Annals of Medical & Surgical Case Reports
(ISSN: 2652-4414)
Image Article
Portal Venous Gas
Jin-Ping Zhang 3, Wei Liu*1,2
1Institute of Digestive Disease, China Three Gorges University, Yichang, China 2Department of Gastroenterology, Yichang Central People’s Hospital, Yichang, China 3Department of Gastroenterology, Zigui People’s Hospital, Yichang, China
*Corresponding Author: Wei Liu, Institute of Digestive Disease, China Three Gorges University, 8 Daxue Road, Yichang 443000, China
Citation: Zhang JP, Liu W (2020) Portal Venous Gas. Ann Med & Surg Case Rep: AMSCR-100091
Received date: 12 December 2020; Accepted date: 23 December 2020; Published date: 29 December 2020
A 60-year-old man presented to the emergency department with an 14-hour history of severe abdominal pain, vomiting and inability to pass flatus after excessive drinking. Exceptfor alcohol abuse, he had no documented medical history. The pulse was 126 beats per minute, and the blood pressure 97/56 mm Hg. Physical examination revealed his abdomen was diffusely tender, with hypoactive bowel sounds. Laboratory tests of the blood confirmed a white-cell count of 29,500 per cubic millimeter (reference range, 4000 to 10,000), a lactate level of 12.4 mmol per liter (reference range, 0.5 to 1.7 mmol per liter), and an arterial blood pH of 7.22 (reference range, 7.35 to 7.45). Computed tomography of the abdomenconfirmed extensive portal venous gasof the left liver lobe, as well as gas in superior mesenteric vein and the bowel wall, whose appearance wasconsistent with ischemic bowel. Portal venous gas is a poor prognostic sign in patients, which is most commonly associated with bowel ischemia. Treatment was initiated with fluid resuscitation, vasopressors and broad-spectrum intravenous antibiotics. After a well-informed discussion of options for interventions with the patient’s family, the decision was made not to pursue an urgent laparotomy. The patient died 6 hours after presentation with clinical condition deteriorated rapidly.
Acknowledgements
Funding: This work was supported by National Natural Science Foundation of China (31600134).
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this “Images in Clinical Medicine”.
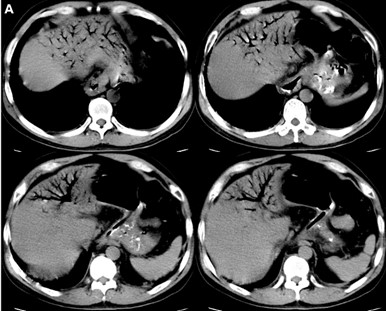
Figure 1: Portal Venous Gas. (A) Axial CT image of abdomen
Citation: Zhang JP, Liu W (2020) Portal Venous Gas. Ann Med & Surg Case Rep: AMSCR-100091