Emergency Medicine and Trauma Care Journal
ISSN 2652-4422
Caffeine and Salt Tabs, A New Headache Cocktail-A Case of Spontaneous Intracranial Hypotension
Kunitake RC 1*, Kitamura K 1, and Lai S1
1Department of Emergency Medicine, University of California, Los Angeles, USA
*Corresponding author: Kunitake RC, Department of Emergency Medicine, University of California, Los Angeles, 924 Westwood Blvd Suite 300, Los Angeles, CA, USA
Citation: Kunitake RC, Kitamura K, Lai S (2021) Caffeine and Salt Tabs, A New Headache Cocktail-A Case of Spontaneous Intracranial Hypotension. Emerg Med Trauma. EMTCJ-100058
Received date: 14 April, 2021; Accepted date: 19 April, 2021; Published date: 23 April, 2021
Abstract
Spontaneous intracranial hypotension is an uncommon etiology of headache that frequently results from a spontaneous CSF leak of the spine and is more prevalent amongst those with underlying connective tissue disorders. We describe the case of a 44-year-old male with history of Marfan syndrome, anticoagulated with a mechanical aortic valve, who presented to the emergency department with a postural headache and was ultimately diagnosed with spontaneous intracranial hypotension in the setting of bilateral subdural hematomas and cerebellar herniation. He was deemed a high-risk candidate for CT myelography or epidural blood patch but responded well to conservative management and had complete resolution of symptoms at 2-month follow up.
Keywords: Headache; Marfan syndrome; Spontaneous intracranial hypotension
Introduction
Spontaneous intracranial hypotension is a rare but potentially life-threatening cause of headache that is often misdiagnosed on initial emergency department presentation but can lead to devastating consequences, including subdural hematomas and herniation, if untreated [1,2]. It most often arises from anatomic defects of the spinal dura and is commonly treated by epidural blood patch [3-5]. In this case, we describe a 44-year-old male with a history of Marfan syndrome who presented with spontaneous intracranial hypotension, but whose ultimate management was challenging due to multiple possible CSF leaks and anticoagulation for a mechanical aortic valve.
Case Report
A 44-year-old male with history of Marfan syndrome complicated by a prior type A aortic dissection requiring extensive surgical repair including grafting of the aortic root and ascending aorta, reimplantation of coronary arteries, and placement of a mechanical aortic valve (currently on Warfarin) presented to the emergency department with headache. Over the previous 4 days, the patient reported a gradual onset “throbbing” occipital and frontal headache that first occurred while standing at rest. His pain lasted several hours at a time, resolved while supine, and was only accompanied by mild lightheadedness while upright. There was no preceding trauma. He otherwise had no associated fevers, nausea, vomiting, visual changes, extremity numbness/weakness, or any additional neurologic symptoms.
All initial vitals were within normal limits. He was well-appearing on exam and exhibited no neurologic deficits. Labs were significant for a sodium of 134, platelets 282 x109/L, and INR 2.9. A CT brain (Figures 1 & 2) was obtained and demonstrated bilateral 2 to 4 mm chronic frontal subdural hematomas, 8 mm of inferior cerebellar tonsillar herniation, and effacement of the perimesencephalic cisterns concerning for intracranial hypotension. Emergent MRI brain confirmed the above CT findings but also noted a subacute component of the bilateral subdural hematomas. Given there was no history of trauma, lumbar puncture, or other clear etiology of his intracranial hypotension, the patient underwent MRI of his cervical, thoracic, and lumbar spine (Figure 3). This demonstrated numerous perineural root sleeve cysts of the thoracic and lumbar spine as well as a large sacral 4.4 cm × 6.7 cm × 5.4 cm Tarlov cyst, all of which were thought to be possible culprit dural defects. He was initially considered for an epidural blood patch but after careful evaluation by neurosurgery, neurology, and cardiology, was ultimately started on conservative therapy with caffeine and salt tablets due to his reassuring exam and the high-risk nature of reversing his anticoagulation with a mechanical valve. At 2 months, the patient’s headache fully resolved and a repeat CT scan showed complete resolution of all prior radiographic evidence of intracranial hypotension.
Discussion
Spontaneous intracranial hypotension is most often caused by defects of the spinal dura or spinal nerve root sheaths that lead to CSF leaks, ultimately precipitating CSF hypovolemia and tension on intracranial bridging veins and meninges [6]. Parallel to the more commonly seen iatrogenic post-lumbar puncture CSF leak, this clinically results in orthostatic headaches but can occasionally lead to subdural hematomas [2]. Spontaneous intracranial hypotension occurs at an annual incidence of 5 in every 100,000 individuals but is seen in greater frequency in those with connective tissue disorders such as Marfan syndrome or isolated features of connective tissue disorders (e.g., joint hypermobility, arachnodactyly, etc.) [7-9]. MRI brain and spine are considered the first line imaging modalities to identify radiographic sequelae of spontaneous intracranial hypotension (sensitivity 73-94%), and recent studies have shown the potential benefits of non-invasive MRI myelography [5,10]. CT myelography is still considered the gold standard in localizing the exact CSF leak itself [3]. In this particular case, MRI revealed multiple possible target lesions and reversing his anticoagulation to facilitate intrathecal contrast and/or multiple epidural blood patches was particularly high risk. Fortunately, the patient responded well to conservative management and the chronicity of his CSF leak(s) likely minimized the impact of his subdural hematomas and cerebellar herniation. We believe this case illustrates the importance of considering the uncommon spontaneous intracranial hypotension when treating patients with headaches in the emergency department.
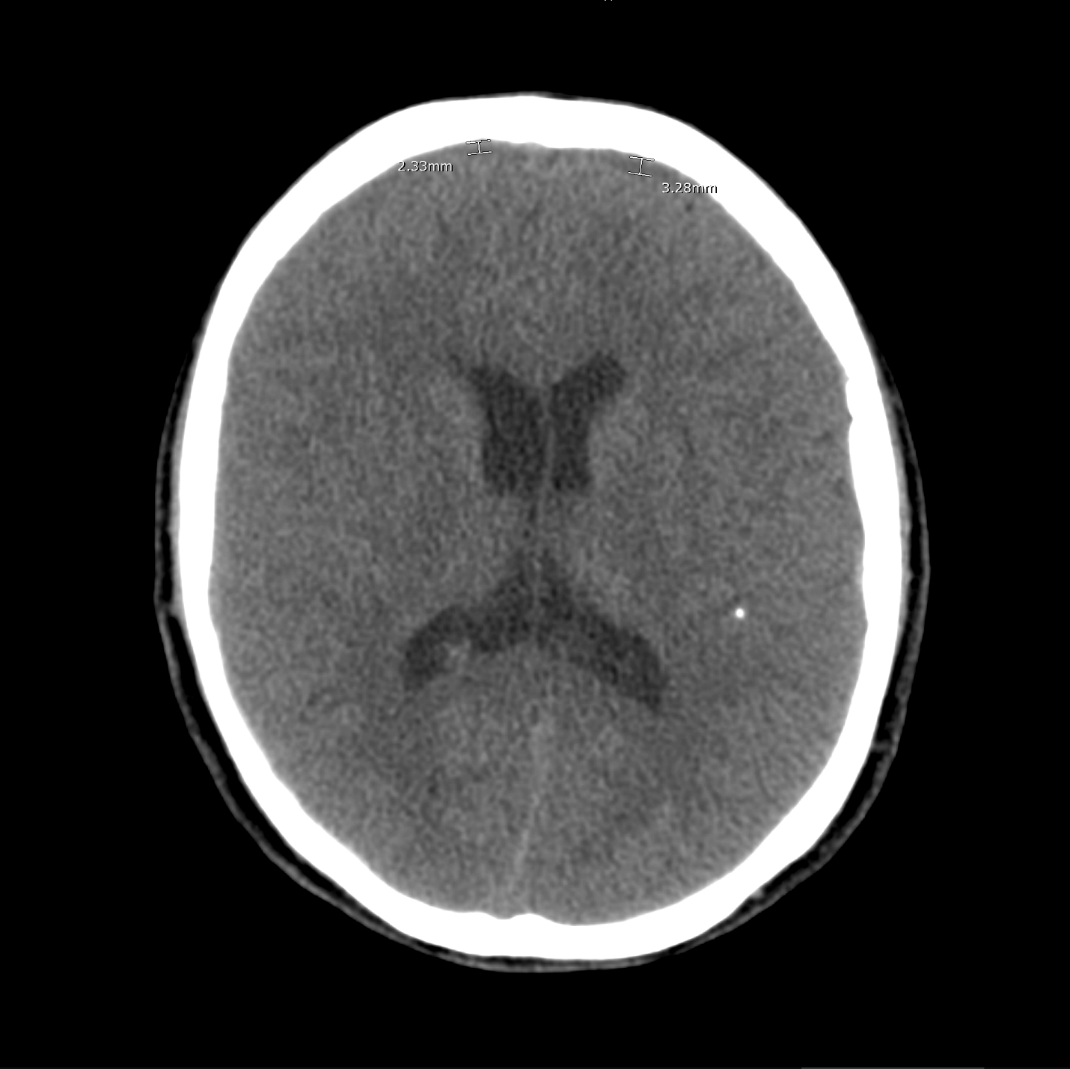
Figure 1: CT Brain without contrast showing bilateral chronic frontal subdural hematomas.

Figure 2: CT Brain without contrast showing 8 mm of inferior cerebellar tonsillar herniation.

Figure 3: MRI lumbar spine showing a large sacral Tarlov cyst.
Citation: Kunitake RC, Kitamura K, Lai S (2021) Caffeine and Salt Tabs, A New Headache Cocktail-A Case of Spontaneous Intracranial Hypotension. Emerg Med Trauma. EMTCJ-100058