regions benefit from conservative therapy. An estimated half (43%) of the seborrheic keratosis require eradication. Majority of individuals opt for decimation of the lesionon account of cosmetic indications. Irritation with consequent pruritus or haemorrhage during handling the benign, pigmented lesions necessitates a therapeutic intervention. Anomalies or an abrupt alteration in the outline, magnitude or co-existent inflammation of lesions or appearance of acute systemic symptoms benefit from conservative treatment. Probable malignant transformation requires a comprehensive elimination of seborrheic keratosis [1]. Topical modalities of treatment are considered as contemporary options [2,3].
Therapeutic options: Guidelines are lacking for optimal treatment of seborrheic keratosis. A comprehensive surgical excision is curative. Nevertheless, localized techniques of lesion eradication such as cryotherapy or curettage can be adopted [12,13]. Cryosurgery: An estimated two-thirds of dermatologists prefer cryosurgery. An outdoor technique devoid of topical anaesthesia, cryosurgery freezes squamoid seborrheic keratosis cells to a temperature of -2ºC to -30ºC or -4ºF to -22ºF. The cells are dehydrated and slough off. Duration of cryosurgical application of liquid nitrogen has not been defined. Liquid nitrogen is applied directly or with a cotton swab. Aberrant or flat lesions are alleviated with a singular application of liquid nitrogen for a period of 5-10 seconds [3]. Enlarged or thin lesions require numerous applications with freezing and thawing of cells. Minimal probability of infection, efficacious applicability and miniscule scarringaptly enumerates the advantages of cryosurgery. Oedema, erythema, diffuse or localized scarring and hypo-pigmentation within the sensitive regions ensues. Lesions adjacent to eyes and individuals with post inflammatory hyper-pigmentation prove to be contra-indications for cryosurgery. Ambiguous lesions which are susceptive of malignancy such as malignant melanoma, basal cell carcinoma and squamous cell carcinoma require an abstinence from techniques of freezing [3]. More than half (60%) the individuals opt for cryotherapy rather than curettage for eliminating the lesions, even though lesions treated with cryotherapy enunciate residual manifestations [24,25].
Focal Curettage of the lesions is performed efficaciously without anaesthesia. Minimal haemorrhage and healing occur with absence of scarring. Surgical elimination: A shave and/or biopsy of the lesion abets the preservation of tissue with histological elucidation of seborrheic keratosis. A well demarcated lesion, diagnostic of seborrheic keratosis does not benefit from a histological assessment, which can be deferred. Site, thickness and multiplicity of lesions dictates optimal therapeutic option [2,3]. Electro-surgery: Employment of electro-surgery with coagulation of lesions by electro-dessication or electro-cautery decimates miniature lesions with heat or cold point diathermy. Electro-dessication necessitates abutment of a Radio-Frequency (RF) electrode with the skin. Electro-fulgration damages superficial lesions with induction of “sparking “. Electro-cautery employs a red hot filamentto eradicate the lesions. Electro-surgery is the optimal modality for managing lesions of dermatosis papulosanigra.
Laser Therapy: Ablative (carbon dioxideor erbium- YAG) and non-ablative (755 nm alexandrite and 532 nm diode) formulations of laser are efficacious for eradicating seborrheic keratosis, though the outcome is inconsistent. As the therapy is devoid of guidelines, individual clinicians decide upon the intensity and duration of applicable laser therapy. Non-invasive treatment with Intense Pulsed Light (IPL) for seborrheic keratosis demonstrates a “disappearance” of lesions with afavourable outcome, particularly with miniature, superficial or thin lesions (an average of two cycles induces a de-pigmentation) and lack of secondary scarring or erythema [2,3].
Topical Agents: Contemporary novel, non-invasive topical applications or formulations which eradicate seborrheic keratosis with an absence of scarring, dys-pigmentation or infections are efficacious and effort lessly procured. A variety of topical options are available through the efficacy of many is questionable. Topical keratolytics are utilized for treating seborrheic keratosis. Formulation of Tazorotene (0.1%) localizes and adheres to retinoic acid receptors (beta and gamma) with consequent decline in proliferation of seborrheic keratosis cells along with reduction of inflammatory bio-markers. Tazarotene (0.1% cream twice daily) successfully disintegrate the lesions within two weeks [2,3]. Analogues of vitamin D elucidate functional effectiveness against seborrheic keratosis. Vitamin D receptors (VDR) modify differentiation and proliferation of keratinocytic cells. A hyper-proliferative reaction is elucidated within the epidermis with deficiency of vitamin D receptors. Therapeutic interference with vitamin D ligand reverts the aforementioned outcome and reduces cellular proliferation [24,25].
An estimated one third (30.2%) individuals demonstrate the decimation of an entire lesion or roughly 80% reduction of disease volume. Approximately half (46.4%) the instances depict a decline in the disease burden be twixt 40%-80%by adopting vitamin D analogues. The lesions can reoccur. Concentration of urea (50%) provides an adjunctive treatment option. Urea molecules function as a keratolytic and disturb the non-covalent cellular interaction, partially disrupt the proteinaceous matrix and remove superficial layer of seborrheic keratosis lesions. Subsequent scraping of lesions ensures appropriate cosmetic outcomes [23,25].
Benzyl peroxide isemployed in combination with a tertiary amine. The amalgamation configures the radicals of benzyl peroxide. Evaluation of results achieved with efficacious, topical treatment is currently insufficient. Lesions of seborhheic keratosis exceeding 2 centimetres in diameter and 0.3 centimetre in thickness are managed with a local, daily application of benzyl peroxide along with topical terbanafine (comprising of a tertiary amine). A declining magnitude of up to 50% within lesions of seborrheic keratosis is elucidated [2,3]. Topical concentration of hydrogen peroxide is employed as a contemporary therapeutic modality. Hydrogen peroxide (H2O2) engenders highly reactive oxygen species. Localized application of intensely concentrated molecules necessitates a careful monitoring. Reactive Oxygen Species (ROS) generated ensures a direct deterioration and termination of cells with apoptosis and necrosis of mutated squamoid cells of seborrheic keratosis. As the reactive oxygen species (ROS) additionally disrupts uninvolved cells, minimal injury is anticipated for healthy, normal skin circumscribing atypical lesions. Concentration of hydrogen peroxide (H202) frequently employed is at 3% and 30%. Topical application of concentrated hydrogen peroxide (H202) induces an irreparable dermal disruption. Concentrated liquid hydrogen peroxide (H202) is not a popular contemporary option [2,3]. An agent which has an approval from the foods and drug administration (FDA) is “Eskata” essentially constituted of a 40% formulation of hydrogen peroxide. The topical ointment is cogent in treating raised lesions of seborrheic keratosis.Conspicuous lesions of face and neck cogitate an adequate cosmetic outcome. Complications accompanying local administration include swelling of the lesion, stinging, itching, crusting, redness and scaling at the site of application. Topical treatment with solution A101 which is a 40% concentration of hydrogen peroxide (H2O2) exhibits an estimated lesion clearance with half (51.3%) the patients, particularly with the face, extremities and trunk. Facial seborrheic keratosis treated with A101 (40% hydrogen peroxide) depicts aclearance of roughly two thirds (65.3%) of the lesions. Adverse reactions such as hypo-pigmentation, hyper-pigmentation and scarring is minimal [3].
Topical formulation of potassium do besilate (5% cream) prohibits the activity of dermal fibroblast growth factor receptor 3 (FGFR3) in order to arrest the progression of seborrheic keratosis. Topical ointment of potassium dobesilate is beneficial in facial lesions. Side effects such as a reaction on the application site, skin atrophy, de-pigmentation or skin thinning are absent. The ointment is advantageous for application in cosmetically sensitive regions [3]. Non-Steroidal Anti-Inflammatory Drug (NSAID) such as a diclofenac gel as 3% concentration iseffective in removing the lesions. BL 5010 as a combination of aqueous tricholoacetic acid and formic acid can be employed. The topical formulation is applied with a pen like device in order to eradicate the lesions [3]. Formulations such as calcipotriene (0.005%) ointment and imiquimod (5%) cream do not provide suitable clinical improvement. Early in vitro trials of agents which inhibit the Akt such as A443654 and GSK 690693 are promising. Lesions treated with A443654 are extensively eradicated [7,8].
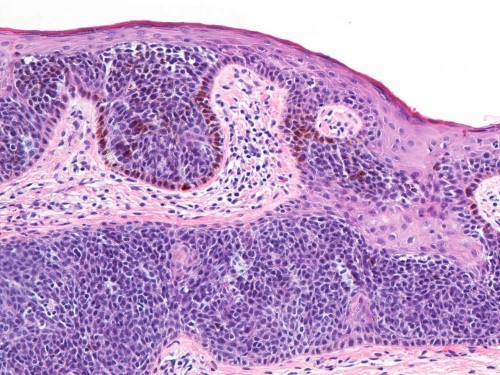
Figure 1: SK-clonal variant with plate like evolution [8].
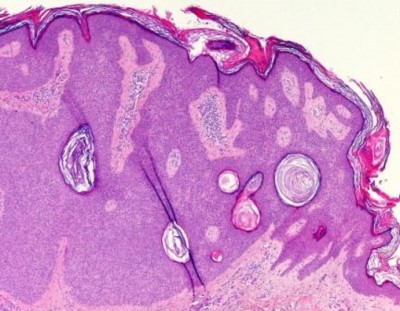
Figure 2: SK acanthotic variant with squamous cell prominence [9].
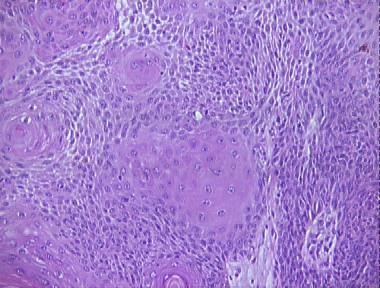
Figure 3: SK inflamed variant with infiltrated inflammatory cells within squamous cell nests [10].
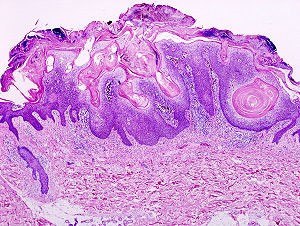
Figure 4: SK: keratincysts, pseudo-cysts and craters [11].
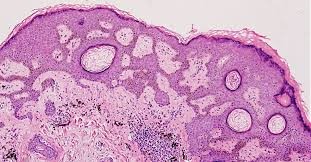
Figure 5: SK clonal pattern with reticulated squamou saggregates [12].
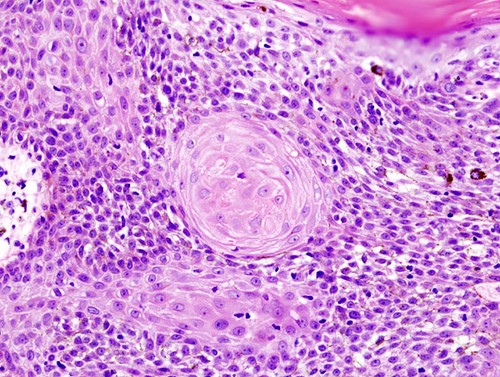
Figure 6: SK: Inflammatory ingress with keratin andcellular whorls [13].

Figure 7: SK invertedfollicular keratosis: with acanthotic squamous epithelium [14].
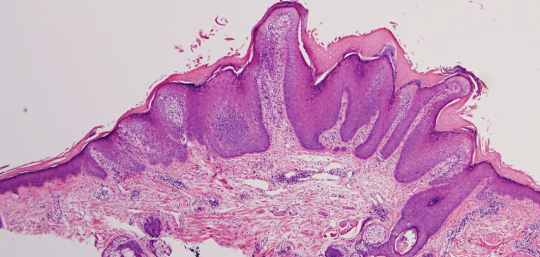
Figure 8: SK: acanthosis with a verrucous surface and hyperkeratosis [15].
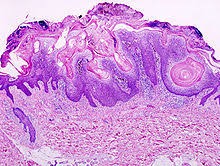
Figure 9: SK: Horn cysts with verrucous papillomatosis and hyper-orthokeratosis [16].
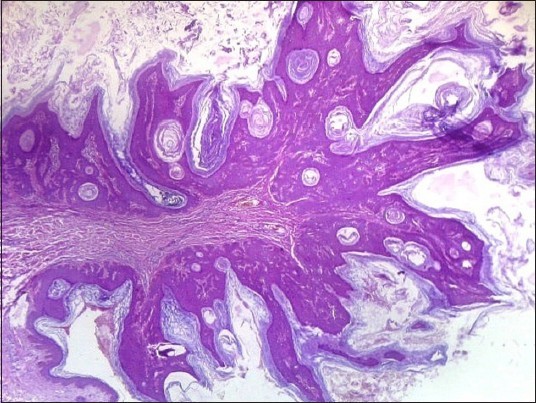
Figure 10: SK: Branching strands of basaloid and squamous cells [17].

Figure 11: SK: Acanthosishorn cysts andpseudo-horn cysts with orthokeratosis [18].

Figure 12: SK: Squamous papillomatosis with hyperkeratosis and parakeratosis [19].
|
Category of Skin |
Classical manifestations |
Tanning Ability |
|
I |
Pale white skin, Blue/ green eyes, Blond /red hair |
Always burns. Does not tan |
|
II |
Fair skin, blue eyes |
Burns easily, tans minimally |
|
III |
Darker white skin |
Tans after initial burn |
|
IV |
Light brown skin |
Burns minimally, tans easily |
|
V |
Brown skin |
Rarely burns, tans darkly easily |
|
VI |
Dark brown or black skin |
Never burns, always tans darkly |
Table 1: Fitzpatrick’s Photo-types of the Skin [3].
|
Malignant or Perpetual Lesions |
Benign Lesions |
|
Actinic keratosis |
Acrochordon ( skin tags) |
|
Bowen’s disease(SCC in situ) |
Acrokeratosisverruciformis |
|
Invasive SCC( SCC in situ) |
Benign lichenoid keratosis |
|
Lentigomaligna |
Condylomataacuminatum |
|
Malignant melanoma |
Ecrineporoma/ hidroacanthoma simplex |
|
Pigmented basal cells |
Melanocytic nevus |
|
Verruca vulgaris(warts) |
Solar lentigo(liver spots) |
|
Infundibulocystic basal cell carcinoma ( IFC-BCC) |
Tumour of the infundibulum |
|
SCC: Sqaumous cell carcinoma. |
|
Table 2: Differential Diagnosis of Seborrheic Keratosis [3].
References
Citation: Bajaji A (2019) Senescence, Keratinisation, Latency: Seborrheic Keratosis. Ann Med & Surg Case Rep: AMSCR: 100002