Dentistry and Dental Ailments Journal
Dentistry Point of View in the Obstructive Sleep Apnea and Snoring Patients: An Overview
Mohamed AM1,2*, Yan Yang3*
1Orthodontic Master Resident, Department of Stomatology, Zhongnan Hospital, Wuhan University, Wuhan, China
2 Demonstrator, Department of Dental Materials, Suez-Canal University, Ismailia, Egypt
3Professor of Orthodontics, Department of Stomatology, Zhongnan Hospital, Wuhan University, Wuhan, China
*Corresponding authors: 1. Abdelrahman Mohamed, Orthodontic Master Resident, Department of Stomatology, Zhongnan Hospital, Wuhan University, Wuhan, Hubei 430000, China, Tel: +8615549448756.
2. Yang Yan, Professor of Orthodontics, Department of Stomatology, Zhongnan Hospital, Wuhan University, Wuhan, Hubei 430000, China, Tel: +8613907172703.
Citation: Mohamed AM, Yang Y (2019) Dentistry Point of View in the Obstructive Sleep Apnea and Snoring Patients: An Overview. Dent Ailments J: DDAJ-100001
Received Date: 08 February, 2019; Accepted Date: 14 February, 2019; Published Date: 09 March, 2019
1. Abstract
1.1. Aim: This paper presents a narrative overview of the dentistry point of view to the Sleep apnea and snoring. In addition, to answer a question which is: can dental practitioners prevent or even improve the sleep apnea and snoring using oral appliances?
1.2. Methods: We used PubMed (https://www.ncbi.nlm.nih.gov/pubmed) to collect the data about this aspect using key words: Obstructive Sleep Apnea, Snoring, Oral Appliances.
1.3. Results and Conclusions: Oral appliances that can designed by dentist has proved as a useful line in the treatment of snoring and OSA with least side effect and noninvasive especially in a normal person with simple snoring without any systemic illness. Also, combining Oral Appliances with other line of treatment can provide a higher level of success than either used alone.
2. Keywords: Obstructive Sleep Apnea; Oral Appliances; Snoring
3. Introduction
Snoring is defined as a sound produced during sleeping when an individual breath due to the turbulence of air passing through the partially obstructed airway. It is considered as one of the most common simplest clinical symptoms of Obstructive Sleep Apnea (OSA) [1]. Snoring may result in excessive daytime sleepiness, loss of concentration, and psychological disturbances that may eventually cause deterioration of the patient life quality unless treated [2]. Sleep apnea and snoring is not a benign symptom. It is associated with an increased risk of hypertension, cardiac arrhythmias, and mortality [2].
Many craniofacial features and malocclusions were reported to be associated with snoring. For example; narrow airway at the level of the soft palate and oropharynx, more inferiorly positioned hyoid bone, more protruding maxilla, anterior-posterior discrepancy of maxilla and mandible, Class II malocclusion, increase in over-jet, narrower upper, and shorter lower dental arch and crowding in the mandibular arch [3-5]. Many treatments have been suggested for obstructive sleep apnea (OSA) which can be Continuous Positive Airway Pressure (CPAP), surgery or mandibular advancement by using oral appliances [6]. Shokri et al. [7] Compared the pharyngeal airway volume in different skeletal facial patterns using cone beam computed tomography, and they found that there are a significant correlation exists between the skeletal facial pattern and upper airway dimensions. The total airway volume and the mean airway area of class III patients were larger than those in class II patients. This may give idea of that correcting the underlying malocclusion can positively improve the airway volume and subsequently improve the Sleep apnea and snoring.
Another pilot study in 2018 made by Zhao et al. [8] to evaluate the impact of pediatric obstructive sleep apnea on the development of Class II hyper divergent. They found that: presence of OSA in pediatric patients has a vital effect on the development of hyper divergent malocclusions and early diagnosis and management of pediatric OSA patients can affect the orthodontic treatment outcome of them.
4. Aim
The aim of treatment obstructive sleep apnea and it is related snoring by the using of oral appliances designed by dentists is to improve the patient’s live and sleep quality as well as that of the relatives or roommates, by reducing or eliminating snoring and respiratory pauses during sleep.
5. Methods for Preparing the Review
We used PubMed Data base (https://www.ncbi.nlm.nih.gov/pubmed) to collect papers and data about this aspect using key words: Obstructive Sleep Apnea, Snoring, Oral Appliances.
5.1. Treatment Options for obstructive sleep apnea and / or Snoring
1. Surgical interventions (Invasive) [9].
2. Conservative noninvasive measures including:
a. Lifestyle modifications [10]
b. Drug control
c. Continuous Positive Airway Pressure (CPAP) [11].
d. Oral Appliances (OAs).
6. Discussion
Surgical intervention by adeno-tonsillectomy was the most common treatment for Obstructive Sleep Apnea (OSA) in childhood. Because of its surgical risks and recurrence that can be associated with craniofacial problems, there was a continuous searching for another line of treatment [12]. Using a drug as losartan and allopurinol for patients suffering from OSA in conjunction with other line of treatment can augment the effect of it specially in patient with raised blood pressure but can’t use as isolated treatment way [13].
Continuous Positive Airway Pressure (CPAP) considered as a gold standard treatment for OSA and snoring [11] but it is not well tolerated by patients, due to problems related with nasal airways, mouth leak and general discomfort from the mask and headgear [14,15]. Therefore, for these patients, other alternatives will be better. Oral appliance provides a non-invasive, non-permanent method for addressing the obstruction at specific points within the upper airway [16]. There are many designs of intraoral devices with different sites of action that shown an impact treatment efficacy [17,18]. Mandibular Advancement Devices (MADs) are more effective than other types of OAs [17,19] and are the most commonly used for treating OSA [17,20] Figure 1.
6.1. Mechanism of action of Mandibular Advancement Devices MAD
The American Sleep Disorders Association [21] defines MAD as a device introduced to the mouth and modifies the position of jaw, tongue and other supporting structures for the treatment of snoring and OSA. They considered it as a first choice in simple snorers, mild OSA cases, mild to moderate OSA with low body mass index, and patients suffering from the syndrome of increased resistance of the upper airway. Second choice for patients who do not improve or cannot tolerate positive pressure devices, patients at high surgical risk and who react badly to surgical treatment.
Mandibular advancement device MAD functions by protruding and stabilizing the mandible in order to maintain a patent airway during sleep [22]. As reported in previous studies, MAD advancement of mandible resulting in either of these actions:
6.2. Types of MAD
Studies support that custom made (adjustable) MAD are more efficient to prefabricated (nonadjustable) alternatives [26,27].
6.3. Efficacy
MAD is useful in reducing the obstructive sleep apnea and snoring, but with lower effectiveness compared with continuous positive airway pressure (CPAP) [26,28,29] and higher complain rate than CPAP [29,30]. Moreover, the custom-made MAD were more effective compared pre-fabricated one.
6.4. Side Effects
Usually mild and transient side effects that resolve within several days. It can be divided to two categories:
7. Conclusion
Mandibular advancement device MAD that can designed by dentist has proved as a useful device in the treatment of snoring and OSA with least side effect and noninvasive especially in a normal person with simple snoring without any systemic illness. Recent studies have suggested that combining MAD with CPAP and can provide a higher level of success than either used alone [32].



Figure 1: different designs of MADs.
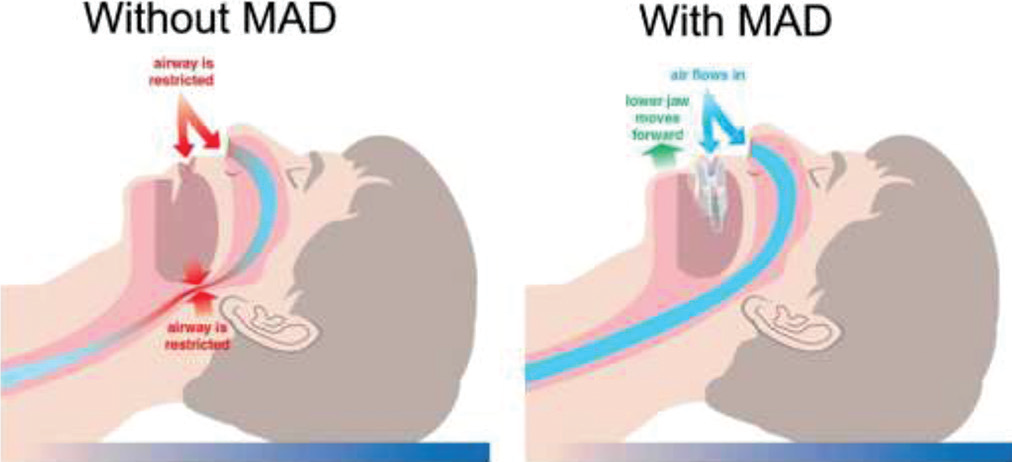
Figure 2: showing effect of MAD in Upper airway.
Citation: Mohamed AM, Yang Y (2019) Dentistry Point of View in the Obstructive Sleep Apnea and Snoring Patients: An Overview. Dent Ailments J: DDAJ-100001