Australian Journal of Nursing Research
(ISSN 2652-9386)
Research Article
Training Law Enforcement to Identify and Treat Diabetes Emergencies
Smith BG*, Smith RE
Department of Nursing, Delta State University, USA
*Corresponding author: Brandy Smith, Department of Nursing, Delta State University, USA
Citation: Smith BG and Smith RE (2020) Training Law Enforcement to Identify and Treat Diabetes Emergencies. Aus J Nursing Res AJNR-100020
Received date: 20 October, 2020; Accepted date: 26 October, 2020; Published date: 02 November, 2020
Abstract
Purpose: To educate Law Enforcement on signs, symptoms, and treatment of diabetes emergencies in drivers to prevent further delay of care.
Background: In the United States, there is an estimated one in six people with diabetes of driving age. Furthermore, there is one state law officer to every 667 people with diabetes. Law enforcement’s knowledge level in identifying diabetic emergencies can result in fatal outcomes. Hypoglycemia, or low blood sugar, can occur suddenly and without warning. Too often, warning signs of low blood sugar are mistaken for intoxication, which may lead to prolonged and unnecessary field sobriety testing, resulting in detrimental patient outcomes. With impaired hypoglycemia awareness (IHA), diabetic shock may ensue. Therefore, it is imperative for law enforcement to be trained on identifying diabetic emergency symptoms and initializing treatment to protect, serve and save people living in communities. Drivers have reported hypoglycemic events while driving. Research studies have shown advanced knowledge results in better prognosis for people with diabetes. The World Health Organization and American Diabetes Association support officer education to detect and treat diabetes emergencies.
Methods: A quantitative, quasi-experimental study was initiated with on-site educational sessions held in two rural counties in Mississippi. The research tool comprised of 14 questions was issued to assess knowledge of diabetes, symptoms, and treatment prior to training. An educational session followed the pretest. Handouts of the power point were given, along with the American Diabetes Association (ADA) Officer Assist program and Diabetes is Serious handouts. A laminated tool was provided to the individual participants to use in the field. Identical to the pretest, a posttest was issued after the educational session. A paired t test was used to analyze the data.
Outcomes: Statistical significance (p= <0.05) was identified in eight out of fourteen questions, thereby determining improved ability to identify and treat drivers with diabetes emergency symptoms by law enforcement. Eighty-nine percent of participants scored above the recommended 75% passing score on the posttest. Improved identification results in better health outcomes.
Implications for nursing: By timely notification of emergency medical services (EMS), there should be better prognosis and improvement in health outcomes of those with diabetes emergencies. This will also facilitate a collaborative relationship using a community approach between law enforcement and medical personnel.
Keywords: Competence training Diabetes knowledge test; Diabetes; Diabetes awareness; Diabetes training; Diabetic emergencies; Driving, diabetes complications; Emergency services Hypoglycemia; First responder training; Hypoglycemia roadside screening tool; Law enforcement training; Recognition of diabetes symptoms
Training Law Enforcement to Identify and Treat Diabetes Emergencies
Law enforcement’s lack of knowledge in identifying diabetic emergencies can result in fatal outcomes. In 1981, Governor William Winter (MS) endorsed standards for law enforcement supporting employment, training, and education. He recognized the impact of law enforcement officers in areas related to “health, safety and welfare” (Board on Law Enforcement Officer Standards and Training [BLEOST], 2017, para. 4). Further, standards and training have realized “the modern law enforcement officer has a far-reaching complex role in society” (BLEOST, 2017, para. 4). Hypoglycemia, or low blood sugar, can occur suddenly and without warning. Too often, warning signs of low blood sugar are mistaken for intoxication, which may lead to prolonged and unnecessary field sobriety testing, resulting in detrimental patient outcomes. With impaired hypoglycemia awareness (IHA), diabetic shock may ensue. Therefore, it is imperative for law enforcement to be trained on identifying diabetic emergency symptoms and initializing treatment to protect, serve and save people living in communities.
Many communities are laden with diabetes. According America’s Health Rankings (2017) Mississippi is ranked number one in diabetes population, with 14.7%, and last in diabetes outcomes in the United States (U.S.) (United Health Foundation [UHF], 2017). Mississippi’s diabetes prevalence is well above the national average of 9.9% (UHF, 2017).
Mississippi places no restrictions on drivers with diabetes, nor requires reporting of diabetes diagnosis at time of drivers’ licensure initial application or renewal process. However, Mississippi offers and encourages voluntary reporting in order to obtain a “special” driver’s license identifying the driver with diabetes. Certification of Diabetes, form DE 16A, must be completed by a physician in order to obtain special license.
Diabetes Mellitus (DM) is a chronic health condition affecting millions worldwide by affecting the blood glucose levels of the people who suffer with this disease. The Centers for Disease Control and Prevention (CDC) defines diabetes as, “the condition in which the body does not properly process food for use as energy your body either doesn't make enough insulin or can't use its own insulin as well as it should. This causes sugars to build up in your blood” (Diabetes, n.d., p. 1). The American Diabetes Association (ADA) defines hypoglycemia as “a condition characterized by abnormally low blood glucose (blood sugar) levels, usually less than 70 mg/dl” (Hypoglycemia (Low Blood Glucose), 2015, para. 1). ADA suggests “people you are in frequent contact with (for example, family members, significant others, and coworkers) should also be instructed on how to administer glucagon to treat severe hypoglycemic events” (Hypoglycemia (Low Blood Glucose), 2015, para. 10) [1-10].
Serious and life-threatening complications can occur from inability to control blood glucose levels. Severity of the complications are usually a consequence of uncontrolled blood glucose levels for prolonged periods of time. Common complications include blindness, kidney disease and/or failure, and amputation of the extremities, seizure, low blood sugar (hypoglycemia) or high blood sugar (hyperglycemia). These complications may occur at any time and without warning. If hypoglycemia or hyperglycemia does not receive prompt treatment, it may result in death [11-14].
Hypoglycemia unawareness is a significant problem among people with diabetes. [15-20] found those at highest risk of severe hypoglycemia had episodes of critical low blood sugars and previous unawareness. Furthermore, there was a significant 6-9-fold increased risk of severe hypoglycemia related to impaired hypoglycemia awareness.
Problem Statement
Inability to detect or recognize symptoms of diabetes emergencies, particularly hypoglycemia, can increase mortality (Tsujimoto, et al., Prediction of 90-day mortality in patients without diabetes by severe hypoglycemia: blood glucose level as a novel marker of severity of underlying disease, 2015). Diabetes affects 30.3 million (12.2% of all adults) adults aged 18 years and older (CDC, 2017). There are estimated 206.5 million drivers 18 years and older, which approximates to every 6 drivers (14.6%) have diabetes (U.S. Department of Transportation Federal Highway Administration [USDOTFHA], 2011). In the United States (U.S.) alone, the disease has reached epidemic proportions. With the most recent statistics from the Centers for Disease Control and Prevention (CDC) reporting 30.3 million Americans are affected by diabetes. This growing epidemic affected nearly 1.5 million new diagnosed Americans in 2015, however, there continues to be an estimated 7.2 million undiagnosed (CDC, 2017). Another 86 million have prediabetes. With continuing upward bound trends, the need for complication prevention and management is critical.
Commonly, DM requires lifestyle modifications and medications to control the blood glucose level. Many people experience hypoglycemia, or low blood glucose, levels in response to their treatment regimen. The prevalence of hypoglycemic episodes is surprising. In one study of “844,683 patients, 119,695 (32.2%) had at least one recorded hypoglycemic event” [20-25]. Equally surprising is the economic impact continuing to burden society. Quilliam, Simeone, [26-30] stated “the mean costs for hypoglycemia visits were $17,564 for an inpatient admission, $1,387 for an ED visit, and $394 for an outpatient visit.
Complications of diabetes can result in sudden altered cognition, slurred speech, impaired vision, agitation, erratic driving and increased risk of accidents, loss of consciousness, seizures and even death (ADA, 2014). [31] found that even “moderate hypoglycemia impairs driving safely” and drivers with diabetes have a “12-19% increased risk of a motor vehicle accident” (p. 263). Therefore, it is crucial to identify and treat diabetic emergencies timely. Often times, a driver may be pulled over due to erratic driving. The next series of steps and timeline is vital and can be detrimental to the health of a person with diabetes if emergent symptoms are not identified in a timely manner. The officer must determine if the driver is intoxicated or is under duress related to a medical emergency. To determine this, the officer has been trained to employ standardized field sobriety testing. If the driver is cooperative, this may not take an extremely long time, however, if the driver is experiencing low blood glucose, he may not be cooperative and even exhibit belligerent and combative behavior. Indeed, this would be a hindrance in critical, timely medical attention and could endanger a life.
National Level: In 2016, the World Health Organization (WHO) released its initiative for World Health Day. A call to action to combat diabetes, beef up prevention measures, increase efforts to detect disease and commit to treatment (WHO, 2016). Although law enforcement officers are not healthcare providers or members of a healthcare team, the global call to action did not eliminate anyone. Community workers are even being utilized in the education process.
The ADA recommends law enforcement training on diabetes emergencies. They have released a short 20 minute training video in stemming from maltreatment of people with diabetes. The ADA also provides a training curriculum designated to educate law enforcement on the basics of diabetes, diabetes emergencies (hypoglycemia and hyperglycemia), behaviors under duress, treatment and management options, and recognition of common diabetes supplies [32].
As aforementioned, the lack of training in diabetes emergency responsiveness has been highlighted as the cause for many of the cases of extreme force, fatalities, and maltreatment. In correctional facilities, prisoners have also suffered the consequence of lack of law enforcement training for diabetes. Preventable complications and fatalities have occurred as a result. The ADA supports training for law enforcement and released a statement in 2014 recommending all “correctional facilities should have written policies and procedures for the management of diabetes and for training of medical and correctional staff in diabetes care practices” (ADA, 2014). The ADA released position statements on importance of training in response to diabetes emergencies, developing a training program to facilitate the sensitive response time in diabetes emergencies. Several cities and states have since implemented or adopted ADA’s Officer Assist training, including New York and Philadelphia, Pennsylvania (ADA, 2014). The ADA and Endocrine Society’s “Hypoglycemia and Diabetes” Report (2013) jointly addressed measures for providers to institute for safe driving practices when educating patients [33].
State Level: The Diabetes Foundation of Mississippi’s (DFM) website eludes to providing “free in-service for all law enforcement officials statewide,” however, there is no data to support this information. When discussed with a MHP PAO, he stated he was unaware of that service and had not been contacted to receive the service. Contact with the DFM was attempted, however there has been no response at this time.
Training law enforcement officers is not a new concept. Each officer of the MHP attends a rigorous 26-week academy with emphasis placed on physical and academic content. The MHP requires officers to obtain continuing education hours like many medical professionals. Due to assuming a first responder role, often times, law enforcement is first on the scene. [34] expressed because of competing medical training programs for law enforcement, the type of training should be related to situations encountered in the field. With the prevalence and incidence of diabetes on the rise, the demand for MHP officers to be equipped with knowledge to identify diabetic emergencies is paramount.
City and County Level: Upon discussion with local police department (GPD) and Sherriff’s Department (LCSD), sadly, nothing is being done to promote diabetes emergency awareness among GPD or LCSD. MHP is interested in pursuing training and compliance. MHP is supportive of efforts to educate law enforcement on diabetes awareness and emergencies.
MHP District headquarters is located in a rural county in the Mississippi Delta. This organization stated they have the most to benefit from this training due to the vast rural territory they cover. Local authorities in the county and city are situated near a hospital, however, some territories covered by MHP is over 30 miles from the nearest hospital or town employing EMS. There are no current policies or procedures in place, nor quality improvement measures, monitored at MHP regarding diabetes awareness training. Discussing the proposed project, a representative of MHP expressed interest in the training and reported a valid need for the training. His plans are to discuss this at their district meeting in October.
Global Level: Diabetes is a rapidly growing epidemic globally. From the latest reports (2014) it affects an estimated 422 million, nearly eight and a half percent (8.4%) of people globally (Diabetes, 2017). WHO projects DM to be the seventh leading cause of death by 2030, although the CDC already reports DM as the seventh leading cause for the death in the U.S.?
National Level: In the United States (U.S.) alone, the burden of DM affects a staggering 30.3 million (9.4%) people (CDC, 2017). Of the 30.3 million, the CDC estimates 23.1 million are diagnosed while the remaining 7.2 million (23.8%) continue to go undiagnosed. Nationwide statistics report DM affects older adults more often than the younger population. Adults 65 years and older account for 25.2% of diabetics. Among adults 18 years and older, the prevalence was highest among American Indians and Alaskan Natives (15.1%), non-Hispanic blacks (12.7%), and Hispanics (12.1%), than Asians (8.0%), with the lowest prevalence among non-Hispanic whites (7.4%) (CDC, 2017). Diabetes shows no bias, affecting both men and women, young and old. In 2014, DM was listed as the seventh leading cause of death, which was unchanged from 2013 [35]. The total deaths related to diabetes in 2014 was 76,488 (2.9% of total deaths). The CDC further acknowledged “significant increases” in unintentional injury related deaths (135,928) in 2014. These included unintentional injuries from motor vehicle accidents, which accounted for 33,736 deaths, equating to 16.9% of deaths from injury [36].
Between 2003 and 2009 the Bureau of Justice Statistics calculated 525 reports of arrest related deaths from intoxication. This accounts for 11% of intoxication related arrests resulting in death [37]. In 2015, it was estimated that 29% (n=10,265) of the driving population died in alcohol related crashes [38].
In 2016, Nunes, et al, estimated 32.2% of the population studied had at least one hypoglycemia event (Nunes, et al., 2016). With use of this information, if the CDC reports 30.3 million people have diabetes, then it can be deduced that almost 1 million will have at least one hypoglycemic event (n=975,660).
According to the National Law Enforcement’s Memorial Fund site (2017), there are currently a total of 900,000 officers in the U.S. This equates for every one police officer, there are approximately 34 diabetics. Diabetes continues to impact public health as direct medical costs continue to rise attributed to care and lost productivity. America’s Health Rankings reported diabetes costs rose 41% from 2007-2012 and with cases of prediabetes and undiagnosed diabetes projected direct costs estimated at $322 billion for 2012 alone (UHF, 2017).
State Level: In 2015 in Mississippi, DM affected more than 333,026 people, propelling the state into a first placed ranking for diabetes for the first time, according to the Mississippi State Department of Health (MSDH). This represents a state total of 14.7% of the population. In addition, it claimed 1,091 lives in Mississippi for the 2015 year (Diabetes in Mississippi, 2017). With the ever-increasing epidemic rates, Mississippi significantly surpasses the national average of 10% [39].
Currently in MS, the MHP is operating at a critical low. Full at approximately 700 officer capacity, the state only has about 500 officers at this time. The MHP has been allotted budgeting for an academy for 2017-2018. Typically, the academy enrolls 150 cadets, however, most graduating class sizes are less than half due to the physical and academic rigor of the program. There is one MHP officer to every 667 diabetics in MS.
County Level: Leflore County, Mississippi is situated in the delta, with a population of 29,856 people (US Census Bureau, 2016). The county diabetes prevalence rate is listed at 16.1% for ages over 20 years old (Leflore County, MS, 2015). Institute for Health Metrics and Evaluation (IHME) revealed mortality for diabetes related disease was 95.9 for females, 113.8 for males per 100,000 population. A transport injury mortality was rated at 16.8 and 40.4 per 100, 000 for females and males, respectively (IHME, 2016). There is an average commute to work time of 17 minutes [40]. No data is listed for transportation injury due to diabetes emergencies.
The ratio of law enforcement officers in the county to population is 1:7.5. However, the ratio for state police (n=25) to population of the county is 1:1,194. With a population of 16.1% (n=4806) of people with diabetes, there is a 1:192 MHP to people diagnosed with diabetes ratio. All are over driving age indicating a need for MHP to be educated on diabetes emergency symptom recognition. According to a source at the local hospital, there were 78 occurrences of hypoglycemia diagnoses in the past year requiring treatment, equating to 1:61 ratio of hypoglycemic events occurring in the population of people with diabetes.
Economic Burden
The devastation of diabetes expands extensively beyond diagnosis. It triggers a cascade of complications related to uncontrolled blood sugar, impacting quality of life and becoming a significant financial burden. In 2013, the economic burden of DM for Mississippi was $3.4 billion. With individual out-of-pocket expenses totaling $303 million (Diabetes in Mississippi, 2017). The CDC reported in 2014, the number of physician’s office visits with diabetes as a primary diagnosis were 30.3 million and Emergency Department visits accounted for 14.0 million (CDC, 2017). DM is a disease caused by insufficient insulin production resulting in high blood glucose levels. High blood glucose levels lead to many complications affecting major organ systems.
Complications of diabetes affect vision, sensation, cognition, and often affects the circulatory system, resulting in major organ damage. Commonly DM requires lifestyle modifications and medications to control the blood glucose level. Many people experience hypoglycemia, or low blood glucose, levels in response to their treatment regimen. The prevalence of hypoglycemic episodes is astounding. In one study of “844,683 patients, 119,695 (32.2%) had at least one recorded hypoglycemic event” [41-46] stated “the mean costs for hypoglycemia visits were $17,564 for an inpatient admission, $1387 for an ED visit, and $394 for an outpatient visit. Diabetes complications impact a person’s quality of life. With decreasing vision, sensation and cognition one may experience with diabetes, it can result in traumatic injuries related to falls, fractures, burns, traffic violations or even death.
Although DM is a preventable disease, in 2015 the CDC estimated that 84.1 million Americans had pre-diabetes; a representation of 33.9% of the U.S. population over the age of 18 years old. This appears to be a growing trend. The Institute for Alternative Futures (IAF) predicted “Between 2015 and 2030. The total number of people with type 2 and type 1 diabetes will increase by 19,629,000 to 54,913,000 people, a 54% increase. The cost of diabetes in 2015 dollars will increase to $622.3 billion, a 53% increase” [47].
The CDC’s initiative to end devastation of diabetes is a considerable undertaking. They have developed a division devoted to diabetes translation. Their mission is to “reduce the preventable burden of diabetes through public health leadership, partnership, research, programs, and policies that translate science into practice” (About CDC's Division of Diabetes Translation, 2015). Two of the divisions priorities include: “enhancing and improving community and environmental strategies to support people with diabetes and building DDT capacity for communication, evaluation, marketing, policy, and partnerships” (About CDC's Division of Diabetes Translation, 2015).
Rationale for the Proposed Project
This project sought to address and evaluate the effectiveness of providing diabetes emergency training for law enforcement. Many states have no formal training implementation plan. Mississippi has a voluntary reporting system similar to New Jersey for licensure, but no laws or requirements for law enforcement diabetes emergency response training. With the sensitive political climate involving law enforcement and citizens, the need to promote justice and support the community is vital to unity, strength, and better outcomes. The project proposed to bridge the gap of lack of training and awareness, providing diabetes emergency response education to law enforcement officers. The goal of this research was to prevent delay of emergency medical attention, which may jeopardize life for those with diabetes.
As recent as 2015, Florida’s governor instituted mandatory online diabetes awareness training for law enforcement in response to a tragic fatality resulting from a diabetic emergency [48]. Other states, such as New Jersey, have adopted legislation allowing the voluntary reporting of the diabetic condition for licensing for protection and prevention of delay in medical care (New Jersey Diabetics Get New Protection from DUI Charges, 2017). Yet another case in New Jersey cited lack of training as the factor for two officers’ use of excessive force. The officers stated they had never received any training identifying diabetes emergencies or diabetic shock [49]. In February 2012, Nevada police assaulted a man with diabetes mistaking him for a drunken driver [50]. There have been several accounts of people with diabetes being tased. The ADA has an advocacy group of legal and medical counsel devoted to end the mistreatment and knowledge deficit related to diabetes. In 2007, ADA released a law enforcement training video to increase awareness and end discrimination. The U.S. Department of Transportation issued problem statements including lack of standardized procedure to detect impaired drivers. They recommended development of training and checklist to identify impaired drivers (Problem Statements, n.d.).
Goals: The purpose of this research was aimed at educating local law enforcement regarding diabetes emergencies and treatment, improving hypoglycemia symptom recognition as compared to intoxication. By evaluating if diabetes emergency training among law enforcement improves recognition of hypoglycemic or hyperglycemic emergency crises, it was hypothesized outcomes of care will improve for the driver with diabetes. Objectives of training included.
Expected Outcomes: Proposed outcomes were centered on the goals and objectives above. This research hypothesized the following expectations.
Due to the physical, emotional, and psychological toll on the patient with diabetes, education is needed throughout our communities to promote health and wellbeing and to prevent life threatening complications. It was expected by providing diabetes emergency education to law enforcement, complications could be treated and managed in a timely manner. Furthermore, a life could be saved. Past research suggests diabetes causes vascular complications, including organ damage and myocardial infarctions. If law enforcement is trained to identify and address these emergencies, there may be reduced fatalities and co-morbidities than if treatment is delayed. Potentially assuming a first responder role, there may also be a diminished financial strain on the patient and society. When these emergencies can be identified, it will eliminate the assumption of driver intoxication and agitation, thereby limiting provocation of natural instinct to use force to subdue these diabetic drivers. In turn, this will eliminate the potential physical harm to the diabetic and litigation to the department or state agency.
Materials and Methods
Searches were conducted using a variety of online search engines for scholarly works and published articles. Sites utilized included PubMed, Sage Journals, National Guideline Clearinghouse, National Institute of Health, American Diabetes Association, Centers for Disease Control and Prevention, the U.S. Census Bureau, National Highway Traffic Safety Administration, National Institute of Diabetes and Digestive and Kidney Diseases, Oregon Health Authority- Public Health Division, Texas Diabetes Council, and The Department of Health and Human Services. Journal searches included The Journal of Internal Medicine, Diabetes Care, The Lancet, Diabetic Medicine, Journal of Pharmacology and Therapeutics, Emergency Medicine, Journal of Safety Research, Diabetology, Disaster Medicine Public Health Preparedness Journal, Injury Epidemiology, Canadian Journal of Diabetes, and Prehospital Emergency Care. Other searches included incorporation of court cases and legal information regarding care, or lack of, of individuals with diabetes.
Inclusion criteria comprised of education of law enforcement, guidelines for training law enforcement, education of first responders, guidelines for training school employees who are not licensed healthcare professionals, training protocols, developing a curriculum for diabetes awareness training, community health awareness, diabetes education, diabetic emergencies, driving and diabetes, hypoglycemia and safe administration of naloxone by police officers.
Exclusion criteria contained diabetes symptoms in police officers, diabetes self-management, traffic stops, current strategies to diagnose and manage diabetes, police referrals to motor vehicle board, traumatic injuries in diabetic patients, non-research-based articles, blogs, and non-reputable websites. Rationale for search strategies limits contained evidence-based journal articles in support of education of diabetic emergencies and management strategies, education of law enforcement, tactical medicine and curriculum for diabetes emergencies.
Information Sources: Eligible information was obtained through searching various databases, including but not limited to PubMed, Cochrane Database, CINNAHL, and Medline. Hand searches were also conducted throughout each included and excluded article using the reference list. Statements of support and position were reviewed and utilized from the WHO and ADA regarding diabetes and driving. Contact was made with the American Diabetes Association legal team regarding use of the Assist Officer Program and Law Enforcement Training curriculum. Permission has been sought for use of the curriculum with modification of not utilizing the attorney developed content. There has been no formal data collection to validate or assess reliability of the curriculum or measurement tool. Eligible articles are dated from 2014-2016 and gray literature from 2009-2017. Older literature that was reviewed and deemed relevant dated back to 2000.
Rating Tools: The AGREE II rating tool was used for synthesis of material validity and relativity, as well as, evidence.
Study Selection Process and Results: Articles were reviewed and narrowed for inclusion or exclusion based on article title, abstract objectives, results or conclusions, method of collection, and type of research. Most inclusion articles addressed quantitative evidence. Data extraction involved reviewing researchers’ questions, study limitations, population, sample size, study design, and outcomes. Hand searches were also conducted by reviewing of reference lists and cited articles. Contact with representatives of the American Diabetes Association was made to discuss curriculum content. Contact was attempted with Texas Diabetes Council, Diabetes Foundation of Mississippi, Florida Law Enforcement, and Philadelphia Police Department for literature review of internal research using the ADA curriculum, without success.
Limited studies pertinent to research were found during the literature review and synthesis. Of several hundred articles found, less than 50 contained information specific to research topic and objectives. Gray literature was included in the literature synthesis, as well as unpublished student research on tactical medicine indicating the need for law enforcement to have basic medical knowledge and skills.
Summary of Evidence: Hill, Rybar, Stowe and Jahns (2016) conducted a study to assist law enforcement with skills to identify and manage medically impaired drivers. Partnering with California Highway Patrol and the University of California, San Diego, Training, Research and Education for Driving Safety (TREDS), the researchers developed a training curriculum and utilized a roadside screening tool assessing for disorientation among drivers, developed by TREDS. Although their study focused on reporting older drivers to the Department of Motor Vehicles (DMV), the training covered medical conditions and assessment tackling chronic disease complications including hypoglycemia and hyperglycemia. They surveyed 2,018 officers with 1,905 (94%) attrition finding their pre-training confidence perceptions in ability to identify disorientation and impairment were high (67%); however, the post-training questionnaire indicated their ability to recognize medical impairments was increased by at least 50%. Needless to say, pre-training participants were overly confident in their skills. They concluded there were changes in knowledge level and intent to utilize the TREDS tool in the future. Overall, they acknowledged the need to incorporate training and screening to assist in identifying and managing medically impaired drivers. They reported the study was generalizable and would be useful in younger populations with medical impairments [51-55].
Recently in 2016, law enforcement was trained on identification of opioid overdose and administration of Naloxone use for opioid overdose. [56] concluded officers were able to correctly identify overdose symptoms and administer Naloxone “without adverse events or outcomes” and “police officers are receptive to training” and intervention [57]. Of the more than 900 participants, 126 doses of Naloxone were used in 18 months, among 89 different officers. Just as [56] concluded, desperate times call for desperate measures. Alternative plans addressing epidemics, such as opioid and diabetes, should include first responders and law enforcement for time-sensitive treatment measures, prevention of aggravating complications, and exposure to the disease. Although the WHO, CDC and ADA strongly recommend diabetic emergency training, conversely, there is very limited research on providing this training to law enforcement or the impact on patient outcomes [56].
Engelman and Deardorff (2016) evaluated law enforcement training as first responders in cultural competency related to domestic violence and the deaf. Providing a two-hour training workshop, they assessed participants’ satisfaction with the training, response skills, attitudes and knowledge. Of the 19 participants, they found significant differences in knowledge based pre and posttest scores and self-efficacy perception.
Wolf-Fordham, Twyman, and Hamad (2014) evaluated the use of online training format to educate law enforcement and other first responders when providing emergency services to individuals with disabilities. They noted there were benefits of the asynchronous educational format, such as the ability to provide education to a larger population, ability to enhance education by providing “immersive, participatory, realistic scenarios” (p. 535), repeat review and corrective action, cost-effectiveness, and reinforcement of knowledge and skills. They added the CDC and Department of Defense believe this to be a beneficial means to education citing the CDC indicated simulation trainings should be utilized in public health education (Wolf-Fordham, Twyman, & Hamad, 2014). Of the 28 participants, 36% completed the research study there was a “very large effect for knowledge gain” correlating to 1.4 and 2.3 overall gain. They also note that this significant knowledge gain is measured by effect sizes that range .2-.8, with .8 representing the largest effect. Overall, there was an 89% satisfaction rate with the educational format.
The National Highway Traffic Safety Administration (NHTSA) “Medical Conditions and Driving: A Review of the Literature (1960-2000)” report stated, in 1990, [57] studied hypoglycemia prevalence, finding 98% confessed to hypoglycemic events and 73% reported having monthly episodes [58]. Further finding, 40% of outpatient drivers in Australia reported hypoglycemia while driving, and 13% of those reported an associated crash while hypoglycemic. In 1982, [59]., retrospectively examined 94 insulin dependent drivers. They estimated that 68% of the participants had hypoglycemia symptoms while driving [57]. This report later concluded the number of hypoglycemic events directly correlated with the number of crashes over a five-year period. Further acknowledging the likelihood of crashes increased two-fold with reports of two or more hypoglycemic episodes per year [57]. Although in older in citation, this material is found to be relevant to this research.
Guidelines
The ADA (2014) produced “Helping First Responders Spot Lows.” This training was instituted to educate law enforcement how to distinguish hypoglycemia from intoxication. Several cities and states, including Philadelphia, Sante Fe, Indiana and Mississippi have provided education to this training to law enforcement. In 2012, Margrett Davis, a nurse in Mississippi, teamed up with a local university and ADA to implement the training to local city law enforcement. She stated, “It’s a way of bridging a gap between the community and the police” [60]. Contact was attempted to reach Mrs. Davis, although unsuccessful.
Oregon law acknowledged that hypoglycemia can lead to complications and warrant life saving measures. Oregon Health Authority developed a “Training Protocol: Emergency Glucagon Providers” to educate unlicensed individuals to respond to hypoglycemic crises. Although this training could be implemented in various settings, the most likely settings would involve the school systems. This training protocol provided a brief overview of diabetes, causes of hypoglycemia, recognition of hypoglycemia symptoms, and administration of glucagon in severe hypoglycemic cases. To ensure proper administration, the training session required return demonstration. It also had an open book test at the end of the training. The trainer requirements included participants must be a licensed physician, nurse practitioner or nurse. The trainee must be at least 18 years of age [52]
In 2005, the Texas Diabetes Council (TDC) assisted in developing a curriculum for training school employees in caring for children with diabetes. Revised in 2009, the curriculum incorporates guidelines for school setting with and without school nurses. Training content reviews individual health plan (IHP), signs and symptoms of low and high blood glucose levels, corrective action steps individualized to the student, performing skills for monitoring blood glucose, insulin and glucagon, and nutritional considerations. A written test of 25 questions with a passing score of 78% must be obtained to permit the learner to advance to the skills performance section. The skills must be performed until successfully demonstrated. TDC suggests annual review of the didactic content and skills. Once trained, the system may conduct a brief overview on an annual basis, but the trainee must complete the written exam each year and if an unsuccessful score, less than 78%, the trainee will require classroom education/didactic training. On annual review of skills performance, if the trainee is unsuccessful, they must complete additional skills training [59].
In 2016, the Endocrine Society released a blueprint to address the incidence of hypoglycemia after determining hypoglycemia increased mortality risks. In this article, Dr. Amit Akirov stated hypoglycemia can occur in people with or without diabetes, adding to the magnitude of potentially increasing incidence (Endocrine Society, 2016) [60]. In this study, they found of 3,000 patient’s hypoglycemic events, by the end of the study nearly 32% had died. They concluded hypoglycemia was associated with increased mortality risks and severe hypoglycemic episode risks were similar to those treated with insulin. They created a Hypoglycemia Quality Collaborative (HQC), further establishing initiatives to reduce the “gaps in care, advocating for increased focus on hypoglycemia and improving quality of care for patients who experience hypoglycemia” (Endocrine Society, 2016) [60]. The HQC report defined six key strategies to aid in reduction of hypoglycemia incidence:
The ADA and Endocrine Society’s “Hypoglycemia and Diabetes” Report (2013) jointly addressed measures for providers to institute for safe driving practices when educating patients [61]. It suggested a reminder not to drive when the blood sugar is low (less than 70mg/dl) and use of a screening tool to assess patient risk for driving associated with hypoglycemia. In their hypoglycemia patient questionnaire, the group asked, “if the patient checks the blood sugar before driving and has the blood sugar ever been less than 70mg/dl while driving?” [61]. It then addressed the number of instances of hypoglycemia while driving since last visit and in the last year.
Court Cases: Austin (2010) discussed the importance of considering alternative strategies to raise awareness and manage severe hypoglycemia. She reported that a court case in 2009, implicated a 19-year-old male, with diabetes, for assault after paramedics responded to a call to his home. Reportedly, he struck the paramedic several times in the face while suffering from severe hypoglycemia. In 2003, due to Rosen v. Philadelphia, the city of Philadelphia was required to make a training video after “failure to provide appropriate care to people with diabetes” [62]. She cited these “sobering” examples of lack of hypoglycemia symptom awareness among paramedics and law enforcement [62].
In 2008, Doug Burns, a Mr. Universe winner, was experiencing a severe hypoglycemic episode outside a Redwood City movie theatre when he was pepper-sprayed and beaten with a police baton. Burns’ wore identification for his diagnosis of diabetes. He sought monetary damages, attorney’s fees and court orders for mandatory training of diabetes emergencies [63] established an “Introductory Guide for Attorneys” in response to inappropriate law enforcement acts. Citing court cases, Fech and Murray, expressed the importance of proper training of law enforcement to prevent maltreatment or deaths of individuals with diabetes. In the Supreme Court case of City of Canton v. Harris, the court maintained an individual has the right to impose liability of a municipality for lack of or deficient training of municipal employees who encounter individuals with disabilities, including diabetes [64]. The case must explicably show how the injury is related to the charge of inadequate training.
In Padula v. Leimbach, a driver was experiencing hypoglycemia that was not determined by the officer. The officer believed the driver was intoxicated due to incoherent speech, flailing arms, then unresponsiveness. Eventually, the ambulance was called and the emergency personnel noted the hypoglycemic crisis, administered dextrose and transported to the hospital, the decedent died approximately a month later [64].
In Adams, a driver with diabetes experienced a hypoglycemic attack leading to blackout. After a chase ensued, his vehicle eventually stalled on an embankment, at which time police “forcibly” removed his from his window and restrained him on the ground using handcuffs. The driver argued failure to adequately train the officers lead to use of excessive force and lack of detection of a medical emergency [64]. In 2015, Florida’s governor Rick Scott instituted a mandatory diabetes training course in response to the death of Arthur Green, Jr. Titled, “Diabetic Emergency and Officer Response,” this training can be accessed online and the officer may receive two (2) education credit hours (Florida Department of Law Enforcement [FDLE], 2015). In Florida, officers are required to obtain 40 education and training hours for certification. Currently, this program begins with statistics of diabetes prevalence across the country, supporting the need for preparation of diabetes emergencies. This training discusses the importance of recognizing diabetes emergencies to prevent permanent complications and liability of self and agency (FDLE, 2015).
In 2014, Alan Yatvin and Dr. Daniel Lorber presented a training to New York City Police Academy and discussed legal implications of failure to train. He began his presentation by screening diabetes videos from the NYPD. He later led into the legal cases. One notable case, Graham v Connor in 1989 established use of force theory that necessitated violation of free person under the Constitution’s Fourth Amendment. He reminded officers that Graham, an individual with diabetes, was pursued after “hastily” leaving a store during a hypoglycemic reaction. Witnessing this, Officer Connor pulled the car over to investigate. During the investigation, Graham’s hypoglycemia worsened and Connor called for backup. When other officers arrived then handcuffed Graham. Graham’s driver, Mr. Berry explained this was a low blood sugar reaction without officers heeding the warning. It was later determined that Graham had no wrongdoing at the store. With use of excessive force, Graham sustained a broken foot, injured shoulder, cuts and bruises [65].
Limitations and/or risk of bias
In the research studies, there was no acknowledgement or perception of bias. In the gray literature, the ADA utilized volunteers for legal counsel when representing people with diabetes discrimination claims. There is no claim of bias, however, in reviewing the court cases and sites, there was often a distinct detection of accusation of wrongdoing of law enforcement.
Conclusion
Throughout the literature synthesis and review, it has been established hypoglycemia can lead to complications, increasing the risk of mortality. Episodes of hypoglycemia are becoming more predominant in driving. Some drivers experience unawareness to an emergent hypoglycemic event, thereby, increasing the severity of the emergency. As the prevalence and incidence of diabetes, prediabetes and hypoglycemic events without diabetes increases, it necessitates the ability to recognize hypoglycemia symptoms and diabetes emergencies. With the support of various state laws and national organizations, such as the ADA, Endocrine Society and NHTSA, education should be provided to law enforcement in identifying and recognizing critical emergent states of drivers with diabetes, to prevent delay of care resulting in permanent complications and increased mortality.
Implementation Plan
Providing diabetes emergency training to first responders can limit delay of care by rapid symptom recognition. Evidence shows providing education to law enforcers enhances knowledge in tactical medicine. Research has shown untreated hypoglycemia is detrimental to patients and drivers alike. Detrimental outcomes can be reduced by providing diabetes emergency training to law enforcement.
Project Design
This quasi-experimental project was designed to assess pre- and post- instruction knowledge of diabetes emergencies. Groups of comparison comprised a pre-knowledge group and a post-knowledge group. Variables included those who were diagnosed as a person with diabetes prior to instruction, those who had connections to others who were diagnosed with diabetes, participants with no prior knowledge of diabetes, participants with prior experience of more than one year, and participants with less than one-year experience. This research attempted to answer if providing diabetes emergency training to law enforcement increases the knowledge base to recognize diabetes emergencies in drivers with diabetes.
Theoretical Frameworks
Interpersonal (Nursing) Relationship Theories are designed to focus on the development of the nurse-client relationship and establishment of influential factors guiding adaptation. Ida Jean Orlando Pelletier (Orlando) theorized that effective care was delivered as a result of the nurse’s ability to identify and meet the patient’s immediate needs. The Dynamic Nurse-Patient Relationship Theory summarizes the involvement of interpersonal elements where the person’s behavior indicates a need, requiring the nurse to react and implement a plan to meet the person’s need.
Major concepts of Orlando’s nursing theory integrate human involvement, implied health, keen nursing awareness, need, and immediacy into the process of nursing [62]. The relationship between the nurse and patient builds a foundation for this process design. Keen nursing awareness signals the human/individual is in need, if that need is unspoken. The immediate deliberate actions of the nurse then address the need of the individual, which provokes the individual’s response. It is implied that health is a constant balance. Need only arises when the individual’s health is out of balance, also viewed as required help. The ability of the nurse to adapt to the changing health status of the individual and the individual’s ability to adapt to the intervention is the functional component of Orlando’s design.
Orlando further expressed the nurse’s actions were either automatic or deliberative. Automatic processes limited the nurse’s independence. These processes included doctor’s orders, care routines or foundational principles in health protection of the patient. She concluded; it was the deliberative nursing processes that determined whether the patient’s needs were met. Deliberative nursing actions include: client centered communication of instructions, suggestions, education, information, explanations, decision making, and altering the client’s immediate environment [63].
Orlando’s Dynamic Nurse-Patient Relationship Theory uniting with a cognitive learning aspect, affords the opportunity to impact the learner’s knowledge by assessing readiness to learn (motivation), incorporating valuable experiences, and interpreting discovery of new knowledge. The development of the learning process takes into account the learner’s perception, interpretation and response. Learning is enhanced through engagement of diverse viewpoints and perceptions, then translated into practice through understanding, problem solving, critical thinking, and evaluation [63]. ???????
Applying this learning process to my clinical problem of delayed care of diabetic emergencies could result in improved recognition of diabetic emergent symptoms by motivating law enforcement to consider erratic driving or alteration of driver behavior as a potential diabetes emergent event. By altering the learner’s perception that abnormal behavior of agitation, aggression, slurred speech, erratic driving, decreased cognition, and inability to focus is strictly related to intoxication, he then may interpret the driver having a medical condition, thereby utilizing new knowledge of signs of diabetes emergent crisis and quickly refer for medical help, or if allowed provide emergent treatment while first responders are notified.
Using Orlando’s theory in translation to practice would include a two-part application. Background of the nurse (myself) to recognize the diabetic driving population’s immediate need of treatment for hypoglycemia and translating it to provide community health education approach of law enforcement. Now, displacing the “nurse-patient” and transitioning to nurse-law enforcement-patient model provides the opportunity for the nurse to train community professionals (law enforcement) to detect an association between hypoglycemia symptoms and intoxication. Next, with this recognition, law enforcement knowledge evolves and identifies the behavior as a (need), considering the presenting impairment may be related to diabetes versus intoxication. Appraisal of the new knowledge allows law enforcement the ability to distinguish between diabetic crisis and intoxication (reaction). After confirmation of findings, law enforcement applies education and treatment (if applicable) or alerts an emergency response system (action). This concludes with the patient receiving care in a timelier manner (action appropriate to person’s need) rather than enduring field sobriety testing prolonging need for emergent care. These pertinent process elements provide a framework for deliberate actions in advocacy and caring for diabetic drivers, thus allowing for increasing awareness of the driver with diabetes emergencies among law enforcement, coinciding with Endocrine Society’s HQC blueprint initiative for promoting hypoglycemia awareness in public health forums (Figure 1).
RE-AIM Model
The RE-AIM model was used to assist in development of planning and evaluation of this public health concern. Although it was originally designed more for evaluation of outcomes, it has been used as a plan to incorporate new knowledge into practice according to literature. King, Glasgow and Leeman-Castillo (2010) evaluated the efficacy of RE-AIM’s use in environmental change approaches to enhancing population health. This model proved to be “applicable to build environment interventions and provide added value given their usefulness in anticipating impact, planning for sustainability, and addressing unexpected or adverse consequences” (King, Glasgow, & Leeman-Castillo, 2010). The goal of RE-AIM is to highlight the sustainability of evidence-based practice (EBP) implementation [64] discussed the framework’s five steps into translation:
The RE-AIM model was an appropriate choice to guide the implementation of this DNP project that had the goal of improving diabetes symptom recognition of law enforcement. This translational researcher Reached the target population (law enforcement) by incorporating diabetes awareness training curriculum at their local district headquarters. Effectiveness of this intervention was established by administering a pre-test to law enforcers to determine their understanding of diabetes symptomatology. A post-test was administered to the participants following the training curriculum to determine if the intervention made a difference at a .05 alpha. Adoption of the training involved meeting with administrative stakeholders to discuss the: prevalence of diabetes, exposing the problem of lack of recognition of emergent crises symptoms resulting in officer litigation and patient death (in some cases), and offering a solution to the problem (training for law enforcement).
According to the RE-AIM model, Implementation of this project informed the learner of basic, but pertinent content related to diabetes. Discussion and instruction of types of diabetes, diabetes emergency symptoms and behavior, immediate response to diabetes emergencies and further management protocol were delivered to each participant in the same manner. This training was presented in a sensitive manner as to eliminate any bias or mechanism of defense from audience. Maintenance of the intervention was based upon the utilization of annual training, tools to identify diabetic symptoms, and proposed policy change throughout the organization (Figure 2).
PICOT Questions
This project sought to answer several questions:
1. Does providing a one-time diabetes emergency training to the Mississippi Highway Patrol increase their knowledge of symptom recognition after instruction?
2. Does providing diabetes emergency training to MHP increase their ability to recognize commonly used supplies of a person with diabetes after instruction?
Sample Size: This project was implemented in a sample size of 56 participants. There are nearly 500 state officers in the MHP. This projected sample size represented approximately 10% of the current state officer population. Participation was voluntary. Sampling was based on a selection of volunteers of the MHP. Inclusion criteria comprised any current sworn officer of the MHP. The experience level included novice to expert. Both genders were included. Participants with and without diabetes were allowed to participate. Exclusion criteria included members of the MHP who were not currently active in duty or suspended for any reason.
Setting: The group designed training curriculum was provided at District headquarters, in two rural counties in Mississippi. The districts have technologically sound training rooms available to meet the project needs, as well as capacity. The headquarters had approximately 63 sworn officers who were not on military or sick leave.
The MHP’s function is to protect and serve the public. Their motto is courtesy, service and safety. Their primary duty is to patrol the highways of the state presiding over jurisdiction of the state. It is their job to assist local law enforcement precincts with emergency response and management at the request of the governor (Mississippi Highway Patrol, 2017).
The MHP officers are required to obtain 24 continuing education hours for certification annually (Mississippi Peace Officer Standards and Training, 2017, p. 99). Most of the education hours are obtained throughout various training sessions on site or through PAOs. Some educational opportunities are provided in an online format. A local PAO sought the prospective interest of the directors, which was expressed as positive and willing to accept training. Further stating, he saw an immediate need for this type of training due to the current numbers of drivers with diabetes.
Expected barriers included providing education to a sizeable group ranging from 8-100, educating a vast territory with the same curriculum, and addressing the needs of a variety of knowledge bases and learners. These barriers were met by providing more than one training session for addressing the different levels and needs of the learner groups, specifically, the two districts. The vast territory was traversed from the local area to approximately 90 miles northeast.
Stakeholders: Key stakeholders included the upper level officers within the MHP. The MHP was seeking accreditation of their governing body. These members felt this training will further enhance their recognition and program, elevating them among other states. Other stakeholders included every MHP officer, by which this accreditation process will encourage acceptance of training. It was important for them to recognize the rapidly growing diabetes population and need for training to decrease any liability while in their custody.
Congruence of Organization to Project: As aforementioned, the current goal for the MHP strategic plan was to gain accreditation of the certifying agency. According to a local PAO, the continuing education meeting the needs of the public would assist in acquiring accreditation. This project was designed to provide an innovative approach to educate ways to promote safety, provide courtesy, and serve the public.
Recruitment Plan: Recruitment involved contacting the local district and speaking with the PAO, as well as the director, training Captain and Captain of each district. Contact was focused on discussing the project idea and plan to contact local officers and provide a training session at the district headquarters. A formal survey of interest of potential participants occurred. Due to this research being voluntary, it was important to allow for the participants to accept or decline the formal invitation to participate in the study. The potential participants were informed of the goals and objectives of the study. They were also informed of the length, process, and results of the study. They were apprised of the ability to withdraw participation at any time.
Evidenced Based Measures: The ADA developed a diabetes emergency training curriculum and videos (ADA, 2017). The measurement tool in this curriculum, The Diabetes Emergency Training Written Exam, required assessment of validity and reliability, which was performed through peer review of content validity and the use of Cronbach’s alpha assessing reliability. The research tool was used as both the pretest and posttest assessment. Modification was permitted to add a question to assess ability to recognize diabetes supplies. Permission was obtained to use the ADA training curriculum without modification, except to exclude if needed the legal advocacy section. Permission was granted by Sarah Fech-Baughman, legal consultant for the ADA. She assisted in the development of the curriculum. She is also serving as content expert on the project.
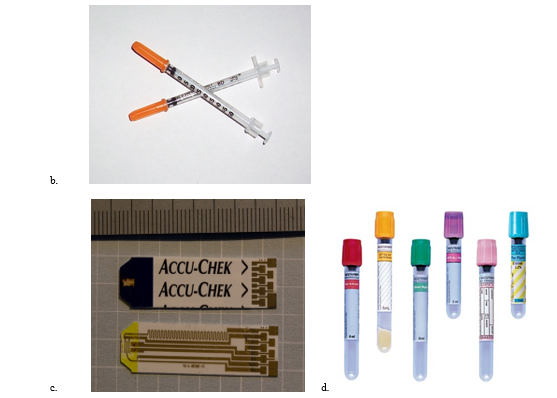
Question types included true or false and multiple choices answers. In modification of the pre- and post-test, a pictorial question was incorporated as well (Appendix A). The research tool posed a total of 14 questions. Using a scoring system of 100 points, the questions will be scored at 7.14 points each. To be determined successful, the participant should score a 75% or better. Questions are outlined below.
True or False:
Multiple choice:
Of the items below, which are not used by a person with diabetes?
Translation Strategies
My plan was to integrate toolkits into my research project by using the resources the ADA provides. Posters, handouts, videos and the “Assist Officer” handout (appendix B) were used. Toolkits are recognized by the AHRQ as supplemental information developed for promotion and transfer of knowledge into evidence-based specific practice recommendations. These toolkits encouraged utilization of practice recommendations and allows for reflection of the transferred knowledge, acting as a resource for review. I incorporated the ADA’s, Diabetes Emergencies (Appendix C), listing the signs and symptoms of high and low blood sugars. This tool was laminated to assist in maintaining integrity. This tool was intended as a resource to assist the law enforcement officers in identifying drivers with diabetes emergencies when used in the field. The toolkit also incorporated the ADA’s, Diabetes is serious: It can be life threatening handout (Appendix D). Lastly, providing an article from the ADA, Helping First Responders Spot Lows, served as a resource for the officers [65].
Results
Ethical review. An application to conduct research was filed with The Delta State University Institutional Review Board (IRB) after IRB training through National Institutes of Health. The IRB granted approval, on March 2, 2018, to conduct research under the exempt status. IRB Protocol Number was issued as 18-010.
Validity and reliability. Content validity was established through peer reviews of the tool. Consequently, six of the fourteen questions resulted a Content Validity Ratio (CVR) of 1.0. Two of the fourteen (14%) netted a CVR of 0.5. Four of the fourteen resulted in a CVR of .25. Six of the questions yielded a negative ratio of -1.0. Reliability was established using Cronbach’s alpha yielding an over score of .639.
Data analysis. Data was analyzed using SPSS software. Input data consisted of each participant’s demographic information obtained through survey and individual answers to the 14 questions on the research tool. Descriptive statistics were used to assess gender, experience and potential pre-knowledge of diabetes.
Proposed versus actual outcomes. Proposed outcomes included increased ability to recognize and distinguish diabetes emergencies from intoxication, providing visual aids of commonly used diabetes supplies will enhance identification of supplies by officers, officers who are diagnosed with diabetes or have connection to someone with diabetes will have higher pretest scores than those who do not have diabetes or a connection with someone who had diabetes, and MHP officers having more than one year experience will score higher on pretest than those who have less than one year experience. Actual outcomes revealed there was increased ability to recognize and distinguish diabetes emergencies from intoxication. The use of visual aids enhanced the officer’s ability to identify commonly used supplies of people with diabetes. It was found that having a pre-existing diagnosis of diabetes or knowing someone with diabetes did not result in a statistically significant higher score. It was also determined level of experience resulted in higher test scores of significant values.
Descriptive statistics. The population targeted consisted of all male participants. Age ranged from 22-60 years old. Years of experience with the Mississippi Highway Patrol ranged from less than one year (n=9) to more than 20 years (n=47). Throughout their years of experience, it was realized 20% of the participants have had any prior diabetes training. Only approximately four percent (3.6%) of the participants had been diagnosed with diabetes (n=2), however a majority (60.7%) had family member(s) with a diagnosis of diabetes. The number of diabetes encounters ranged from 0-15. Eighteen percent of participants have never encountered a person with diabetes involving their career duties. Seventy-one percent of participants had between one and five diabetes related encounters, while only two percent had up to 15.
Inferential statistics. Pretest and posttest correlations were analyzed through SPSS software. There was a positive correlation (r =0.530) resulting in a paired t test statistical significance (p=0.000). The null hypothesis, there will be no statistical significance between pretest and posttest scoring, was rejected. The level of significance was 0.00 using a related-samples Wilcoxon Signed Rank test. Fifty-six out of sixty-three male participants took part in the study, yielding an attrition rate of 89%. All completed pretest and posttest scores were analyzed at completion of collection. Pretest scoring range from 43.2-100% (n=1, n=2 respectively), with the majority scoring between 78.7-85.8% (n=10, n=13 respectively). Posttest scoring ranged from 57.4-100% (n= 3, n=13 respectively), with the majority scoring 85.8-100% (85.8 n=17; 92.9% n= 13; 100% n=13). Eighty-nine percent of the participants scored above 75% on the posttest.
Using a 95% confidence interval, it was determined the difference in the pretest and posttest scoring was statistically significant with a p value of .000 in the paired samples correlation (.530) and two-tailed t-test (.000) with 55 degrees of freedom. This indicates the training produced an overall knowledge improvement. The 14 test questions were categorized into either knowledge based or treatment-based questions. Of the two categories, significant improvement was noted in both the knowledge and treatment-based questions. Knowledge related questions yielded a range of significance from .000-.250. The treatment-based questions yielded a significance level of .000-.195.
Questions based on the meaning of diabetes, diabetes causes, definition of hyperglycemia, court ruling of Graham v. Connor, alerting emergency response system, lack of insulin production, definition of hypoglycemia, and identifying signs and symptoms of hypoglycemia were measured. Of the eight knowledge questions, four (50%) showed statistical significance representing improvement of knowledge in diabetes emergencies. The questions addressing significant improvement of knowledge including the true or false type: “Having diabetes means that you just need to control how much sugar you eat”, with a significance of .000 and “Because Graham v. Connor (1989) established the standard of ‘objective reasonableness,’ we cannot be held civilly liable for injuries resulting from using force to get control of a person experiencing insulin shock” with a significance of .000. Multiple choice type of question indicating knowledge gain included: “When the body does not produce insulin, the amount of sugar in the blood (increases, decreases, stays the same or none of the above)” with a p value of .000; and lastly, “Hypoglycemia is defined as (Very low blood sugar, Very high blood sugar, A lack of pancreas, Any of the above)” resulted in a p value of .029.
Four out of six (67%) treatment questions indicated officer improvement of knowledge related to diabetes emergency treatment. These questions measured the participant’s ability to treat insulin shock, assure driver’s access to supplies, recognize complications and offer treatment related to neuropathy, treat hypoglycemia, and identify supplies related to treatment of diabetes. Of these questions, there were two true false including: “Diabetes can be cured with diet and exercise” yielding a significance level of .003 and “You should allow a person/driver with high or low blood sugar or neuropathy to sit rather than stand during an on-the-street interrogation or in a detention setting” resulting in a p value of .000. Multiple choice questions that recognized statistical significance in improvement of knowledge included: “You respond to a call-in reference to a man staggering and acting bizarrely in a parking lot of a convenience store. Upon your arrival you discover the man has collapsed and is unconscious, but you observe a medical alert bracelet indicating that he has diabetes on his wrist. You should take all of the following actions except (Notify fire/rescue, Check the man’s airway and respirations to make sure it’s clear, Attempt to get him to wake up, Attempt to force some orange juice into his mouth to try to get his sugar levels up)” yielding a p value of .000 and a pictogram question “Of the items below, which are not used by a person with diabetes (pictures are of lancets/lancet holder, syringes, glucometer testing strips and vacutainers)” resulted a significance of .0.01.
Discussion of Findings
Inability to detect diabetes emergencies in drivers can increase complications and mortality. With increasing epidemic proportion of diabetes, complication prevention and management are essential. Hill, Rybar, Stowe and Jahns (2016) found LEO’s pre-training confidence perceptions in ability to identify disorientation and impairment were high (67%); however, the post-training questionnaire indicated their ability to recognize medical impairments was increased by at least 50%. As in this research, they concluded an improvement in knowledge and the need to incorporate training and screening to assist in identifying and managing medically impaired drivers. This study focused on use of field tool to assist in screening and identification of diabetes emergency symptoms, similar to their TREDS tool helped identify medically impaired drivers. [62] concluded officers were able to correctly
identify overdose symptoms and administer Naloxone “without adverse events or outcomes” and “police officers are receptive to training” and intervention [62]. This study used the officer’s ability to detect diabetes emergencies symptoms in comparison to [62] participants identifying overdose symptoms.
Engelman and Deardorff (2016) found significant differences in knowledge based pre and posttest scores and self-efficacy perception in training first responders on domestic violence of the deaf. Perhaps in the most similar comparison to this study, it was found statistical significance from pre-knowledge to post-knowledge of the officers. Though self-efficacy perception was not addressed in this study, it was determined officers that either were diagnosed
with diabetes or knew others with diabetes did not score higher on pretest overall but all participants had a significant knowledge gain from pretest to posttest. Sixty percent (60%, n=34) of participants had family members who have diabetes, while 3.6% (n=2) had been diagnosed with diabetes. Mean pretest scores were 76.29%. There was no statistical significance noted when correlating pretest scores with prior diabetes training (p=0.253), participant diagnosis of diabetes (p=0.544) or having family members with diabetes (p=0.539). When correlating posttest scoring with prior diabetes training, there was no statistical significance (p=0.109). There was no direct relationship noted between posttest scores and a diagnosis of diabetes (p=0.246).
Correlations between posttest scoring and having family members with diabetes revealed a statistical significance (p= .036) however. Wolf-Fordham, [63-70] found of 28 participants, 36% completed the research study there was a “very large effect for knowledge gain” correlating to 1.4 and 2.3 overall gain. Of the participants included in this study, it was concluded the training yielded a significant knowledge gain consistent with the Wolf Fordham, Twyman and Hamad’s research findings.
Conclusion
In summary of the findings in this study, there was compelling evidence of statistical significance of overall improvement of knowledge in both categories of knowledge base and treatment of diabetes emergencies. The participants included state law enforcement officers in different districts of the state. A one-hour training session was initiated after pretest administration. Once training concluded, a posttest was issued to the participants. Upon data analysis, it was determined overall pretest to posttest scores showed significant improvement in knowledge gain. Specific questions that yielding highest gain of knowledge included diabetes meaning, lack of insulin, hypoglycemia definition, ability to recognize signs and symptoms of hypoglycemia, diabetes cure, complications, legal implications, and treatment of hypoglycemia and identification of diabetes supplies [71-75].
Nursing and Advanced Practice Implications
Diabetes occurs as epidemic proportions in this country. While the population continues to age, more diabetes will be diagnosed if dietary and lifestyle changes are not made. Of great importance is education on lifestyle and dietary modifications in prevention and treatment of diabetes. The nurse’s and Advanced Practice Nurse’s role are to aid in treatment and prevention and deter future complication of the person with diabetes. In the case of a driver with diabetes, if the officers are not aware of the problem and mistake it for intoxication, the patient may present to the emergency department later due to field sobriety testing than a patient presenting with diabetes emergency of their own recognizance or a caregiver who alerts emergency medical response. Patients presenting to the emergency department with impaired level of consciousness undergo numerous tests to determine the cause [76,77].
This may ultimately delay much needed emergency treatment and increases the facility’s manpower, costs and mortality risk of the patient. Nurses should address any case of cognitive impairment as an emergent crisis until ruled out. Upon discharge, the nurse should educate the patient on hypoglycemia while driving, hypoglycemia unawareness and notification of department of transportation by utilizing a wallet carrying card alerting first responders to
driver’s diabetes.
In an office setting, Advanced Practice Nurses (APNs) may encounter these drivers for follow up after outpatient or inpatient treatment. It is imperative for APNs to stress the importance of maintaining stable blood sugars to people with diabetes, especially drivers. Upon follow up from outpatient or inpatient treatment, APNs will be tasked to adjust medication and other treatment regimens to stabilize the patient’s blood sugar levels. APNs should closely follow an abnormality of glucose findings and adjust treatment regimens as indicated. They should provide diabetes education to those drivers suggesting blood sugar testing prior to driving. If low, they should delay driving until after treatment restores blood sugar to a normal level. Drivers should carry fast acting form of sugar with them, as well as a maintenance form of sugar to use when blood sugar drops below normal to prevent impairment while driving.
Future Considerations
The sample size was small. For future research a larger sample size would provide a better assessment of the distribution of knowledge and ability to treat diabetes emergencies. Questions that offered no statistically significant data were treatment for insulin shock, cause of diabetes, definition of hyperglycemia, and when to alert the emergency response system. Therefore, it would be beneficial to review the questions pertaining to these deviations and consider reformulating for better wording or comprehension. It would also be beneficial to focus on these questions in future training sessions and emphasize the difference between hypoglycemia and hyperglycemia definitions and treatment. In these training sessions, there was limited information discussed about treatment of either. Therefore, there should be an emphasis placed on treatment in the future. It was also found that alerting the emergency response system yielded no statistical difference. This is imperative to emphasize in future research. Officers lacking the ability to recognize when to notify emergency response can result in a delay of medical care and increase overall mortality. Future research is warranted to promote an understanding of drivers with diabetes, identify complications that can occur and varying forms of treatment dependent upon the complication. Ability to have and use glucometers in the field may promote screening of diabetes in drivers. Consideration should be given to annual training and retraining officers on diabetes emergencies if score is less than 75%. Considerations should be given to legislative efforts to promote mandatory diabetes and diabetes emergency training of law enforcement and first responders in Mississippi and other states lacking mandatory training.
Funding
This project was funded solely by the primary researcher. Acknowledgements are granted to the Delta State University Robert E. Smith School of Nursing for the use of printing materials for the project and presentation of research at the Mississippi Nurses Association (MNA) state convention.
Feasibility/Sustainability
The sustainability of this project could be enhanced by stakeholders valuing the education and results of the research. Plans to continue this research beyond this scholarly project are in process. Consideration is given to an online platform delivering the same educational information provided in the traditional face to face sessions. Florida recently instituted this platform in 2014. An online platform increases the ability to transcend the normal borders of the communities and expand the territory statewide. The stakeholders would have to “buy in” to needing annual or biannual training on diabetes to sustain this project. Lobbying legislation for mandatory training would also increase the sustainability of the project.
Team
The team of researchers include the primary researcher, Dr. Shelby Polk (research chair), and the DNP Scholarly Project Advisory consisting of Dr. Addie Herrod and Dr. Elizabeth Julyn Overstreet who have contributed endless hours editing and advising promoting project success. In the future, the primary researcher will continue the research producing reliable and valid recommendations based on the available evidence.
External team members included mentors who contributed time discussing the proposed project, curriculum, and setting of trainings. Acknowledgements to mentors Sarah Fech-Baughman, of the American Diabetes Association, and Ronnie Shive, Public Affairs Officer of the Mississippi Highway Patrol Troop D.
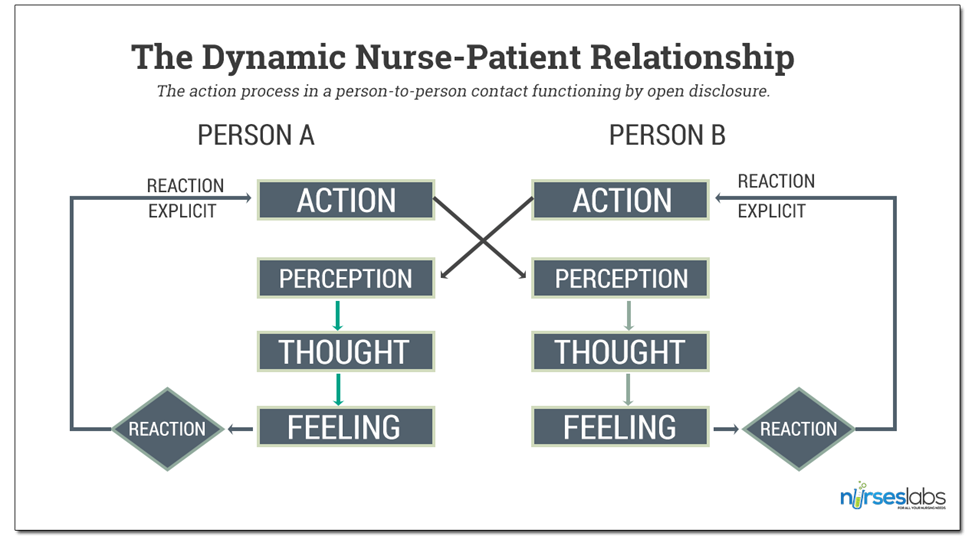
Figure 1: The Dynamic Nurse-Patient Relationship Model from Nurses Labs (Wayne, 2014).
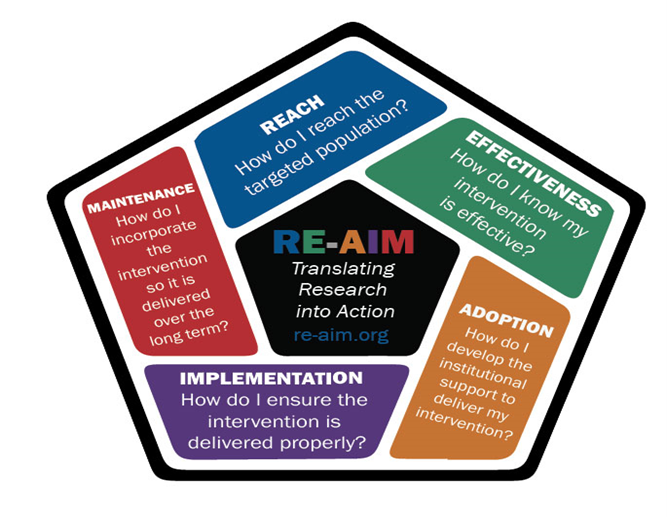
Figure 2: RE-AIM Translation Model (Cummings Online Resources, 2017).

Citation: Smith BG and Smith RE (2020) Training Law Enforcement to Identify and Treat Diabetes Emergencies. Aus J Nursing Res AJNR-100020