Emerging Infectious Diseases and Diagnosis Journal
(ISSN 2652-4449)
Volume 03; Issue 01
Case Report
The First Case of Septic Shock for Klebsiella Pneumoniae Carbapenem - Resistant In Patient with Severe Interstitial Pneumonia and Long-Term Positivity for Sars-Cov-2
Weimer LE1, Cattari G2, Binelli A1, Fanales Belasio E3, Piras S2, Sensi F4
1National Center for Global Health, Istituto Superiore di Sanità, Rome, Italy
2Reparto COVID, Ospedale Marino-Alghero, ASSL Sassari, ATS Sardegna , Italy
3Department of Infectious Diseases , DMI; Istituto Superiore di Sanità, Rome, Italy
4Direzione ASSL Sassari, ATS Sardegna, Italy
*Corresponding author: Liliana Elena Weimer, National Center for Global Health, Istituto Superiore di Sanità, Rome, Italy, Email: liliana.weimer@iss.it
Citation: Weimer LE, Cattari G, Binelli A, Fanales Belasio E, Piras S (2021) The First Case of Septic Shock for Klebsiella Pneumoniae Carbapenem - Resistant In Patient with Severe Interstitial Pneumonia and Long-Term Positivity for Sars-Cov-2. Emerg Infect Dis Diag J: EIDDJ-100030. DOI: 10.53634/2652-4449.100030
Received date: 16 June, 2021; Accepted date: 02 July, 2021; Published date: 09 July, 2021
Abstract
COVID-19, caused by severe acute respiratory syndrome coronavirus 2 (SARS Cov2), has resulted in 176 million infections and 3.8 million deaths by 16 June 2021, globally. Just like other viral pneumonias, bacterial and fungal infections are common complications seen in hospitalized COVID-19 patients. A proportion of COVID-19 patients also require prolonged stay in hospitals and are at a higher risk of developing hospital-acquired bacterial and fungal infections. This is due to the impaired ability of the host to clear bacterial pathogens owing to release of specific cytokines like IL-10, IL-6, IL-17 and IL-23; reduced dendritic cells function, macrophages, natural killer cells, CD4+ and CD8+ T-cells; and also certain phagocyte-independent mechanisms by which virus infection may facilitate secondary bacterial diseases. Infections with carbapenem-resistant Enterobacteriaceae are emerging as an important challenge in healthcare settings. Currently, carbapenem-resistant Klebsiella pneumoniae are the species most commonly encountered in hospitals because is resistant to almost all available antimicrobial agents, and infections have been associated with high rates of morbidity and mortality, particularly among persons with prolonged hospitalization exposed to invasive devices . We report a case of Septic Shock for Klebsiella Pneumoniae Carbapenem-Resistant in patient with Severe Interstitial Pneumonia and Long-Term Positivity for Sars-Cov-2.
Keywords: Long-Term Sars-Cov 2, Ewing’s Sarcoma, Immunosuppressive Therapy
Description
Our Italian patient 87-year-old , male , developed fever up to 38.9 degrees C, diarrhea, asthenia, myalgia, dyspnea and poorly productive cough on 24 Mars 2021. In the Hospital of Alghero, Sardigna, Italy, he was admitted immediately after computed tomography (CT) imaging of his chest showed multiple and bilateral ground-glass opacities located in both subpleural and apico-basal spaces (especially on the right). Nasopharyngeal swab specimens were collected to detect severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) nucleic acid. The swab specimens were tested by real-time reverse transcriptase– polymerase chain reaction; a positive result was received 1 day later on 25 Mars 2021 [1-4].
Our patient was diagnosed with COVID-19 and he received O2 Therapy; methylprednisolone three i.v. boluses of 200mg; Tocilizumab was given in a single i.v. 400-mg dose ; prophylactic enoxaparin 4000 mg × 2 was prescribed , prompt protonic inhibitor (pantoprazole 40 mg), diuretic (furosemide 20 mg 1f), steroid (dexamethasone 6 mg), antihypertensive (amlodipine 5mg 1 cp losartan 50mg 1 cp), hypocolerolemizing (atorvastatin 40mg), rehydrating (suspended cardioASA for recent accidental fall with head trauma).
The patient had a history arterial hypertension, dyslipidemia, ischemic heart disease, atrial fibrillation.
On day five our patient developed episode of biliary vomiting, uncooperative, unresponsive to stimuli, febrile (Tc 38.9 C), hypotensive (PA (85/45 mmHg), tachycardic (Fc 112 bpm), tachypnotic (Fr 21 acts/min), contraction of diuresis (300 cc/24h), declivous edema, SO2 97% with VM FiO2 50%. Presumed diagnosis of septic shock.
On ecography gallbladder distended with corpuscular material inside, no free effusion in abdomen, inferior vena cava hyporeplete and collapsible. Rectal swab screening Klebsiella Pneumoniae Carbapenem-resistant negative. Culture tests (urine culture and then blood cultures) positive for Klebsiella pnemoniae carbapenem - resistant producer: antibiotic therapy with Ceftazidime/Avibactam 20.5 g tid and Fosfomycin 4g tid was started, with progressive improvement of clinical and laboratory picture.
Biochemistry test indicated leucocytes 9.58 × 10 3c/ μl (reference 4-11 × 103c/μl), D-dimer 3.3 μg/ml (reference 0.1-0.5 μg/ml), C-reactiveprotein 329 mg/l (reference 0-5 mg/l), procalcitonin 6.72ng/ml (reference 0-0.1 ng/ml), lactate dehydrogenase 316u/l (reference 135-225 u/l) and lactic acid 3.6 mmol/l (reference 0.5-1 mmol/l). The response to treatment was refractory. The swab specimens were tested by real-time reverse transcriptase–polymerase chain reaction was positive (long-term Sars-Cov-2). The patient’s haemodynamic status worsened and she suffered sepsis, respiratory and renal failure. An abdominal computed tomography (CT) showed gallbladder and abdomen distended with no signs of perforation.
Fortunately, after the maintenance of intensive medical treatment in hospital our patient progressively improved to total recovery. On May 17, 2021, our patient was negative to swab specimens (PCR) and he has after computed tomography (CT) imaging of her chest a complete resolution of bilateral areas of altered density a ground glass after treatment (Figure 1).
Due to advanced age and to avoid other intra-hospital infections the patient was followed at home. Suspended the current antibiotic therapy with resolution of symptoms and research Klebsiella Pneumoniae Carbapenem-resistant negative.
Discussion
The exact incidence of bacterial and fungal co-infections in COVID-19 is unknown, and the incidence seems to be much lower than in other viral diseases as severe influenza [5]. The rationale for antibiotic treatment in patients with COVID-19 is based on the experience with bacterial superinfection in influenza, where most studies reported initial co-infection or secondary bacterial pneumonia in hospitalized patients .
In the study of [6] the frequency of empirical treatment of patients with COVID-19 infections was quite lower (33.7 %), resulting in a lower incidence of invasive multidrug-resistant microorganisms bloodstream infections and a lower incidence of candidemia. Thus, when the probability of a bacterial infection is low antibiotics should not be prescribed and any empiric antibiotic therapy should be discontinued immediately. Antibiotics should be reserved for patients with the most severe respiratory presentations.
Our patient has been a Septic Shock for Klebsiella Pneumoniae Carbapenem - Resistant and Severe Interstitial Pneumonia and Long-Term Positivity for Sars-Cov-2. In this setting, bacterial infections has represented a serious complication that can slow down the healing process of the our patient with COVID-19 related pneumonia and can sometimes cause death. Some issues need to be investigated, such as the best empirical antibiotic therapy, the need for possible anti-fungal or anti-viral prophylaxis, and what are the best methods for the diagnosis of certain co-infections associated with COVID-19 pneumonia (e. g. pulmonary aspergillosis)
Equally, attention should be paid when assessing cases of possible invasive fungal infection, particularly cases of invasive pulmonary aspergillosis and P. jirovecii pneumonia. Several studies had reported the occurrence of COVID-19 associated with Invasive Pulmonary Aspergillosis. The largest series was shown by [7] in Jiangsu Province, China (January 22 - February 2, 2020) in which 23.3% (60/243) COVID-19 patients had co-infection with Aspergillus.
Several studies in Europe [8-10] reported different incidence rates of IPA among COVID-19 patients admitted in ICU: 19.6% in Netherland, 20.6% in Belgium and 33.3% in France. In our population, 5 cases (1.2%) of Invasive Pulmonary Aspergillosis (3 probable and 2 possible) and 3 (0.7%) cases of P. jirovecii pneumonia have been observed. All the fungal infections occurred in patients admitted in Intensive Care Unit and considering only these setting (n = 101), the incidence of Invasive Pulmonary Aspergillosis and
P. jirovecii pneumonia was very low (4.9 and 2.9%, respectively). The data showed that the incidence of pulmonary fungal infections in our population is lower than other studies. The diagnosis of aspergillosis and pneumocystosis is not easy in patients with COVID-19 pneumonia because one of the diagnostic criteria (the radiological one) is of scarce use because it can be confused with the alterations due to COVID-19. Moreover, being ubiquitous and opportunistic fungi, it is not uncommon to find them in the respiratory material of hospitalized and intubated patients. In addition, broncho-alveolar lavage is an invasive procedure highly at risk of infection for clinicians when performed in a patient with COVID-19 and is therefore rarely performed. For these reasons and in light of low sensitivity of serum galactomannan, more sensitive blood tests should be performed, e. g. PCR for Aspergillus, β-D- glucan, and the Aspergillus-specific lateral flow device and lateral flow assay,. Rectal swab screening Klebsiella Pneumoniae,Culture tests (urine culture and then blood cultures)
Conclusion
The results presented in our Case Study indicate the necessity of paying attention to carbapenem-resistant Klebsiella pneumoniae infections in patients with COVID-19. In order to prevent the increase of bacterial resistance, rational antibiotic therapy should be used, as well as continuous control and surveillance of hospital infections caused by multidrug-resistant organisms.
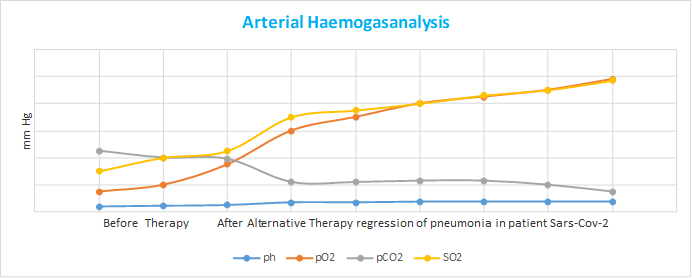
Figure 1: This figure show Arterial Haemogasanalysis before Antiviral and Antimicrobial Agents for Sars-Cov-2 and Klebsiella Pneumoniae Carbapenem-Resistant and After Therapy with regression of pneumonia.
Citation: Weimer LE, Cattari G, Binelli A, Fanales Belasio E, Piras S (2021) The First Case of Septic Shock for Klebsiella Pneumoniae Carbapenem - Resistant In Patient with Severe Interstitial Pneumonia and Long-Term Positivity for Sars-Cov-2. Emerg Infect Dis Diag J: EIDDJ-100030. DOI: 10.53634/2652-4449.100030