Annals of Medical & Surgical Case Reports
ISSN 2652-4414
Case Report
Metastatic Renal Neuroectodermal Tumor about a Case and Review of the Literature
Erraichi H(1), Randriamanovontsoa NE(1) , Litique V (1), El ouai Y(1) ,Oualla K(2),Ammadour L(2), Benbrahim Z(2), Mellas N(2) and Limacher JM(1)
*Corresponding author: Hayat ERRAICHI, I, Medical Oncology Service, CHU hassan II fes, Morocco
Citation: Errachi H, Randriamanovontsoa NE, Litique V, Oualla K, Ammadour L, et al. (2020) Metastatic Renal Neuroectodermal Tumor about a Case and Review of the Literature. Ann Med & Surg Case Rep: AMSCR-100075
Received date: 28 November, 2020; Accepted date: 07 December, 2020; Published date: 10 December, 2020
Abstract
Primary renal neuroectodermal tumor (PNET) is a very rare disease; often diagnosed at a late stage due to their non-specific clinical presentations. Diagnosis is based on histology, immunohistochemistry and molecular biology. Once PNET is diagnosed, multimodal treatment is indicated. Despite all the treatment options, the prognosis for people with metastatic disease is poor. We report the case of a 40-year-old female patient with metastatic renal Ewing's sarcoma from the outset who was treated with palliative chemotherapy such as vincristine, Doxorubicin, cyclophosphamide with a good initial response.
Keywords: Histology; Palliative chemotherapy; Primary renal neuroectodermal tumor
Introduction
Renal PNETs are exceptional malignant tumors, and highly aggressive, which are seen mainly in young adults, urinary signs clinically manifest them at locally advanced and metastatic stages, which explains their late diagnosis and poor prognosis. Due to the rarity of this disease, there is no consensus regarding the treatment of renal Ewing's sarcoma / PNET. We report the case of a young patient with metastatic renal Ewing's sarcoma who was treated with chemotherapy. Diagnosis is based on histology, immunohistochemistry, and molecular pathological findings. Once PNET is diagnosed, multimodal treatment IS indicated. Despite all the treatment options, the prognosis for people with metastatic disease is poor.
Presentation of the case
A 40-year-old young woman followed for hip dysplasia, surgically treated strabismus who has presented headaches, left ptosis and then binocular diplopia since September 2019, the brain scan revealed a sphenoidal tumor mass syndrome with involvement of the cavernous sinus. Brain and spinal cord MRI showed diffuse metastatic bone damage with lumbosacral epiduritis, right frontotemporal meningeal metastasis with extension to the right temporal soft tissue, invasion of the sella turcica and sphenoid sinus (Figure 1). TAP CT showed a tumor renal heterogeneous calcified metastatic pulmonary, mediastinal and bone level (Figure 2).
An endoscopic biopsy of the sphenoidal mass via the endonasal route was carried out, the anatomopathological study of which returned in favor of a secondary localization of an Ewing sarcoma The biopsy of the renal mass also revealed an Ewing sarcoma / a primary neuroectodermal tumor With absence of labeling by anti cytokeratin AE1 / AE3, Anti chromogranin A, Anti synaptophysin, CD56, PS100, CK19, CK5 / 6 antibodies, KI 67 High on the immunohistochemical study the diagnosis was confirmed by molecular biology with PCR detection of the fusion transcript EWS-FLI1 t11-22.
The patient received palliative multidrug therapy based on cyclophosphamide 1.2g / m2 J1, doxorubicin 60 mg / m2 J1 and vincristine 1.5mg / m2 J1, J1 = J21. We observed a very noticeable improvement in his general condition after the 1st treatment and partial radiological response after the first 3 courses (Figure 3), given this excellent clinical and radiological response, we agreed to continue up to 6 courses, but the patient presented with grade IV medullotoxicity, hence the weekly switch between vinblastine and cyclophosphamide by the oral route.
Discussion
Primary renal PNET is most commonly a disease of relatively younger patients. The average age at diagnosis is only 30.4 years and more than half of new cases diagnosed are seen in men [1,2]. The clinical expression of renal PNETs is not pathognomonic. The diagnostic time is relatively short, testifying to his aggressiveness. Urinary signs such as low back pain, nephretic colic, palpable mass are their main manifestations, hematuria and deterioration of the general condition reflect an advanced stage of the disease and sign a poor prognosis. The x-ray workup should include computed tomography imaging, which often shows a mass syndrome with areas of necrosis or bleeding. On MRI, the tumor is in hyper signal in the T1 and T2 sequences [3].
Our patient underwent a thoraco-abdominopelvic CT which showed an enormous retroperitoneal solid-cystic mass, heterogeneously enhanced, from the left kidney, measuring 98mm long axis. Abdomino-pelvic MRI was not performed in our patient. The diagnosis of renal PNET is based on the pathological examination. Macroscopically the tumor is rounded, oval or multi-nodular, well defined, without encapsulation. When cut, it is gray-beige or yellow and its consistency is soft or crumbly. Necrotic or hemorrhagic changes are frequent. Calcifications are sometimes observed [4]. Histology finds a malignant proliferation, lobular architecture, pseudo-alveolar, consisting of small round or oval cells, monomorphic appearance and poorly differentiated immunohistochemistry and molecular studies are necessary to diagnose the family of sarcoma tumors of 'Ewing (ESFT), as they help to differentiate ews from other tumors with histologic resemblance, such as Wilms tumor, neuroblastoma, rhabdomyosarcoma and lymphoma [5-7]. Cytogenetics have an important role to play in confirming the diagnosis, by screening for the t (11; 22) (q24; q12) translocation resulting in the production of the EWS / Friend leukemia virus integration 1 (FLI-1) fusion [8,9] (Figure 4).
There is no consensus on the treatment of metastatic renal PNET due to its rarity. The treatment is extrapolated from the treatment for Ewing's sarcoma of bone. It is based on a combination of chemotherapy comprising active drugs such as doxorubicin (A), vincristine (V), cyclophosphamide (C). Our patient received 4 cures of VAC / IE which allowed locoregional and remote control after 4 cures but with poor clinical and haematological tolerance, hence the switch to weekly vinblastine -cyclophosphamide by the oral route.
Ewing's sarcoma and PNET present an aggressive course characterized by early metastatic disease (25–50% at the time of presentation) and are considered systemic disease [11]. In addition to local lymph node involvement, renal PNET often metastasizes to the lung, liver, and bone [5, 12].
Conclusion
Renal-located PNETs should be considered in renal tumors of all ages, but especially in children and young adults. Despite aggressive treatment, the prognosis for patients with metastatic disease is poor. One of the main challenges is proper diagnosis and adequate treatment within an accelerated period.
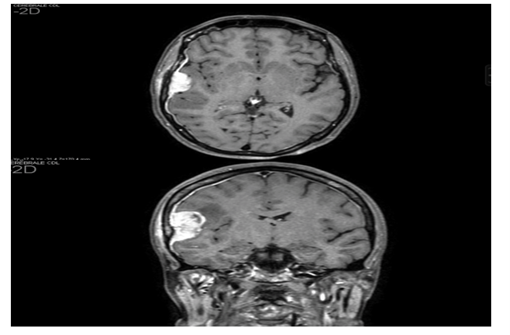
Figure 1: Right frontotemporal meningeal metastasis with extension to the right temporal soft parts, invasion of the turcics it and the sphenoid sinus.
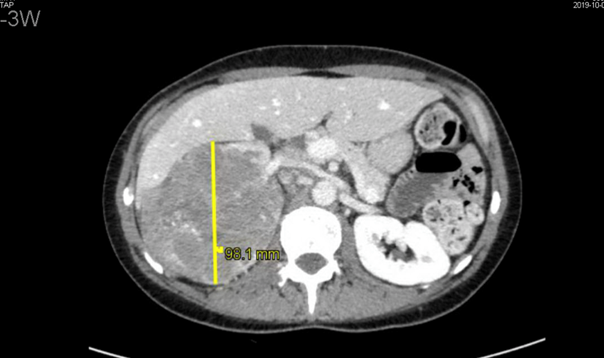
Figure 2: Abdominopelvic CT scan; there is a huge retro-peritoneal solid-cystic mass, heterogeneously enhanced, coming from the left kidney, measuring 98mm long axis.

Figure 3: Abdominopelvic CT scan; Hypodense tissue mass in the middle third of the right kidney, measuring 45mm versus 98mm Long axis.
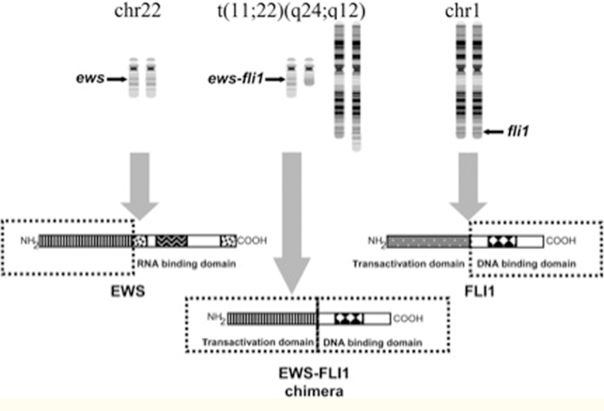
Figure 4: Reciprocal translocation of chromosomes 11 and 22 t (11; 22) which leads to the formation of an EWS-FLI1 fusion gene (Adapted with permission from Bernstein et al. [10]
Citation: Errachi H, Randriamanovontsoa NE, Litique V, Oualla K, Ammadour L, et al. (2020) Metastatic Renal Neuroectodermal Tumor about a Case and Review of the Literature. Ann Med & Surg Case Rep: AMSCR-100075