Journal of Surgery and Insights
ISSN 2652-4643
Review Article
An Algorithm for the Management of Patients with Upper Limb Spasticity
Gill P1*, Henry A1, Hassan Z1,2 and McArthur P1,2
1 Department of Burns and Plastic Surgery, Whiston Hospital, Mersey, United Kingdom
2 Department of Burns and Plastic Surgery, Alder Hey Children’s Hospital, Liverpool, United Kingdom
*Corresponding author: Gill P, Department of Burns and Plastic Surgery, Whiston Hospital, Warrington Road, Prescot, L35 5DR, United Kingdom, Tel: (0044)-151-426-1600; Fax: (0044)- 151-430-1855; Email: Parneet.gill@sthk.nhs.uk
Citation: Gill P, Henry A, Hassan Z, McArthur P (2020) An Algorithm for the Management of Patients with Upper Limb Spasticity. J Surg Insights: JSI-100029
Received date: 15 October, 2020; Accepted date: 20 October, 2020; Published date: 27 October, 2020
Abstract
Background: Patients with upper limb spasticity are often treated using a range of conservative measures, including physiotherapy, splinting, serial casting and botulinum toxin. Surgical options may be offered once conservative measures are no longer successful, including tendon transfers/lengthening, selective neurectomy or carpectomy and fusion. There are no published recommendations for the stepwise management using these modalities.
Objective: We propose an algorithm to streamline the management of upper limb spasticity within a multidisciplinary team (MDT) setting.
Methods: We have used case studies to illustrate the process and its application into clinical practice.
Results: The algorithm follows the patient journey from initial diagnosis, to referral to a specialist MDT for assessment using history and examination, followed by differentiation into groups depending on status of tone/fixed contracture. We have illustrated the use of the algorithm in 3 cases.
Conclusion: We propose a clinically relevant algorithm for the management of patients with upper limb spasticity.
Keywords: Algorithm; Botulinum toxin; multidisciplinary team; Upper limb spasticity
Introduction
Upper limb spasticity may be congenital or acquired. It often presents in the paediatric population as a result of cerebral palsy and in the adult population following acute traumatic brain injury, spinal cord injury or stroke [1].
Spasticity was traditionally defined as a disorder of the motor unit resulting in velocity-dependent increase in muscle tone, due to the hyperexcitability of the stretch reflex [2]. More recently it has been described as an upper motor neuron lesion, producing disordered sensory-motor control via involuntary activation of muscles [3]. The delicate equilibrium of the extensors, flexors, abductors and adductor muscles of the hand and the extensors, flexors, pronators and supinator’s of the arm ensures good function of the upper limb [4]. Spasticity of specific muscle groups or imbalance of forces around a joint lead to reduced range of motion [5].
Algorithm
We propose an algorithm (Figure 1) to streamline the management of patients with upper limb spasticity from initial diagnosis to definitive treatment.
Following initial diagnosis of upper limb spasticity at the presenting unit, the patient is referred to a specialist MDT where a formal assessment can be carried out. It is important to identify the individual functional aims of each patient and whether affected muscle groups display increased tone, a fixed contracture or are on the continuum within a combination group.
If increased tone is present, we suggest management with botulinum toxin (BTX-A) as first-line treatment, with consideration of splinting, lycra garments or selective neurectomy. If a fixed contracture is present, we suggest management with serial casting if appropriate, but primarily surgical intervention should be considered with tendon lengthening/transfers or carpectomy and fusion.
If the patient falls into the combination group, where increased tone is developing into a reversible contracture or a fixed contracture, management can be tailored by following the algorithm. It is important to reassess the patient following intervention and continue management as proposed by the algorithm.
Results
Patient A (Figure 2) is a 65-year-old female with a history of cerebral palsy and right sided spastic hemiparesis. She was referred to the specialist MDT for full assessment. She has a history of angina, osteoarthritis, hypertension and left sided carpal tunnel syndrome. Clinical examination revealed mild spasticity in right wrist flexors, moderate spasticity in right lumbricals/interossei and mild spasticity in right long flexors. She was noted to have tight metacarpal joints (MCPJ) and painful hyperextension of the proximal interphalangeal joints (PIPJ). Her functional aims were to achieve good bilateral upper limb function, specifically she wanted to be able to shake hands in a social setting.
She was placed in the increased tone group and underwent BTX-A treatment to flexor carpi radialis (FCR), pronator teres (PT), flexor digitorum profundus (FDP) and intrinsics in conjunction with use of splintage to increase MCPJ extension and FDP stretch. Upon reassessment, she developed an intrinsic minus position, which was treated with a lower dose of BTX-A. This significantly improved her right upper limb function and enabled her to shake hands in social settings. Regular reassessment is ongoing, with 6-monthly maintenance doses of BTX-A maintaining a good range of motion.
Patient B (Figure 3) is an 18-year-old male with a traumatic brain injury following a road traffic collision at the age of 2 years old resulting in left upper limb spasticity. He was referred to the specialist MDT. He was fit and well, with not significant prior medical history. Examination revealed a fixed contracture to the left upper limb. His functional aims were to develop bilateral upper limb function.
He was placed in the fixed contracture group and underwent a tendon transfer using palmaris longus (PL) and FCR to extensor carpi radialis brevis/extensor carpi radialis longus (ECRB/ECRL) and extensor carpi ulnaris (ECU), with release of pronator quadratus (PQ), release of flexor digitorum superficialis (FDS) and capsulotomy of the wrist. He is maintaining good range of motion upon regular reassessment.
Patient C (Figure 4) is a 21-year-old male with a traumatic brain injury following a road traffic collision causing spastic quadriplegia. He was referred to the specialist MDT. He was fit and well with no significant prior medical history. Examination revealed mild PIPJ contractures affecting the right upper limb. A strong association reaction affected the left upper limb, with increased tone at the left elbow, extreme wrist extension, MCPJ fixed flexion contractures, lumbrical tightness and FDP/FDS increased tone. His functional aims were to mobilize with bilateral upper limb function for activities of daily living but specifically weight bearing.
He was placed in the combination group and underwent treatment with BTX-A to left biceps, brachialis, wrist extensors, FDS and lumbricals. This was followed by step lengthening of the left wrist extensors, release of MCPJ volar plates and check rein ligaments and fractional lengthening of FDP. Follow up was performed with static splinting, followed by dynamic splinting and intensive physiotherapy. He is maintaining a good range of motion upon regular reassessment.
Conclusion
Neurologists, paediatricians, therapists and hand surgeons undertake the management of paediatric and adult upper limb spasticity. The range of treatment modalities offered range from conservative, pharmacological to surgical interventions. There are no published gold standard guidelines available in the literature to date. We propose an algorithm to streamline the assessment and management of patients with upper limb spasticity, within a specialist MDT. This aims to offer patients the full range of treatment in a timely manner, in order to achieve the best possible outcome.
Discussion
Classical presentation of paediatric patients with spastic cerebral palsy may include adduction/internal rotation of the shoulder, flexion of the elbow, flexion/pronation of the wrist, flexed finger posture and thumb-in-palm position.
Upper limb spasticity in the adult population can occur following a stroke or an acute traumatic brain injury. Long-term sequelae include difficulty in maintenance of personal hygiene, pain, deformity and the development of contractures [6].
Spasticity of the extrinsic flexors of the wrist (FCR and FCU), digits (FDS and FDP) or thumb (flexor pollicis longus [FPL]) commonly causes deformity at the wrist and digits. A thumb in palm position is usually caused by additional adductor pollicis and 1st dorsal interossei involvement. Although primarily muscular in origin, other factors may also play a role in causing the contracture, including skin deficiency, capsular contracture or neurovascular shortening [7]. These should be considered when assessing the patient.
Alterations in position at rest can result in difficulties with maintenance of hygiene, reduced functional range of movement and can result in wounds from nails digging into the palm. The function of the hand may be affected as actions such as grasping, release and pinch may be near impossible to perform. Although appearance is often placed at the bottom of the priority list in patients with upper limb pathology, it is an important aspect of the patient’s self image and thus should not be forgotten or underestimated.
Bilateral upper limb and lower limb involvement should be noted whilst performing a general inspection of the patient. The posture of the wrist, digits and thumb should be inspected at rest. Assessment of the quality of the skin and presence of any wound or maceration should be performed. Abnormal position of the digits, such as a swan neck deformity should be highlighted, specifically if it is static or dynamic.
Palpation of the volar wrist crease, digital creases and palmar thumb crease enables assessment of skin laxity. Any obvious tight bands at the FCR or FCU should be identified.
The patient should be asked to grasp an object whilst palpating the FCR and the FCU sequentially. Under normal circumstances, activation of finger flexors causes the wrist flexors to relax, however in patients with increased spasticity, the FCR or FCU may also contract. The passive and active range of motion should be measured using a goniometer. The wrist angle that the digits go to, from a starting extended position into a flexed position, is called the Volkmann’s angle. The larger the Volkmann’s angle, the more severe the deformity.
Evaluation of the wrist deformity is done in conjunction with the finger deformity and can be classified using the Zancolli classification [8]. Three groups are described based on the degree of spasticity. An alternative classification system looks at the thumb in palm deformity [9], also describing the severity of each.
Radiographs are useful to highlight joint damage, remodeling or arthropathy. The wrist joint may display loss of proximal carpal row height, whereas articular head changes or joint space narrowing may be noted in the presence of swan neck deformities. These aids accurate diagnosis following clinical examination.
Conservative management begins with regular physiotherapy to stretch the muscles affected, with a view to improve the range of motion at joints. The exercises demonstrated by the hand physiotherapists are reproduced on a daily basis by careers or the rehabilitation team. These are supplemented by splintage to maintain adequate position of the upper limb. Incremental increases in range of motion can be achieved by serial casting, however this requires a compliant patient for success.
BTX-A is a popular treatment choice in patients with spasticity without fixed flexion deformities. It works by blocking the release of presynaptic acetylcholine at the neuromuscular junction, resulting in chemo denervation of the injected muscle [10]. This action is irreversible; however, new nerve roots grow into the denervated muscle, enabling contraction and therefore the blockage is rendered temporary. Practically this means that the patient will require regular treatments with BTX-A in order to maintain improved range of motion.
Indications for surgery include impairment in hygiene, breakdown in palmar skin or restriction in pinch, grasp and release [11]. There is no formal cut-off for degrees of deformity before surgery may be considered, although generally conservative measures are considered first [4]. A relative contraindication to surgical intervention is athetosis, with fluctuations in spasticity.
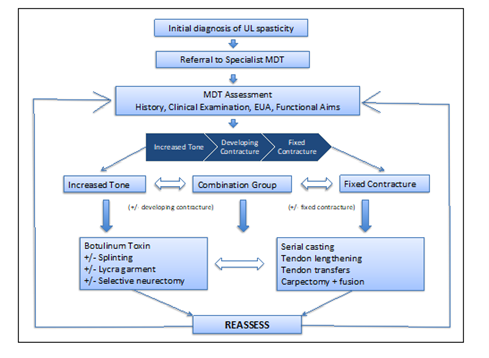
Figure 1: Algorithm for the management of patients with upper limb spasticity.
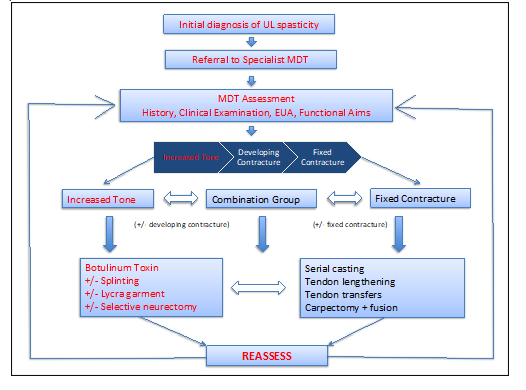
Figure 2: Algorithm for the management of patient with increased tone.
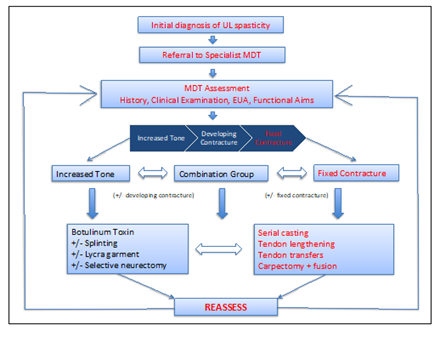
Figure 3: Algorithm for the management of patient with fixed contracture.
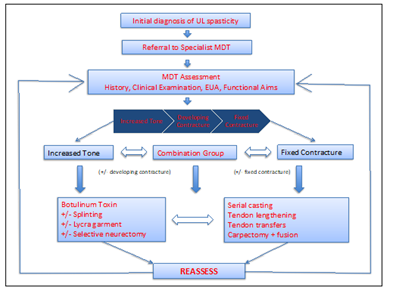
Figure 4: Algorithm for the management of patient with increased tone and fixed contracture.
Citation: Gill P, Henry A, Hassan Z, McArthur P (2020) An Algorithm for the Management of Patients with Upper Limb Spasticity. J Surg Insights: JSI-100029