Annals of Medical & Surgical Case Reports
(ISSN: 2652-4414)
Image Article
Esophageal Melanocytosis
Ping Huang1,2, Meng-Ting Li1,2, Wei Liu*1,2
1Institute of Digestive Disease, China Three Gorges University, Yichang, China
2Department of Gastroenterology, Yichang Central People’s Hospital, Yichang, China
*Corresponding Author: Wei Liu, Institute of Digestive Disease, China Three Gorges University, 8 Daxue Road, Yichang 443000, China
Citation: Huang P, Li MT, Liu W (2020) Esophageal Melanocytosis. Ann Med & Surg Case Rep: AMSCR-100082
Received date: 12 December 2020; Accepted date: 23 December 2020; Published date: 29 December 2020
A 57-year-old man with a past history of gastroesophageal reflux disease and alcohol and tobacco use underwent an elective gastroscopy as part of the workup for mild epigastric pain. He referred intermittent epigastric pain for the past 3 weeks, along with heartburn and regurgitation. He denied other symptoms with no medication history. Gastroscopy showed two darkly pigmented patches of 3 mm in the proximal esophagus (Figure 1A) as well as an erosive esophagitis (Los Angeles Classification Grade B). Pathological examinationrevealed deposition of a dark brown pigment in the basal layerwhich stained positive for FontanaMasson. The immunohistochemistry staining for melanocytesverified the presence of rare small melanocytes without atypia that was consistent with the manifestation of esophageal melanocytosis. Esophageal melanocytosis,manifested by hyperpigmented lesions with uncertain etiology and pathogenesis, is a rare and benign entity characterized by increased quantity of melanin and melanocytic proliferation in the basal layer of the esophageal squamous epithelium [1, 2]. It has been related to some chronic stimuli whichcause damage of the esophageal mucosa including gastroesophageal reflux disease and alcohol and tobacco use [3, 4]. Meanwhile, it has been considered to be the precursor lesion of primary esophageal melanoma but with no proven firm link [5, 6]. There are insufficient data to establish guidelines regarding management because of its infrequency. Most importantly, gastroenterologists should pay attention to this condition owing to its potential association with primary esophageal melanoma.
Acknowledgements
Funding: This work was supported by National Natural Science Foundation of China (31600134).
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this “Images in Clinical Medicine”.
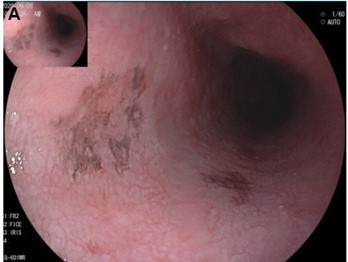
Figure 1: Esophageal Melanocytosis. (A) Endoscopic view of two darkly pigmented patches in the proximal esophagus.
Citation: Huang P, Li MT, Liu W (2020) Esophageal Melanocytosis. Ann Med & Surg Case Rep: AMSCR-100082