Annals of Medical & Surgical Case Reports
ISSN 2652-4414
Parietal Endometriosis; Cases Report and Review of Literature
Yassine D1*, Abderahim AA2, Zahara GF3, Hicham E1, Ouadii M1, Elbachir B1, Adelmalek O1 and Khalid AT1
1Department of Visceral Surgery A, Hassan II University Hospital, Fez, Morocco
2Department of Visceral Surgery B , Hassan II University Hospital, Fez, Morocco
3Department of Obstetrics-Gynecologic service A, Hassan II University Hospital, Fez, Morocco
*Corresponding author: Dkhissi Yassine, Department of Visceral Surgery A, Hassan II University Hospital, Fez, Morocco
Citation: Yassine D, Abderahim AA, Zahara GF, Hicham E, Ouadii M, et al. (2021) Parietal Endometriosis; Cases Report and Review of Literature. Ann Med & Surg Case Rep: AMSCR-100098
Received date: 07 April, 2021; Accepted date: 15 April 2021; Published date: 22 April, 2021
Abstract
Introduction: Parietal endometriosis is a rare condition that affects women of childbearing age, it represents a diagnostic challenge given the recurrent and atypical character. The different symptoms of each patient whose main symptom remains the catminaial pain and the palpation of a mass. The diagnosis is carried out primarily on the anatomopathological study of the operative part, a lot of therapeutic attitude are possible but the surgery remains the ideal.
Observation: We report t two cases collected in the surgery department A of the CHU Hassan II of Fez. A 37-year-old female and a 32-year-old female, with a history of cesarean ago, who consults for cyclic pain with sensation of mass. The radiology confirm the diagnosis of parietal mass, a medical treatment is started initially without improvement, then a surgical excision with margin of safety gave good clinical results.
Conclusion: parietal endometriosis is a rare affection; its clinical diagnosis can be difficult. Its positive diagnosis is radiological. That requires a surgical treatment once the diagnosis is confirmed.
Keywords: Anatomopathological study; Parietal endometriosis; Surgical excision
Introduction
Endometriosis is a common pathology in gynecology, causing various symptoms dominated by pain. It mainly affects women in full genital activity and its prevalence is between 18 and 20% [1].
Abdominal parietal endometriosis, defined as ectopic implantation of endometrial tissue outside the uterine cavity, affects 8-15% of women during genital activity [2]. The extra genital locations of this pathology have been widely described in the literature: pelvic peritoneum, bladder, rectum, kidney, gallbladder, lung and brain [2, 3].
Parietal endometriosis is rare because it’s a superficial graft of endometrial cells. It affects only 1-4% of extra genital endometriosis cases [3].
It usually occurs on gynecological or obstetric surgery stitchs, including; Episiotomies, uterine surgery stitchs, caesarean stitchs or a trocar orifice of coelioscopy ,Painful symptoms secondary to parietal endometriosis on a postoperative scar sometimes can lead to an erroneous diagnosis of a surgical complication, Its treatment is surgical requires a wide excision, sometimes including adjacent muscle and aponevrotic structures to prevent recurrence.
We report two observations of parietal endometriosis on caesarean scar, the clinical presentation often evocative, and the contribution of imaging, treatment and evolution of these lesions using a literature review.
Case reports
Case 1: A 37-year-old female, with a history of cesarean section 2 years ago, who consults for pain in the right iliac fossa episodic with sensation of mass in the right iliac fossa. Abdominal sonography and CT scan show a parietal mass [arrows] (Figure 1).
Case 2: A 32-year-old female, with a history of 2 cesareans section 4 years ago, who consults for pain in the left hypochondrium episodic with sensation of mass in this area. CT scan show a parietal mass (Figure 2).
Discussion
The rarity of PE is attested in the literature with paucity of reported cases. However the biggest recently reported study included 227 patients treated in a gynecological department [4]. General surgeons are seldom involved in treating PE, the biggest series treated in a surgical department being of only 15 cases. PE incidence reaches 1.08-2% after hysterotomy, 0.03-1% after cesarean section , 0.06-0.7% after episiotomy , values that are significantly lower than those reported in the past . This reduction in incidence is partially due to the preventive methods that gained popularity after Wasfie had suggested cleaning thoroughly and washing the incision area with saline after surgeries on uterus and uterine tubes. However, PE does not necessarily occur after gynecological procedures, instances of PE being observed after laparoscopic procedures, appendectomy, inguinal hernia repair, colorectal surgery [5-8] or even de novo . We encountered two patients with groin masses with no previous surgical scar.
PE may coexist with pelvic endometriosis in 26% of patients [3]. Pathogenesis of PE can be explained with several theories [9]: direct inoculation during surgical interventions and subsequent stimulation by estrogens, that could be the incriminating factor in our patients with previous gynecological interventions; retrograde menstruation theory [10]; immunesystem dysfunction and autoantibody formation (similar to autoimmune diseases); coelomic metaplasia theory; lymphatic and blood dissemination of endometrial cells, that could explain the groin PE in our patients; stem cell theory; embryonic rest theory that explains the endometriosis presence in men. Alcohol consumption and heavy menstrual flow may act as predisposing factors to disease occurrence. Instead, high parity is considered to be a protective factor against PE [10].
Clinically, PE usually respects the triad described by Esquivel: palpable mass, catamenial pain and history of cesarean section. Cyclicity of pain is not found in all cases. Other symptoms such as increasing size of lump, bleeding, discharge, skin discoloration, dysmenorrhea, infertility and dyspareunia are mentioned . In our study, catamenial pain was present in both patients the accuracy of preoperative diagnosis is reported between 20% and 50% .
Time interval elapsed from last operation and presentation could range from 6 months to 10 years . Our cases confirmed the literature results; this denotes that thorough supplementary investigations should be performed. Abdominal sonography is the most cost-efficient investigation. It may reveal hypoechoic inhomogenous echo-texture with scattered hyper echoic echoes and irregular margins, often spiculated, surrounded by a hyperechoic ring of variable width and continuity. On color Doppler examination, single pedicles may be identified at periphery of the mass. If the lesion is sizable or expending beyond abdominal wall, then the patients should undergo MRI, in order to better characterize the mass anatomy and its surrounding structures. The major role of MRI is to depict the extent of the disease preoperatively. MR characteristics of PE may be nonspecific, showing a solid enhancing mass in the abdominal wall. In cases in which MRI shows a hyper intense heterogenous lesion associated with anterior abdominal or pelvic wall surgical scarring on both T1- and T2-weighted images, subacute hemorrhage within endometrioma may be the reason. Imagistic results may be helpful in surgical planning to estimate the parietal defect and need of mesh parietal repair.
In the first case, CT-Scan and abdominal sonography shows a tissue mass subcutaneous of 4x3 cm hypoechoic inhomogenous with irregular contours, that comes into contact with the muscle rectus abdominis.
The CT-scan of the second case show a subcutaneous mass hypodense at the expense of large muscles in the left hypochondrium measuring 3-4cm with regular contours. Although fine-needle aspiration cytodiagnosis was used by other authors and gave a precise diagnosis, its application remains controversial because of risk of endometrioid tissue dissemination. The serum level of CA-125 was reported in the literature to be normal or slightly increased. Because PE is easily confound with surgical lesions like umbilical and inguinal hernias, abscess, stitch granuloma, hematoma, tumor; and moreover some patients have no antecedents of operations, histo-pathological analysis of the surgical specimen is mandatory .The histo-pathological diagnosis was performed in both patients and was based on recognition of at least 2 from 3 criteria: endometrial stroma, endometrial glands and hemosiderin pigment.
Medical treatment with combined oral contraceptives, progestogens, anti-estrogens, gonadotropin-releasing hormone agonists or aromatase inhibitors provides temporary alleviation of symptoms with their recurrence after drug cessation [4] and could be recommended to prevent recurrences after PE resection.
Surgical excision of PE is unanimously considered to be the only curative treatment. It is preferred to conduct the operation under general anesthesia. Wide surgical excision with at least 1 cm margin resection is advisable. Sometimes preoperative placement of a hook wire under ultrasound guidance is useful in tracking small, impalpable lesions. If the lesion is large and extends to deeper tissues such as muscle, aponevrosis or peritoneum and even invades other organs, visceral resections and reconstructive techniques may be required. In our cases a medical treatment was initiated initially based on analgesics and hormonal without improvement, a surgical resection with margins of safety is carried out with good clinical results with patient satisfaction
Conclusion
Even if rarely encountered by the general surgeon, PE must be thought in all female patients with/without previous surgical or obstetrical interventions that complain of catamenial pain at the level of abdominal wall or perineum. The diagnosis should be sustained by imaging studies and confirmed by histopathology. The only curative treatment remains large excision of PE with disease-free margins under general anesthesia.
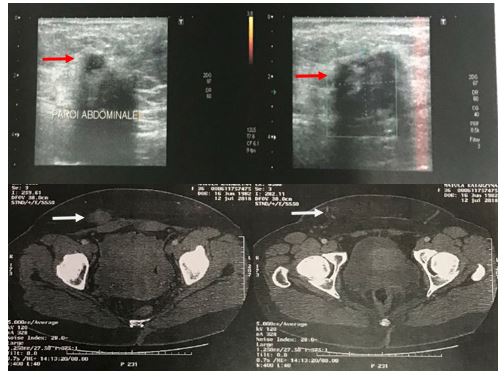
Figure 1: Surgical excision is performed; with safety margins. The anatomopathological study shows endocmetrial cells.
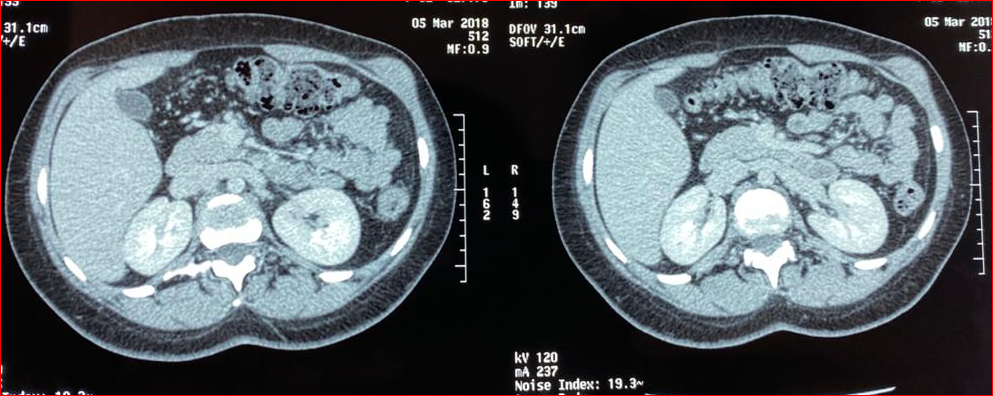
Figure 2: Surgical excision is performed; with safety margins. The anatomopathological study shows endometrial cells.
Citation: Yassine D, Abderahim AA, Zahara GF, Hicham E, Ouadii M, et al. (2021) Parietal Endometriosis; Cases Report and Review of Literature. Ann Med & Surg Case Rep: AMSCR-100098