Emergency Medicine and Trauma Care Journal
ISSN 2652-4422
Case Report
Awake Prone Positioning during Weaning from Invasive Mechanical Ventilation in COVID-19 Pneumonia-Is it Possible? Description of a Case Series
Del Castillo-Gordillo C1,2*, Mora-Valdes R2, Appiani-Florit F1, Van Grieken-Garcia J1,2, Castillo-Veliz J1, Silvio-Salazar S1, Rojas-Gallegos F1, Cereño-Fuentes C1, Potthoff-Navarrete P1, Yañez-Vidal F2, Luque-Gonzalez M 2 and Begazo-Gonzales A1
1Cononary unit, cardiovascular centre, DIPRECA Hospital. Santiago, Chile
2Coronary unit, cardiovascular centre, San Borja Arriaran Hospital Hospital, Chile
*Corresponding author: César Del Castillo Gordillo MD, Cardiologist, Cardiovascular center, DIPRECA Hospital. 1200 Vital Apoquindo, 7601003, Santiago, Chile
Citation: Del Castillo-Gordillo C, Mora-Valdes R, Appiani-Florit F, Van Grieken-Garcia J, Castillo-Veliz J, et al. (2020) Awake Prone Positioning during Weaning from Invasive Mechanical Ventilation in COVID-19 Pneumonia-Is it Possible? Description of a Case Series. Emerg Med Trauma. EMTCJ-100054
Received date: 03 December, 2020; Accepted date: 08 December, 2020; Published date: 15 December, 2020
Abstract
We present three cases of patients connected to IMV due to COVID-19 pneumonia. Case 1: A 37-year-old man was withdrawn from IMV at 12 days of evolution, subsequently tolerated intermittent awake prone over the next three days, for 2, 18, and 4 hours, respectively. Case 2: A 33-year-old man was withdrawn from IMV after 7 days of evolution, subsequently tolerated intermittent awake prone on the third and fourth day, for 18 hours and 11 hours, respectively. Case 3: A 44-year-old man was withdrawn from IMV at 10 days of evolution, subsequently tolerated the awake prone on the first and third day, for 2 hours and 4 hours, respectively. There were no associated complications. Limitations in prone were due to patient intolerance and delirium. There were no significant changes in either oxygenation or ventilatory mechanics while they were in the prone position. None of the patients required re-intubation. They were transferred to less complex units.
Keywords: COVID-19; Prone position; Ventilator weaning
Abbreviations
COVID-19 : Coronavirus disease 2019
IMV : Invasive mechanical ventilation
Introduction
Awake prone, in conjunction with oxygen therapy, has been instituted in the emergency department and critical care areas as a highly effective measure to treat patients, and to some extent, avoid invasive mechanical ventilation (IMV).
Prone is a proven therapy in the management of moderate-to-severe acute respiratory distress syndrome under IMV [1]. Its operation is mainly based on the idea that by improving the ventilation-to-perfusion ratio, the prone could decrease the physiological dead space. This would decrease the effort involved in respiration. Given the current pandemic, during the year 2020, different publications have reported the use of the prone in non-intubated patients with COVID-19 and respiratory failure, associated with various types of supplemental oxygen administration [2-5].
All of these studies report a significant improvement in oxygenation, associated with a decrease in respiratory rate and ventilatory work [2-5]. The most remarkable result of these studies is that only 26% of patients required intubation, and mortality did not exceed 11% [4,5]. However, like any technique, adverse effects have been reported, the main one being poor tolerance to this position.
Despite these studies on awake prone to avoid connection to IMV, there are no studies on the use of this position to consolidate IMV weaning, which is why we describe a series of cases where this technique was applied.
Case presentation
We present 3 cases in which we used the awake prone after IMV disconnection. All the patients were hospitalized in a cardiovascular critical care unit between May and June 2020.
Case 1: A 37-year-old man with no contributive medical history, hospitalized for severe pneumonia caused by COVID-19, with severe respiratory failure, poor response to oxygen therapy and awake prone, and was therefore connected to IMV. The thoracic CT scan revealed extensive areas of ground-glass opacities, predominantly subpleural and basal, with condensation at both lung bases. Protective mechanical ventilation, deep sedation, and neuromuscular blockade, associated with two periods of prone position lasting 72 hours and 12 hours were performed. Complete empirical antibiotics were administered for 7 days, and the patient did not receive corticosteroids. There were no dysfunctions of other systems or proven co-infections. The patient showed a good clinical response, with intermittent hyperactive delirium managed with quetiapine plus dexmedetomidine, and finally, IMV was withdrawn after 12 days of intubation. He tolerated the prone position for 2 hours on the first day, for 18 hours on the second day, and for 2 hours on the third day. The prone position is affected by back pain. For its adaptation, it requires support with dexmedetomidine, quetiapine, and clonazepam. It is desirable that ventilatory mechanics and oxygen requirements remain stable both in the supine and prone positions (Figure 1). There were no associated complications during the changes in position. Finally, the patient left the unit five days after extubation.
Case 2: A 33-year-old man with a history of grade 2 obesity, hospitalized for severe pneumonia due to COVID-19, with an increasing need for oxygen therapy, significant respiratory effort, and poor response to prone vigil, for which he was connected to IMV equipment. Thoracic CT scan revealed extensive bilateral ground-glass opacities in all lung lobes, associated with poor alveolar filling. Protective mechanical ventilation and deep sedation were performed. Complete empirical antibiotics were administered for 7 days, and he did not receive corticosteroids initially. There were neither dysfunctions of other systems nor proven co-infections. The patient demonstrated a good clinical response, with intermittent hyperactive delirium managed with quetiapine plus dexmedetomidine, and finally, IMV was withdrawn after 7 days of intubation. He presented mild laryngeal stridor, with a favorable response to corticosteroids (dexamethasone 4 mg) and nebulization with racemic adrenaline. During the first and second days, he did not tolerate the prone position due to back pain and delirium. He remained prone for 18 hours on the third day and 11 hours on the fourth day. He required support with quetiapine and clonazepam for adaptation. Ventilatory mechanics and stable oxygen requirements are desirable in both supine and prone positions (Figure 2). There were no associated complications during changes in position. Finally, the patient left the unit five days after extubation.
Case 3: A 44-year-old man with a history of high blood pressure and type 2 diabetes mellitus, was hospitalized for severe pneumonia due to COVID-19, with an increasing need for conventional oxygen therapy, significant respiratory effort, and a poor response to awake prone, for which he was connected to IMV equipment. No chest CT was performed on admission due to his clinical instability. Microbiological study revealed co-infection with Streptococcus Pneumoniae. Protective mechanical ventilation, deep sedation, neuromuscular blockade, 3 doses of methylprednisolone (125 mg/day), and antibiotic therapy with ampicillin/sulbactam were performed. On day 8 of evolution, he presented tracheobronchitis due to carbapenemase-producing Klebsiella pneumoniae, so the antibiotics were changed to colistin and meropenem. The patient demonstrated a good clinical response, with intermittent hyperactive delirium managed with quetiapine plus dexmedetomidine, and IMV was finally withdrawn after 10 days of intubation. During the first day, he tolerated awake prone for 2 hours. However, he could not maintain this position on the second day due to delirium. On the third day, he maintained the position for 4 hours. He was initially supported with a high-flow nasal cannula and required support with dexmedetomidine, quetiapine, and clonazepam for adaptation. Ventilatory mechanics and stable oxygen requirements are desirable in both supine and prone positions (Figure 3). There were no associated complications during changes in position. Finally, the patient left the unit five days after extubation.
Conclusion
We presented 3 cases of relatively young men with severe COVID-19 pneumonia and the need for IMV, who cooperated to varying degrees with the change of position to prone during the weaning period and maintained clinical stability during this period. Furthermore, there were no significant complications during the prone period, although this period could not be longer, mainly due to poor position tolerance and delirium.
The clinical course allowed for consolidating IMV weaning and discharge from the intensive care unit. However, as described, there was no clinical impact on the improvement of lung mechanics or oxygenation, as described in the published series. We attribute the latter to the fact that the evolutionary process of the disease is different from that reported in the published evidence.
Our case series shows neutral results of the application of the vigil prone during weaning. This can be assessed in future studies. It is also a complement to what has been published on prone vigil during this pandemic.
Footnote
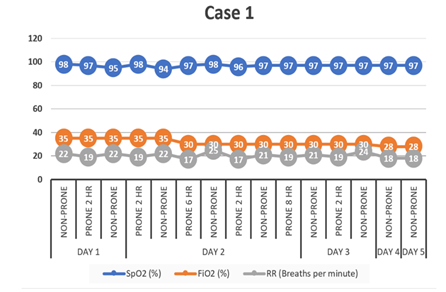
Figure 1. Case 1: Temporal evolution with awake prone during IMV weaning. SpO2: Saturation of peripheraloxygen (%). FiO2: Fraction of inspired oxygen (%). RR: Respiratory rate (breaths per minute).
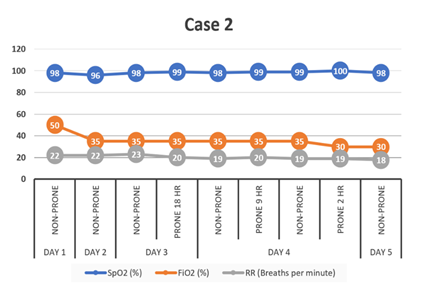
Figure 2. Case 2: Temporal evolution with awake prone during IMV weaning. SpO2: Saturation of peripheral oxygen (%). FiO2: Fraction of inspired oxygen (%). RR: Respiratory rate (breaths per minute).
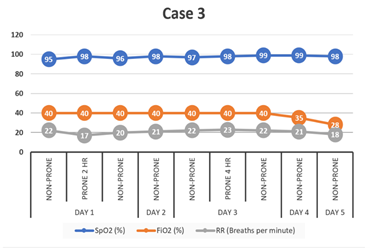
Figure 3. Case 3: Temporal evolution with awake prone during IMV weaning. SpO2: Saturation of peripheral oxygen (%). FiO2: Fraction of inspired oxygen (%). RR: Respiratory rate (breaths per minute).
Citation: Del Castillo-Gordillo C, Mora-Valdes R, Appiani-Florit F, Van Grieken-Garcia J, Castillo-Veliz J, et al. (2020) Awake Prone Positioning during Weaning from Invasive Mechanical Ventilation in COVID-19 Pneumonia-Is it Possible? Description of a Case Series. Emerg Med Trauma. EMTCJ-100054