Annals of Medical & Surgical Case Reports
(ISSN: 2652-4414)
Image Article
Gastric Phytobezoar
Ping Huang1,2, Li-Min Zheng1,2, Wei Liu*1,2
1Institute of Digestive Disease, China Three Gorges University, Yichang, China
2Department of Gastroenterology, Yichang Central People’s Hospital, Yichang, China
*Corresponding Author: Wei Liu, Institute of Digestive Disease, China Three Gorges University, 8 Daxue Road, Yichang 443000, China
Citation: Huang P, Zheng LM, Liu W (2020) Gastric Phytobezoar. Ann Med & Surg Case Rep: AMSCR-100083
Received date: 12 December 2020; Accepted date: 23 December 2020; Published date: 29 December 2020
A 72-year-old man presented to the emergency department with a 2-week history of epigastric pain and melena. Physical examination revealed normal vital signs and mild epigastric tenderness. Computed tomography (CT) of the abdomenrevealedround nodular shadow in stomach (Figure A). Considering the ill-defined and strange CT findings in this patient, gastroscopy was initially assessed and confirmed a 10-cm-diameter gastric phytobezoar with necrotic pressure ulcer of the angulus (Figure B, C). A diagnosis of gastric phytobezoar was made.Further questioning of the patient found that he had eaten dried persimmons. Gastricphytobezoars are likely to be formed after ingestion of dried persimmons, which usually cause ulcerative lesions in the stomach and subsequent bleeding [1]. The currently available treatment options for a gastric phytobezoar include dissolution of the phytobezoar by Coca-Cola and removal by endoscopic devices [2, 3]. Oral administration of Coca-Cola is often performed in an attempt to soften the phytobezoar because endoscopic fragmentation with biopsy forceps is a big challenge due to the hard consistency [4]. In this patient, we fragmentized the phytobezoar into smaller pieces with the help of Coca-Cola lavages. Finally, endoscopic fragmentation and removal were successful. The patient was then discharged home with a 2-month course of rabeprazole 10 mg twice daily administered for peptic ulcer. Follow-up endoscopy at 3 months revealed the absolute disappearance of any residual fibers and the ulcer healed.
Acknowledgements
Funding: This work was supported by National Natural Science Foundation of China (31600134).
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this “Images in Clinical Medicine”.
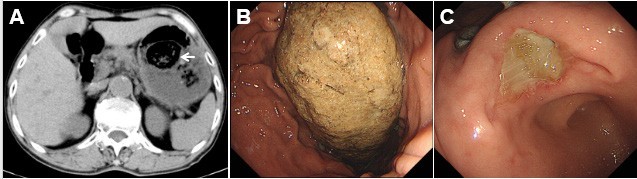
Figure 1: Gastric phytobezoar. (A) Axial CT image of round nodular shadow in stomach (arrow); (B) endoscopic view of an indigestible mass of 10 cm diameter in the lesser curvature; (C) pressure ulcer caused by gastric phytobezoar
Citation: Huang P, Zheng LM, Liu W (2020) Gastric Phytobezoar. Ann Med & Surg Case Rep: AMSCR-100083