Annals of Medical & Surgical Case Reports
(ISSN: 2652-4414)
Image Article
Pancreas Divisum with Acute Recurrent Pancreatitis
Meng-You Zeng1,2, Rong Du1,2, Wei Liu*1,2
1Institute of Digestive Disease, China Three Gorges University, Yichang, China
2Department of Gastroenterology, Yichang Central People’s Hospital, Yichang, China
*Corresponding Author: Wei Liu, Institute of Digestive Disease, China Three Gorges University, 8 Daxue Road, Yichang 443000, China
Citation: Zeng MY, Du R, Liu W (2020) Pancreas Divisum with Acute Recurrent Pancreatitis. Ann Med & Surg Case Rep: AM- SCR-100088
Received date: 12 December 2020; Accepted date: 23 December 2020; Published date: 29 December 2020
A 59-year-old woman presented to the emergency department with a 1-day history of abdominal pain and vomiting. Her past medical history was of an acute recurrent pancreatitis (ARP) of 7 years’ duration. She denied alcohol abuse, greasy food and overeating. Physical examination revealed normal vital signs and mild left upper quadrant abdominal tenderness with normal bowel sounds. Her temperature was 36.5°C, her pulse 75 beats per minute, and her blood pressure 125/75 mm Hg. Laboratory test revealed an elevated serum amylase level of 597 IU/L (normal range, 35 to 135). Computed tomography of the abdomenconfirmed diffuse swelling of the body and tail of pancreas (Figure A). Considering the ill-defined ARP in this patient, magnetic resonance cholangiopancreatography (MRCP) was assessed and confirmed pancreas divisum (Figure B). Pancreas divisum (PD) was considered to be the most plausible explanation, but the differential diagnosis of the ARP also consisted of biliary, alcoholic and hyperlipidemic pancreatitis. Gastroscopy revealed normal appearance of duodenal papilla.A diagnosis of PD with ARPwas made. PDis the most common congenital variant of the pancreatic ductal system [1, 2] and a potential cause of ARP [3-6]. Secretin augmented MRCP is the non-invasive imaging modality of choice for diagnosis of PD [7]. Endoscopic Retrograde Cholangiopancreatography (ERCP) with minor papilla endotherapy and sphincterotomy is considered to be the current first line of therapy [8-10]. After a well-informed discussion of options for interventions with the patient’s family, the decision was made not to pursue ERCP. She was charged home with clinical symptomatic relief.
Acknowledgements
Funding: This work was supported by National Natural Science Foundation of China (31600134).
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this “Images in Clinical Medicine”.
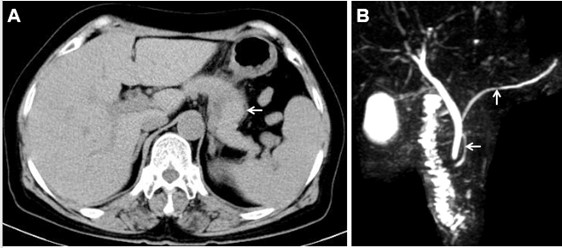
Figure 1: Pancreas divisum with acute recurrent pancreatitis. (A) Axial CT image of diffuse swelling of the body and tail of pancreas (arrow); (B) pancreas divisum by magnetic resonance cholangiopancreatography (vertical arrow represents main pancreatic duct, left arrow represents accessory pancreatic duct)
Citation: Zeng MY, Du R, Liu W (2020) Pancreas Divisum with Acute Recurrent Pancreatitis. Ann Med & Surg Case Rep: AM- SCR-100088