Emerging Infectious Diseases and Diagnosis Journal (ISSN 2652-4449)
Volume 03; Issue 01
Case Report
Respiratory Failure and Long Sars-Cov-2 in a Patient with Progressive Multiple Sclerosis on Immunosuppressive Therapy
Weimer LE1*, Cattari G2, Binelli A1, Fanales Belasio E3, Piras S2, Sensi F4
1National Center for Global Health, Istituto Superiore di Sanità, Rome, Italy
2Reparto COVID, Ospedale Marino-Alghero, ASSL Sassari, ATS Sardegna, Italy
3Department of Infectious Diseases, DMI; Istituto Superiore di Sanità, Rome, Italy
4Direzione ASSL Sassari, ATS Sardegna, Italy
*Corresponding author: Liliana Elena Weimer, National Center for Global Health, Istituto Superiore di Sanità, Rome, Italy, Email: liliana.weimer@iss.it
Citation: Weimer LE, Cattari G, Binelli A, Fanales Belasio E, Piras , et al. (2021) Respiratory Failure and Long Sars-Cov-2 in a Patient with Progressive Multiple Sclerosis on Immunosuppressive Therapy. Emerg Infect Dis Diag J: EIDDJ-100028. DOI: 10.53634/2652-4449.100028
Received date: 14 June, 2021; Accepted date: 01 July, 2021; Published date: 08 July, 2021
Abstract
The world, and especially our healthcare system, is currently confronted with one of the greatest challenges of modern times. At June 2021, the SARS-CoV-2 pandemic has already infected more than 174 million people worldwide and resulted in 3,7 million deaths. A major concern during the current severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic is the use of immunosuppressive therapies for the treatment of Multiple Sclerosis due to an increased risk of contracting SARS-CoV-2 and more severe disease. Multiple Sclerosis is known as an autoimmune disease, in which the immune system — which normally protects against viruses and other insults — wrongly attacks the fatty sheath around nerve fibers to disrupt the flow of electric signals, causing a variety of symptoms. Most Multiple Sclerosis disease-modifying therapies are designed to suppress these attacks by limiting immune responses. But that can leave people more vulnerable to infections, including SARS-CoV-2. Actually the large number of different disease-modifying therapies in the treatment of neuroimmunological diseases such as multiple sclerosis poses a challenge. We report a case of Respiratory Failure and Sars-Cov-2 in a Patient with Progressive multiple sclerosis on immunosuppressive therapy.
Keywords: Progressive Multiple Sclerosis; Long Sars-Cov-2; Respiratory Failure
Introduction
The world, and especially our healthcare system, is currently confronted with one of the greatest challenges of modern times. At June 2021, the SARS-CoV-2 pandemic has already infected more than 174 million people worldwide and resulted in 3,7 million deaths. A major concern during the current severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic is the use of immunosuppressive therapies for the treatment of Multiple Sclerosis due to an increased risk of contracting SARS-CoV-2 and more severe disease [1].
Multiple Sclerosis is known as an autoimmune disease, in which the immune system which normally protects against viruses and other insults wrongly attacks the fatty sheath around nerve fibers to disrupt the flow of electric signals, causing a variety of symptoms. Most Multiple Sclerosis disease-modifying therapies are designed to suppress these attacks by limiting immune responses. But that can leave people more vulnerable to infections, including SARS-CoV2 [2]. Actually the large number of different disease- modifying therapies in the treatment of neuroimmunological diseases such as multiple sclerosis poses a challenge [3]. We report a case of Respiratory Failure and Sars-Cov-2 in a Patient with Progressive multiple sclerosis on immunosuppressive therapy.
Description
Our Italian patient 70-year-old, woman, developed dyspnea, chest tightness with fever, cough and a progressive neurological
symptoms hypoesthesia lower limbs, apraxia) on 7 April 2021. In the Hospital of Alghero, Sardigna, she was admitted immediately after computed tomography scan (CT) imaging of her chest showed multiple ground-glass opacities located in both subpleural spaces. Nasopharyngeal swab specimens were collected to detect severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) nucleic acid. The swab specimens were tested by real-time reverse transcriptase–polymerase chain reaction; a positive result was received 7 hours later. Our patient was diagnosed with Sars-Cov-2 and was given 100-mg Remdesivir (VeKlury) tablets orally, 3 times daily, Tocilizumab was given i.v 400 mg single dose for “cytokines storn”, received 400 mg of moxifloxacin IV daily for 3 days , Pantoprazole 40 mg x 2, Methylprednisolone 20 mg,
Fondaparinux 2.5 mg, Pregabalin 75 mg x 3, Azathioprine 50 mg x 2, Clonazepam10 drops, Amitriptyline 6 drops x 3, Diazepam 10 drops x 3, Quetiapine 25 mg x 2, Folin 5 mg, Cholecalciferol 100,000 IU, rehydration therapy.
The patient had a history of insulin-dependent diabetes mellitus and symptomatic Progressive Multiple Sclerosis, which was diagnosed on 2 February 2016 with immunosuppressive therapy and symptoms in rapid evolution (muscular pain, headache, pain in the legs and feet, back pain, and muscle spasms, trouble walking, vision problems, muscle weakness, hypoesthesia lower limbs). At second Computed Tomography scan, bilateral pneumonia with interstitial character and viral pathogenesis and respiratory failure.
After therapy for Sars-COV-2, Diabetes and Progressive Multiple Sclerosis, response to treatment was refractory.
On 2 May 2021 swab specimens were tested by real-time reverse transcriptase–polymerase chain reaction; a positive result was received 6 hours later (Long Covid-19). On 26 May 2021 after immunosuppressive and antiviral therapy, our patient has shown a progressive clinical stabilization. Her blood examination displayed a total white cell count (WCC) of 11.6, a neutrophil count of 9.8 and a lymphocyte count of 0.6. His neutrophil-lymphocyte ratio (NLR) was 16.4 compared to expected value of < 2 for his age group. C- Reactive protein was also significantly elevated (132 mg/L compared to expected < 5 mg/L) at admission.
On May 27, 2021, computed tomography scan (CT) imaging of her chest has revealed a complete resolution of bilateral areas of altered density a ground glass after treatment and improving arterial haemogasanalysis (Figure 1).
Fortunately, on May 28, 2021, nasopharyngeal swab specimens was negative and after the maintenance of intensive medical treatment in hospital computed tomography (CT) imaging of her chest a complete resolution.
Discussion
COVID-19 infection affected patients globally, with a high incidence in Europe and the Americas. The disease has affected patients of all age groups; however, heterogeneity in the outcome of COVID-19 infection associated with comorbidities, racial differences, and individual characteristics such as smoking has been observed [4]. Of note, the presence of comorbidities has been extensively studied to identify patients at higher risk of infection and those with worse outcomes.
Here, we report a patient responding to Remdesivir for regression of pneumonia caused by Sars-Cov-2 with Tocilizumab, despite immunosuppressive therapies for Multiple Sclerosis. Currently, there are 11 drugs for this disease (i.e., intramuscular interferon (IFN) beta-1a; subcutaneous IFN beta-1a; subcutaneous IFN beta-1b; subcutaneous glatiramer acetate; oral dimethyl fumarate; oral teriflunomide; oral fingolimod; oral cladribine; intravenous natalizumab; intravenous alemtuzumab; and intravenous ocrelizumab) have been approved for the treatment of relapsing-remitting Multiple Sclerosis in the European Union. The monoclonal antibody ocrelizumab is the only approved therapy for primary progressive multiple sclerosis. Siponimod has been introduced to the market for the treatment of secondarily progressive Multiple Sclerosis in the EU. Recently, a Swedish national cohort study showed that patients with Multiple Sclerosis have a generally higher risk of infection [5]. The results of this large observational study suggested that rituximab was the only drug with a significantly increased infection rate compared with interferon beta and glatiramer acetate in the most adjusted model. This included particularly severe bacterial infections.
Overall, immunosuppressive therapy does not appear to have a major impact on SARS and MERS-CoV and Sars-Cov-2 infection nor does it appear to lead to a severe course of disease in many cases [6]. As a final consideration, it should be noted that coronaviruses appear to implicate the host inflammatory response as an important contributor to the disease process. Dysregulated (innate) immune responses appear to be crucial factors in tissue damage after initial infection. Therefore, immunomodulatory therapy could not only be seen as a risk factor, but could help to mitigate the damage caused by the excessive immune response induced by the virus.
Conclusion
We can hope to provide adequate clinical care and urgently design interventional studies to prevent Sars-Cov-2 infection in the patient with Multiple Sclerosis because the mortality associated with this devastating pandemic is dramatically high. Overall, immunosuppressive therapy does neither seem to have a major impact on infection with SARS- and MERS-CoV, Sars-Cov-2 nor does it seem to lead to a severe disease course in many cases. In summary, previous coronavirus outbreaks have not shown an increased risk for immunocompromised patients. Patients with severe neuroimmunological diseases should be kept from hasty discontinuation of immunotherapy.
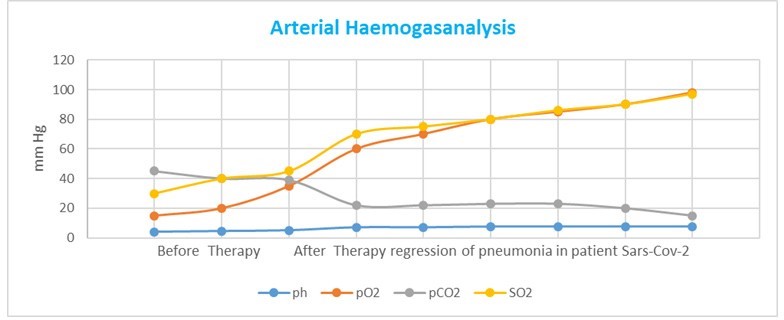
Figure 1: Before Remdesivir and TocilizumabTherapy and After Remdesivir and Tocilizumab Therapy regression of pneumonia in patient with Sars-Cov-2 and Multiple Sclerosis without interruption of Immunosuppressive Therapies.
Citation: Weimer LE, Cattari G, Binelli A, Fanales Belasio E, Piras , et al. (2021) Respiratory Failure and Long Sars-Cov-2 in a Patient with Progressive Multiple Sclerosis on Immunosuppressive Therapy. Emerg Infect Dis Diag J: EIDDJ-100028. DOI: 10.53634/2652- 4449.100028