Annals of Medical & Surgical Case Reports (ISSN 2652-4414)
Research Article
Vaginal Birth after Caesarean: The Local Experience of an Obstetric Unit in the Middle East
Shittu S, Athar S*, Koujan F, Rawamat J, Ramanunny M, Kassim S and Alansari L
Department of Obstetrics and Gynaecology, Al Wakra Hospital (AWH), Hamad Medical Corporation (HMC), Qatar
*Corresponding author: Dr Sufia Athar, Department of Obstetrics and Gynaecology, Al Wakra Hospital, HMC.
Doha, Qatar, Tel: +97433991773, E-mail: Sathar1@hamad.qa
Citation: Shittu S, Athar S, Koujan F, Rawamat J, Ramanunny M, et al. (2022) Vaginal Birth after Caesarean: The Local Experience of an Obstetric Unit in the Middle East. Ann Med & Surg Case Rep: AMSCR-100203
Received date: 13 March, 2022; Accepted date: 18 March, 2022; Published date: 25 March, 2022
Abstract
Background
There are universal social and professional concerns about the global increase in Caesarean section (CS) rates. Various approaches have been introduced to reduce it. For most women with previous CS, vaginal birth is possible. International guidelines highlight the importance of informative counseling. The overall success rate of vaginal birth after Caesarean (VBAC) is quoted at 72 -75%. Hence increasing the uptake of VBAC can help reduce the CS rate and morbidity and mortality associated with multiple repeat CS.
Objectives
The objectives of the audit are to assess the mode of delivery, success rate and outcome of the trial of vaginal delivery among pregnant women with one previous CS to improve the care of such women.
Method
A retrospective cohort study of 465 patients with one previous CS delivered between 1st of March to 30th September 2019 in the Al Wakra Hospital, Qatar, was done to establish local success rate and uptake rate of VBAC. Auditable standards in the RCOG and Hamad Medical Corporation guidelines were assessed and used for comparison.
Results
465 cases of women with one previous CS were reviewed. Our success rate was 73.8%, uptake rate was 40.2% and VBAC rate was 29.7%. The commonest indication for repeat CS was maternal request accounting for 43.12% of all CS. 7.43% (fifteen) of the women intending VBAC changed their mind during labour and had a CS. The successful VBAC group had the lowest number of complications. Two women undergoing VBAC had uterine rupture (1.0% risk), and their maternal and neonatal outcomes were satisfactory.
Recommendation
We recommend postnatal counseling of women regarding their suitability for VBAC in future pregnancy; Early use of epidural for those in labour and early referral to VBAC clinic for counseling and rigorous review of primary CS in the unit.
Conclusion
VBAC remains a safe and effective mechanism to reduce the CS rate in our clinical setting. Our good local result in terms of the safety and success rate is compatible with global data and can be used to guide decisions and improve VBAC uptake.
Keywords: Caesarean section; Vaginal delivery; VBAC; TOLAC; ERCS
Abbreviations
CS : Caesarean section
TOLAC : Trial of Labour After Caesarean
EMCS : Emergency CS
ERCS : Elective Repeat CS
IVD : Instrumental Vaginal Delivery
SVD : Spontaneous vaginal delivery
VBAC : Vaginal birth after Caesarean
HMC : Hamad Medical Corporation
Key Message
Introduction
Caesarean section (CS) is a surgical procedure that has positively influenced fetomaternal outcomes worldwide, with CS accessibility and outcomes serving as proxy measures of the availability of emergency obstetric services and healthcare quality in many parts of the world [1-2]. Although CS is considered a safe and beneficial procedure, it is not without anaesthetic and surgical risks for both the mother and child. CS is associated with increased healthcare costs in most countries, with the costs either borne by individuals or government health services [3-5]. As a result, there have been professional and public concerns regarding the rising rate of CS worldwide [6].
The increased rate of CS worldwide has led to a larger proportion of pregnant women having previous CS scar [7]. Comparatively, in Saudi Arabia, the CS rate increased from 10.6% in 1997 to 19.7% in 2006 [8]; while in the United States a rise from 23% in 2000 to 32% in 2015 was documented [9]. An increase from 19.7% in 2000 to 26.2% was reported in the CS rate for the United Kingdom [9]. Here in Qatar, the proportion of births by CS has steadily risen from 16.3% in 1998 to 29.8% in 2013 [16]. The increasing rate of CS is now among the most controversial themes in obstetric care worldwide because the increased rate of CS has not to be found to be associated with much more improved perinatal outcome [10,11].
As a result of its inherent health risks and financial implications on the health system, numerous authorities are publicly recommending a lower CS rate for a long time [12,13]. Several approaches are being suggested for this, mainly concentrating on limiting the number of planned CS. Previous CS is one of the most common indications for planned CS [14]. A previous CS has been cited as the primary indication in approximately 28% of planned Caesarean deliveries in the UK [10], and 30–50% in the USA [11].
Women who deliver vaginally after a previous CS are less likely to experience birth-related morbidity such as blood transfusion, ruptured uterus, unplanned hysterectomy, and admission to the Intensive Care Unit than women who have repeat CS [13]. Therefore, vaginal birth after caesarean (VBAC), being a safe and appropriate alternative for most women with one previous CS has been recommended as a practical mechanism of decreasing the CS rate. It is now established in clinical practice of many obstetric units worldwide and supported by the guidelines on both sides of the Atlantic including that of the Royal College of Obstetricians and Gynaecologists (RCOG) [13], the American College of Obstetricians and Gynaecologists (ACOG) [15] and Hamad Medical Corporation (HMC), Qatar.
Being that the success and uptake rate of VBAC show appreciable variations from one clinical setting to the other and VBAC is not without risks, it is essential to provide relevant information that helps the woman to make an informed choice after she has been assessed suitable for VBAC. This audit aims to evaluate our adherence to the RCOG and HMC guidelines and the outcome for women with one previous CS delivered in our hospital. The result will generate local data that would be useful for counselling and improve the clinical outcome of women with one previous CS and reduce CS rate particularly in our settings where it is the woman herself that chooses between VBAC or planned CS.
Methodology
We conducted a retrospective cohort analysis of 465 pregnant women with one previous CS delivered at Al-Wakra Hospital, Qatar from 1st of March to 30th of September 2019 to establish the success rate, uptake rate, and VBAC rate. The Al Wakra Hospital is the second-largest maternity public hospital in Qatar. This hospital receives approximately 6000 deliveries annually. Healthcare is accessible and free or subsidized for all citizens and residents in Qatar, with almost 90% of all deliveries conducted at public hospitals. In AWH, women with one previous CS have the right to choose VBAC or elective repeat CS.
Maternal electronic records were reviewed, and the study data were retrieved with a proforma (appendix a) and entered into a Microsoft Excel spreadsheet. Auditable standards in the RCOG and HMC guidelines were used for comparison as shown in Table 1. Women with more than one previous CS were excluded. Only women with one previous CS and singleton or twin pregnancies and with gestational age between 37 and 41wks were included in the study. We used the program of Medcalc online software Version 20.019 for data analysis. Odds ratio with 95% confidence interval (CI) was used to compare rates of complications between the successful VBAC group and those who had CS. Significant differences are identified when p < 0.05. Our study was approved by the institutional review board of Hamad Medical Corporation and the institutional review board number was HMC-IRB Reference: MRC -01-21/054
In our unit VBAC is offered to all suitable women with one previous CS after comprehensive counselling that explains the pros and cons of both VBAC and elective repeat CS (ERCS), and the patient is supported to make an informed choice. A thorough clinical assessment and a review of indication and note of the previous CS (if accessible) and sonographic evaluation of the fetus for presentation and estimated fetal weight are also done are done to recognize any contraindications to a trial of labour. Maternal consent is obtained before proceeding to a specific method of delivery. Those who opt for elective repeat CS are delivered using a daily elective CS list. Women who choose to have a trial of labour are offered a membrane sweep at term and encouraged to await the establishment of labour up until the woman is due for delivery or 40 weeks + 10 days with a view to provisional ERCS or induction of labour. When the patient is due for delivery, pelvic examination and membrane sweep or cervical ripening with Foley’s catheter or artificial rupture of membranes and use of Syntocinon are carried out based on the discretion of the labour ward consultant and patient’s consent. Our protocol does not allow induction of labour with prostaglandins in women with previous CS.
Labour was managed as per unit guidelines and the fetus was continuously monitored using cardiotocography throughout labour in all women having a trial of labour after Caesarean (TOLAC). No specific duration was set for a trial of labour and any decision for emergency CS was made by the labourward consultant based on the unit guideline.
Results
We had four hundred and sixty-five pregnant women with one previous CS delivered during the study period. 212(45.59%) had ERCS and 115(24.73%) had EMCS. 138 (29.68%) had vaginal delivery out of 187 that attempted VBAC (Figure 1). Of these 14(3.01%) and 8(1.72%) had ventouse and forceps deliveries respectively as shown in Figure 2. Table 1 shows our observed results in comparison to auditable standards of RCOG and HMC.
Definition of Relevant Rates
Documentation of counselling using the operation-specific counselling chart in the electronic record was 58% (270) and 65% (302) of the patients were seen before 36wks. All patients had CTG monitoring in labour and documentation of complications as appropriate. The success rate, uptake rate, and VBAC rates are as documented in table 1.
As shown in Figure 3, the commonest indication for repeat CS is maternal request as in 141 (43.12%) of cases while 15 women (4.69%) changed their mind while in labour making total cases of maternal request 156 (47.81%). Those that opted for VBAC but had CS without attempting VBAC at the time they were due for delivery for various reasons (e.g., postdate; diabetes and PET) formed the second largest group of 80 (24.46%). 15(4.69%) women changed their minds while in labour and 26(7.95%), 21(6.42%), and 20(6.12%) were cases of failure to progress, fetal distress, and short interval (less than two years) respectively. Breech and macrosomia were the indications in 7(2.15%) and 4(1.22%) cases. Miscellaneous cases like transverse lie, twins not suitable for vaginal delivery, antepartum haemorrhage, placenta previa, etc. were 13(3.98%).
Table 2 shows the various complications in each group based on their mode of delivery. The group that had successful VBAC (138) had the lowest complications being 4 cases of postpartum haemorrhage (PPH) needing a blood transfusion and 2 cases of third-degree perineal tear. The ERCS group (112) had one case of endometritis and 3 cases of PPH including one case of intra-abdominal haemorrhage that required another laparotomy. The EMCS group (115) had the highest number of complications- 8 cases of PPH including one that required laparotomy for anterior abdominal wall haematoma, 2 cases of endometritis, 2 cases of scar rupture with good maternal and neonatal outcome, 3 cases of scar dehiscence, one case of intraoperative bladder injury and one fetal scalp injury. There were no cases of HIE, intrapartum stillbirths, or Caesarean hysterectomy. However, the results were not statistically significant due to few cases in each group (p>0.05).
Discussion
Our audit showed good adherence to the HMC and RCOG guidelines even though there are areas for improvement. Of note is our success rate of 73.8%. This aligns with the RCOG standard of 72-75%. VBAC success rates are mostly estimated to be between 54 and 75% in the literature with the largest proportion of 84-90% in women with previous vaginal delivery [13-15]. 15.94% (22) of our patients with successful VBAC had instrumental vaginal delivery much less than 39% recorded by Hehir et al [17]. The advantages of a successful VBAC include maternal fulfilment after vaginal delivery, a greater chance of normal birth in the future, decreased maternal morbidity, decreased neonatal respiratory morbidity, easier breastfeeding, a reduction in the general CS rate, and cost of healthcare at the population level [13,15,18].
Our uptake rate of 40.2% is higher than the average national VBAC uptake rate of 8.0% in the USA in 2012 [19] and lower than 52.2% recorded in the UK in a 2014 study [20]. In many countries, the VBAC rate has been declining consistently, with an accompanying increase in the rates of ERCS. Reasons identified include clinicians’ perspectives, maternal choice, corporate and national guidelines, legal action, and insufficient quality evidence to guide women reliably [21-23]. Patients’ preference for CS was the main reason for the low uptake rate in our unit.
The VBAC rate varies significantly from country to country with 13.3% recorded for the US22 and 29-36% for Ireland and Germany and higher rates of 45-55% for Finland and Sweden.23 Our VBAC rate of 29.7% is relatively low because most of our patients suitable for VBAC opted for elective CS and even 15 (4.69%) that presented in labour changed their minds and opted for CS. Only one patient planning elective CS had a vaginal delivery. This finding highlights the need for us to improve antenatal counselling and reassurance regarding the safety of VBAC as only 58% of the patient had their counselling done with VBAC specific consent documents in the electronic record. The fact that only 80% of the patients were seen before 36 weeks could have contributed to this.
The two major risks of TOLAC are uterine dehiscence and rupture. In this audit, we had 3 cases of dehiscence and 2 cases of uterine ruptures and all had good outcomes. Uterine dehiscence occurs in 0-19/1000 TOLACs15, our 16/1000 (3 out of 187 TOLACs) was comparable. The rate is also comparable to that in women having ERCS. In contrast to dehiscence, uterine rupture occurs in approximately 0.7% of women with a prior CS [15]; our risk of 1.1 % (2 out of 187 TOLACs) was slightly higher. Uterine rupture is hard to foresee, and avert, and negative consequences can be fatal to both the mother and fetus [13-15]. We are cognizant of this in our unit and staff are trained to recognise the potential early signs of uterine rupture and provide appropriate early intervention. Our 2 cases of uterine rupture had very good maternal and neonatal outcomes. This reflects our adequate intrapartum monitoring of patients and ready access to the theatre when EMCS is indicated under general anaesthesia.
Sonographic evaluation of uterine scar thickness can be a useful tool for the prediction of uterine rupture when used in conjunction with other risk factors. In a cross?sectional validation study, Sarwar et al concluded that a cut?off value of ≤5 mm of uterine scar thickness, had a sensitivity of 76.9%, specificity of 48.7% and accuracy of 58.12% for prediction of uterine rupture and additional factors should be considered when choosing a mode of delivery [20].
A failed VBAC, leading to EMCS, has the most significant risk of complications which include bleeding, need for blood and blood products, uterine rupture, and endometritis. For the neonate, a higher risk of asphyxia or perinatal death [13,15,18]. The risks are lowest in the successful VBAC group as experienced in our unit (Table 3). Therefore, meticulous attention should be paid to the likelihood of vaginal birth for each woman. Hence, appropriate patient selection is essential to accomplish a high VBAC success rate with negligible risk of complications. Unfortunately, screening tools or models developed to predict VBAC success have not consistently identified women who may achieve successful VBAC [23]. The clinical use of currently available VBAC calculators is also discouraged [24,25]. However, several factors available to the obstetrician antenatally can help in selecting the most suitable patients. VBAC rate is highest in women with previous vaginal delivery (including the previous VBAC) and previous CS delivery for non-vertex presentation and women with spontaneous onset of labour [13,15]. A history of one or more previous vaginal deliveries is the ‘single best predictor of successful VBAC’ and is associated with success rates of 85-94% and a lower risk of uterine rupture [13]. Others include active labor settled at 40 weeks of gestation or less, fetus with weight <4,000 g and a favorable cervix; time interval since the last CS more than one year; absence of serious maternal comorbidities (e.g., cardiovascular, renal and metabolic); and health facility with the right equipment and trained personnel.
Factors related to higher VBAC failure rates are BMI greater than 30, fetal macrosomia, labour induction, non-white ethnicity, no previous vaginal delivery, advanced maternal age (> 40), medical disorders, and previous CS for dystocia can reduce the success rate to 54%. The presence of these factors can lower success rates to as low as 40% [13,15].
The choice of future delivery is affected by several determinants including clinical factors in the pregnancy, maternal preference and social circumstances, willingness to have a vaginal birth, previous vaginal birth, and advantages and disadvantages of each mode of delivery. However, physician’s counselling is one of the most significant factors affecting women’s decisions regarding the route of delivery [25]. The unwillingness of the physician to support VBAC and preference for CS significantly lower uptake rates [23].
In a population?based cross?sectional study,Cegolon et al examined the patterns of previous CS, elective repeat CS, VBAC, and associated factors, the authors suggested that a careful evaluation of indication for previous CS as well as staff education, prenatal counseling, clinical audit, and financial rewards could be beneficial in term of reducing the primary cesarean delivery rates and promoting VBAC [25]. A 10% improvement in VBAC uptake rate was revealed by an Australian study after the establishment of a dedicated VBAC clinic for counselling and provision of a consistent approach to care during pregnancy and labour [28]; hence a pro-VBAC culture (including physicians’ attitude supportive of VBAC) is imperative [29] for our unit as we do not have a dedicated VBAC clinic and patients are seen by different consultants.
VBAC in special circumstances
Twins- All our patients with twins had CS for obstetric reasons or maternal preference. Some studies of women with twins who attempt VBAC have consistently shown that their outcome is like that of women with singleton gestation attempting VBAC. Women with twins and one previous CS who are otherwise appropriate for vaginal delivery can be offered TOLAC [15,32].
Induction of labour for maternal or fetal indication is an option in women with one previous CS. Some of the 80 (24.46%) women who had CS for not being in labour when due for delivery could have had an induction, however, this increases the risk of rupture two- to three-fold and CS around 1.5-fold compared with spontaneous VBAC labour [13]. The selection should be based on the woman’s informed decision, having an average size baby, previous vaginal delivery, and uncomplicated low-risk pregnancy. Mechanical dilatation with transcervical catheters is preferred for VBAC candidates because of the less increased risk of rupture [13].
External Cephalic Version (ECV) - There is limited data on ECV for a breech baby in a woman suitable for VBAC and is not contraindicated if the woman is at low risk of adverse outcome from ECV. Some studies suggest the likelihood of a successful ECV is similar in women with and without a prior CS [15,29,30], but McLaren RA Jr et al concluded that the success rate of ECV may be reduced in women with previous CS and ECV appears to increase risks of complications among such women undergoing a trial of labour [33]. All our patients with previous CS and breech pregnancy opted for CS.
The Northern New England Perinatal Quality Improvement Network VBAC guideline offered a three-tiered risk-based system with management suggestions as shown in table 4 [34]. If this is applied to the practice in our unit, we can conclude that our patients belong mainly to the low-risk group and this may partly explain our success rate.
Limitation: The limitation of our study includes its retrospective nature and the fact that it was conducted in a single centre; hence does not represent Qatar’s population. The relatively small sample size might have affected our result. Also, the neonatal outcome could have been better assessed with values of cord gases or Apgar scores
Recommendation
Postnatal counselling of women regarding their suitability for VBAC in a future pregnancy.
Early use of epidural in labour as a majority of the patients who changed their minds did so because of pain.
Early referral of women with one previous CS to VBAC clinic to allow for adequate time for antenatal education and counselling with use of information leaflets locally developed to promote VBAC uptake
A rigorous review of primary CS in the unit and appropriate feedback to reduce primary CS rate.
Consideration for induction of labour in appropriately selected suitable women.
Regular re-audit of good adherence to available guidelines to reduce individual variations and ensure the provision of high-quality care.
Future Directives: Research into the factors that impact most on women’s acceptance or refusal of VBAC would be helpful so that such factors can be addressed to increase the uptake rate of VBAC in the unit
Conclusion
Globally, CS is the most common operative procedure and has accounted for approximately one-third of all deliveries in Qatar. Our audit has shown that the practice of VBAC remains a safe and effective mechanism to reduce the CS rate in our clinical setting. Our good local result in terms of the success rate and safety of VBAC is promising and compatible with global data and can be used to guide patients’ decisions and improve VBAC uptake among women with one previous CS. Adequate patient education and appropriate selection are key to achieving a high VBAC success and uptake rate. This effort to increase access to VBAC and reduce the CS rate is essential to public health because of the increased operative and postoperative morbidity and mortality associated with multiple repeat CS.
Authors’ contributions
SS, SA, and KF were responsible for the design of the audit, interpretation of data, and the drafting of the manuscript. RJ, RM, and KS participated in the collection, analysis, and interpretation of data. AL was involved in audit supervision and drafting of the manuscript. All authors read and approved the final manuscript.
Ethical Approval and Consent to Participate
Ethical approval for this study as a quality improvement project was granted by the Institutional Review Board (IRB)/ Ethics Committee in Medical Research Center of Hamad Medical Corporation, Doha, Qatar. Permission to access the anonymized (de-identified) data was granted by the Clinical Informatics Unit and the Head of Obstetrics and Gynaecology in the Al Wakra Hospital.
Consent for publication
All data were anonymised so individual consent for publication was not applicable.
Data availability
The datasets generated and analysed during this study are not publicly available but are available upon reasonable request to the Medical Research Centre, HMC, and Clinical Informatics Unit of the Al Wakra Hospital.
Competing Interests
The authors declare that they have no competing interests.
Funding
The open-access publication of this article is funded by the Qatar National Library
Acknowledgment
We appreciate the sponsorship of the Qatar National Library and all our colleagues that participated in the care of the patients
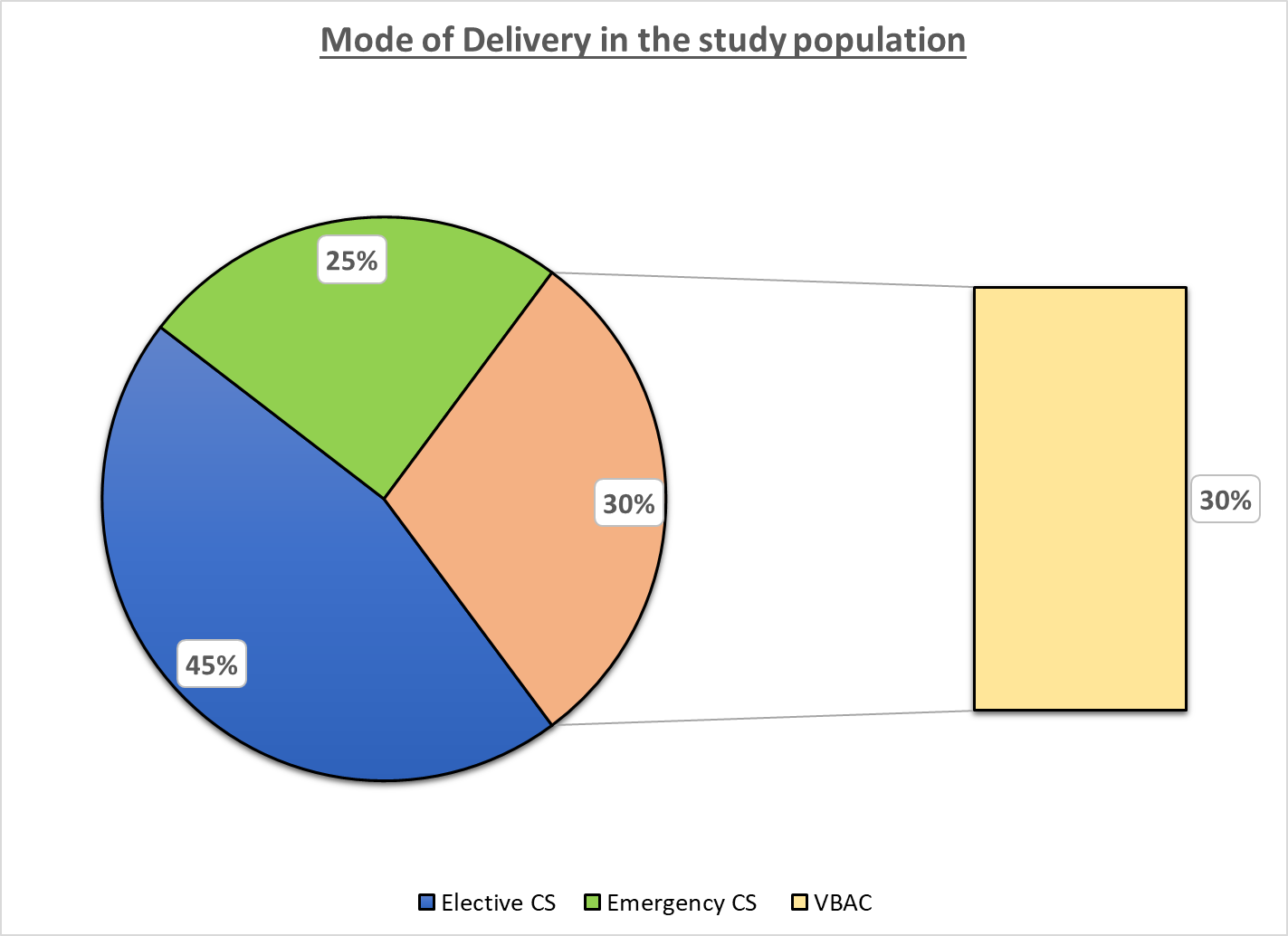
Figure 1: Modes of Delivery in the study population
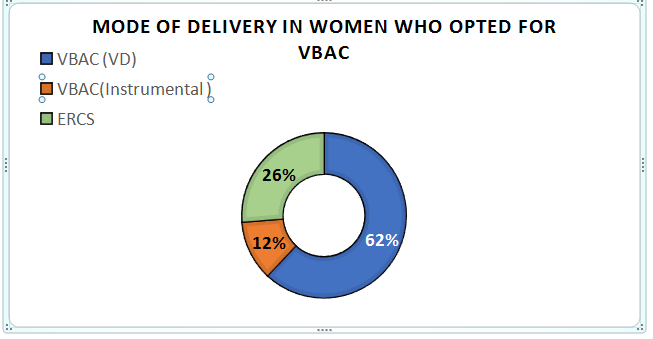
Figure 2: Depicts the mode of delivery in women who opted for Vaginal birth after Cesarean ( VBAC) . In this group 74% had VBAC and 26% had Caesaraen Section.
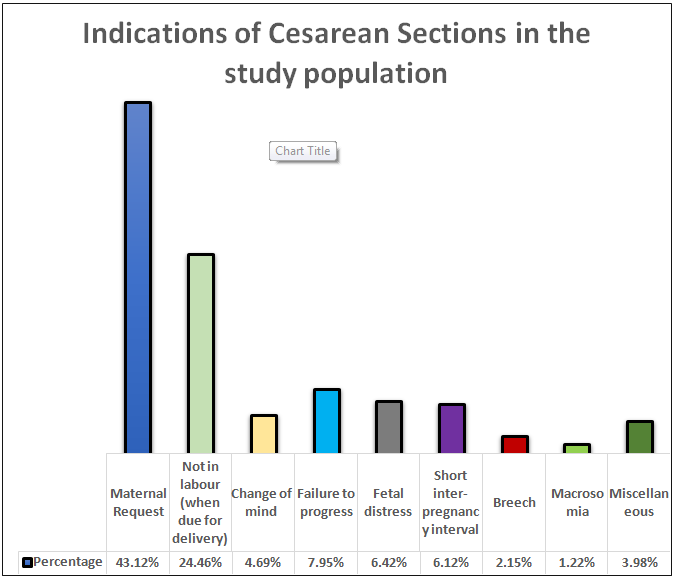
Figure 3: Indications of Cesarean Sections in the study population
|
Criteria |
Expected (Standard) |
Observed |
|
Documentation of counselling |
100% |
58% (270/465) |
|
Patient seen at 36wks |
100% |
80.0% (372/465) |
|
Use of CTG |
100% |
100% |
|
Reporting of complication |
100% |
100% |
|
VBAC success rate |
72-76% HMC/RCOG |
73.8% (138/187) |
|
VBAC Uptake rate |
8.0% (USA, 2018)19 52.2% (UK, 2014)20 |
40.2% (187/465) |
|
VBAC rate |
13.3% (USA, 2015)22 45-55% (Sweden/Finland 2016)23 |
29.7% (138/465) |
Table 1: Comparison with Auditable Standards
|
Outcome |
VBAC (n, %) |
LSCS (n, %) |
OR |
95% CI |
value of P |
|
N=138(29.68%) |
N=327(70.32%) |
|
|
|
|
|
Intrapartum stillbirths |
0 |
0 |
NA |
NA |
NA |
|
Hypoxic-ischemic encephalopathy (HIE) |
0 |
0 |
NA |
NA |
NA |
|
PPH/ Blood transfusion |
4(2.9%) |
11(3.36%) |
0.858 |
0.268 to 2.741 |
>0.05(0.796) |
|
Third/Fourth degree tear |
2 |
NA |
NA |
NA |
NA |
|
Infection (Endometritis) |
0 |
3(0.92%) |
0.335 |
0.017 to 6.524 |
>0.05(0.470) |
|
Scar Rupture |
0 |
2(0.61%) |
0.335 |
0.017 to 6.524 |
>0.05(0.470) |
|
Caesarean hysterectomy |
0 |
NA |
NA |
NA |
|
|
Relaparotomy |
0 |
2(0.61%) |
0.47 |
0.022 to 9.855 |
>0.05(0.627) |
|
Caesarean hysterectomy |
0 |
0 |
NA |
NA |
NA |
Table 2: Complications after Vaginal Birth after Cesarean (VBAC) and Caesarean Section (CS) in the study population
|
Patient classification |
Condition/complications |
Management approach |
|
Low Risk |
1 or 2 low transverse CS incision Spontaneous labour No need for augmentation Previous successful VBAC |
No additional interventions/CS delivery team may have other acute care responsibility |
|
Medium Risk |
Induction of labour Oxytocin augmentation <18 months between prior cs and current delivery Three or more previous CS |
CS team in the hospital during active phase of labour and may have other acute care responsibility. An open and staffed operating room is available if immediately required. |
|
High risk |
Recurrent clinically significant deceleration of (variable late or prolonged) not responsive to clinical intervention. Significant bleeding of uterine origin New-onset intense uterine pain. 2 hours without cervical changes in the active phase of labour despite adequate contraction |
CS delivery team present in the hospital and have no other acute patient care. Open and staffed operating room immediately available. |
Table 3: Classification of patients by level of risks
Citation: Shittu S, Athar S, Koujan F, Rawamat J, Ramanunny M, et al. (2022) Vaginal Birth after Caesarean: The Local Experience of an Obstetric Unit in the Middle East. Ann Med & Surg Case Rep: AMSCR-100203