Journal of Surgery and Insights
Volume 04; Issue 01
Case Report
Challenges of Management of Long Tubular Complicated Enteric Duplication: A Case Report of a Pediatric Patient
Hamed RR¹´²*and Sa’ada J²
¹Department of General Surgery, Al Makassed Hospital, Jerusalem, Palestine
²Department of Paediatric Surgery, Al Makassed Hospital, Jerusalem, Palestine
*Corresponding author: Hamed RR, Department of General Surgery, Makassed Hospital, Jerusalem, Palestine
Citation: Hamed RR and Sa’ada J (2021) Challenges of Management of Long Tubular Complicated Enteric Duplication: A Case Report of a Pediatric Patient. J Surg Insights: JSI-100033
Received date: 01 June, 2021; Accepted date: 01 July, 2021; Published date: 08 July, 2021
Abstract
Enteric duplication is one of the causes of gastro-intestinal (GI) tract bleeding and should be always suspected especially among paediatric population.Management of complicated cases has been controversial due to their unpredictable clinical behaviour. In this study, we presented a 2 year old female patient with a history of lower GI bleeding and haemoglobin drop. Investigations failed to show the cause of bleeding. Due to lack of Technetium, we decided to proceed for exploratory laparotomy. Intra-operatively, a large segment of duplicated small bowel containing ulcers was found. The decision to do minimal bowel resection, preserving the adjacent healthy bowel, was an attractive option. But later on, it showed to be unsuitable as the patient developed new ulcers and recurrent attacks of melena. This case was reported because of lack of studies and guidelines on management of intestinal duplication when the duplicated segment is large.
Keywords:Enteric duplication; Lower GI bleeding; Technetium
List of abbreviations:
GI : Gastro-intestinal
ED : Enteric duplication
Hb : Haemoglobin
PRBCs : Packed red blood cells
U/S : Ultrasonography
CT : Computed tomography
MRI : Magnetic resonance imaging
Introduction
Enteric duplication (ED) is a rare congenital malformation that can occur anywhere along the gastrointestinal (GI) tract [1,2]. The variations in the size, location, type [3], and therefore the clinical presentation of this malformation, have rendered the accurate pre-operative diagnosis of the ED difficult. These variations have also made it difficult to make a standard outline for management of this anomaly.
The most common site for enteric duplication is the small bowel, constituting about slightly less than half of the total percentage of the anomaly [1,4,5]. The clinical diagnosis of ED is difficult due to the variations stated above, in addition of the mimicry between the symptoms of different types of ED and other pathological diseases among paediatrics. Few studies focused on the appropriate management of ED, especially long ones. Therefore, the aim of the present study was to outline the treatment options, with their benefits and risks, for complicated ED.
Case presentation
A 2 years old female child, a full term product of normal vaginal delivery, with a birth weight of 2800 grams, and with an insignificant peri-natal history, presented to our hospital with a history that dated back to 3 weeks prior to admission when she started to have recurrent attacks of large amount of painless haematochezia & melena. She had history of haemoglobin (Hb) drop down to 6 g/dl and therefore, she received packed red blood cells (PRBCs). She had no other symptoms. The clinical examination was unremarkable.During routine investigations, her Hbwas found to be 8.2, and she had normocytic normochromic anaemia. Upper and lower endoscopies were done and were normal. Therefore, the initial diagnosis was most likely Meckel’s diverticulum. However, Technetium-99m was not available in our hospital. Therefore, we decided to proceed to exploratory laparotomy.Intra-operative findings, after running of bowels, revealed normal bowel loops from the ileocecal valve up to 60 cm proximally, then a segment of unhealthy bleeding bowel (Figures 1-2)measuring about 6 cm containing ulcers in its inner lining. Starting from the bleeding segment proximally, there is a 60 cm segment of small bowel duplication (Figure 3 (A-B)). The proximal part of the duplicated loop had a blind end.
Resection of the small 6-cm unhealthy bleeding bowel segment was done. Then the dilemma was to resect the whole length of duplicated bowel alongside the adjacent native bowel or just to do two common channels between the duplicated and the adjacent healthy bowel. The former option would let the patient suffers from possible complications of sacrificing a large segment of healthy bowel, while the second one would risk making the patient suffer further ulceration and bleeding from the remaining duplicated bowel loop. However, as the duplicated loop in our case was in the mesenteric side, and the blood supply was, in many areas, common and difficult to be separated between the native bowel and the duplicated one, we decided to preserve the duplicated part and to do two anastomoses. Incidental appendectomy was also done.
Post-operative, the patient did very well and her Hb was stable. She was discharged home in a good general condition after a week of in-patient observation. She also did well at home for about 2 moths, but then started to develop attacks of melena again. Faecal occult blood test was done and was positive. Therefore, she was admitted again to our hospital and underwent laparotomy with resection of the duplicated bowel, alongside the adjacent healthy bowels (Figure 4), with release of ileo-ileal intussusception, and anastomosis between normal bowels. Post-operatively, the patient was kept under observation for a week, and started on oral diet gradually without any complications. Since the second operation, the patient has been well, and did not develop any attacks of melena or Hb drop.
Discussion
Enteric duplication (ED) is a rare congenital anomaly that can occur anywhere along the gastrointestinal (GI) tract [1,2].This anomaly can occur as a single or multiple pathologies. The most common location of ED is the distal ileum occupying about 33% of the total percentage of the anomaly, followed by the oesophagus (20%), colon (13%), jejunum (10%), stomach (7%) and duodenum (5%) [1].
ED can be asymptomatic, but it can sometime produce symptoms, which occur mainly among the paediatric population [1,2]. The most common clinical presentation of the small bowel ED is intestinal obstruction or perforation [4]. However, lower GI bleeding is a possible complication from ED, as the duplication of bowel often contains ectopic gastric mucosa, which is liable to local peptic ulceration and subsequent lower GI bleeding [2]. Bleeding may also occur due to stasis and bacterial overgrowth causing subsequent local ulceration or ischemic necrosis of the bowel [6].
Bleeding from ED can be a misleading clinical symptom as many other common GI conditions among paediatrics can mimic this presentation, including intestinal polyp and Meckel’s diverticulum. So a high index of suspicion is required [3], especially when symptoms occur in the first two years of life.The ED can be classified as simply as cystic and tubular duplications, with the former ones being the commoner (65%) and are completely separate from the intestine, while the later ones tend to have communication with the gut lumen commonly at the caudal end, but can also have communication at both ends [2].
However, a more convenient classification was described taking into consideration the blood supply of the duplication and involved bowel [7]. This classification classifies the duplications into [2]:
This classification has some important clinical implications in the intra-operative settings. One of these implications is that studying the vascular pattern of the ED allows resection of the duplication without the need of resecting the involved bowel [7] and thus reducing the immediate and remote intra- and post-operative complications.
The diagnosis of ED, as mentioned above, can be challenging. The radiological investigations, as well as the use of endoscopies, may not be helpful in diagnosing the duplication, but can provide an indirect clue of the diagnosis by excluding other causes.
Abdominal x-ray, ultrasonography (U/S), computed tomography (CT) and magnetic resonance imaging (MRI) are all common imaging modalities, however, their use is limited in case of bleeding duplication because of their inability to detect the ectopic gastric mucosa [3]. About 24% of the duplications contain ectopic mucosa [5]. In this type of anomalies, Technetium-99m pertechnetate scintigraphy can accurately identify the ectopic gastric mucosa [3]. However, the use of Technetium is not always available. Therefore, the intra-operative diagnosis during laparotomy is not uncommon and that arises many challenges for the surgeon to choose the best operative technique to manage the malformation, due to lack of enough studies and recommendations.
In our case, the lack of Technetium in the nearby region and due to technical causes that prevented the imaging study to be done, and due to the recurrence of the attacks of rectal bleeding which were associated with anaemia, the decision was to procced with exploratory laparotomy.
The most challenging part during surgery of bowel duplication, especially when the duplicated part is long, is the decision of whether to conserve the duplicated part, and therefore to take a risk of further attacks of bleeding, orto do resection, for both the duplicated and the adjacent native bowel, with subsequent possible complications of short bowel syndrome.Usually the cystic and small tubular duplications are managed with complete resection [4]. In cases where the attached bowel is too long, stripping of the entire mucosa leaving behind sero-muscular layer intact may be done[7].
The clinical behaviour of asymptomatic ED cannot be predicted as it may increase gradually in size and produce fatal complications like massive bleeding, intestinal obstruction and a potential risk for malignant transformation in the adulthood [1]. Therefore, the management of these cases remains controversial.
On the other hand, management of long tubular ED is difficult. Creation of common openings at both ends of the duplicated bowel with the native one is an option to preserve the function of native bowel, especially when excision of the adjacent native bowel is inevitable due to vascular considerations. However, this option carries a risk of making the patient suffers from complications stated above due to possible presence of some ectopic nests.
When acute symptoms occur, surgical excision becomes the first line of management of ED. Minimally invasive techniques, like laparoscopy, are attractive options to treat small duplications [1,4], however, laparotomy should be done when indicated. In general, the principles of management include bowel preservation, mucosectomy, internal drainage and staged operations where indicated in order to achieve the best possible outcome for each individual child [4]. However, when symptoms recur or do not improve with bowel preservation surgeries, complete resection of the duplicated bowel becomes an inevitable option.
Conclusion
This case focuses on the importance of considering enteric duplication in the differential diagnosis of any case of bleeding per rectum, especially in children below 2 years of old.It also suggests that management of cases of ED double anastomoses of the duplicated bowel with the healthy native bowel, even when the duplicated portion of the bowel is being large and looks healthy, could be an unsafe option as it is liable to recurrent ulceration and bleeding. However further studies are still needed in this aspect.

Figure 1: The bleeding part of bowel with ulcers in its inner lining.
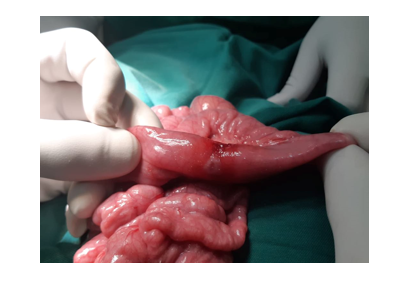
Figure 2: The appearance of the unhealthy bowel segment from outside.
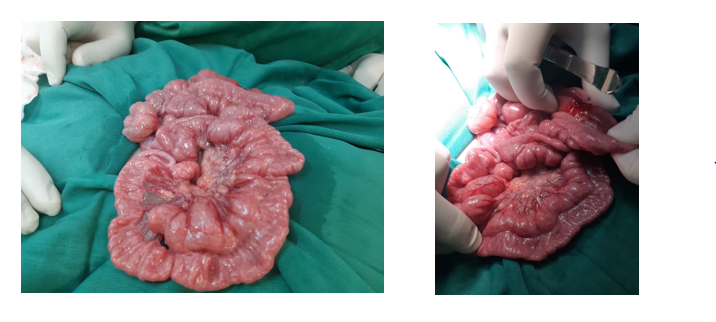
Figure 3 (A-B): The appearance of enteric duplication, alongside the healthy adjacent bowel.

Figure 4: The duplicated part of small bowel after resection.
Citation: Hamed RR and Sa’ada J (2021) Challenges of Management of Long Tubular Complicated Enteric Duplication: A Case Report of a Pediatric Patient. J Surg Insights: JSI-100033