Journal of Urology and Renal Problems
(ISSN 2652-4805)
Research Article
Do we really need to place any tubes after PCNL? The Era of Stubeless (stent+tube less) PCNL
Yelikar A*
Medical trust hospital, kochi, kerala, India
*Corresponding author: Aditya Yelikar, Medical trust hospital, kochi, kerala, India
Citation: Yelikar A (2020) Do we really need to place any tubes after PCNL? The Era of Stubeless (stent+tube less) PCNL. J Urol Ren Probl: JURP-100009
Received date: 29 July, 2020; Accepted date: 11 August, 2020; Published date: 17 August, 2020
Abstract
Introduction: PCNL has now become the standard minimally invasive treatment for renal stones≥1.5cm. Many modifications came forward to reduce the drawbacks of placement of a PCN like prolonged hospital stay, pain, fever. One such modification was tubeless PCNL (placement of only a double J stent & no PCN).We offer totally tubeless PCNL to a selectedgroup of patients (wherein no PCN or double J stent is placed). We have termed tubeless PCNL as Stubeless PCNL where Stubeless word is a combination of two words-stent + Tube.We compared standard, tubeless &Stubeless PCNL in terms of stone free rate, hospital stay, pain score, surgery duration & complications in patients undergoing renal stone surgery (PCNL) at our centre.
Methods: A randomised controlled study was done including patients undergoing PCNL for renal stones by standard or tubeless or totally tubeless technique.we compared the 3 techniques in terms of stone free rate, surgery time, Haemoglobinchange,creatinine change andcomplications.
Results: 28% ,6% & 5% of the cases in the standard, tubeless and totally tubeless groups had complications.There was significant difference in the mean percentage increase of the serum creatinine post operatively, which was highest in the totally tubeless group (6.8%) & least in the tubeless group (0.7%). There was significant difference in the percentage drop of haemoglobin between the groups, which was highest in standard (7.4%) & least in the tubeless group (5%).
Conclusion: Tubeless & totally tubeless PCNL are good alternatives to standard PCNL with less complications and comparable outcomes.
Keywords: PCNL-Percutaneous nephrolithotripsy; PCN-Percutaneous nephrostomy;Stubeless (totally tubeless) PCNL
Introduction
PCNL has now become the standard minimally invasive treatment for renal stones ≥1.5cm after its first introduction in 1976 by [1]. Placement of a percutaneous nephrostomy tube at the end of procedure is an integral part of the standard technique. PCN helps in hemostasisby tamponade, drainage of the pelvicalyceal system & helps to maintain the tract in case of a second re-look procedure.Fear of complications (bleeding, leakage, collections, and prolonged hospital stay) was the reason for this well-establishedpolicy.An early trial omitting placement of a PCN led to significant complications and made urologists very adherent to this policy [2]. Many modifications came forward to reduce the drawbacks of placement of a PCN like prolonged hospital stay, pain, fever [3,4]. One such modification was tubeless pcnl (placement of only a double J stent & no PCN). However, the ureteral stents can cause irritative voiding symptoms, for example dysuria andpollakuria, and removal of the stent at a later timeresults in additional morbidity for the patient. For thisreason, we offeredStubeless PCNL to a selectedgroup of patients (wherein no PCN or double J stent is placed).Stubeless PCNL was first described by [5].We compared standard, tubeless &Stubeless PCNL in patients undergoing renal stone surgery (PCNL)at our centre.
Materials & Methods
We used a randomized trial study design, after receivingthe approval from the ethical committee. Informed consent was obtained from all eligible patients atthe time of admission. Then patients underwent PCNL for renal stones. The inclusion criteria wererenal stones of size ≥1.5 cm,extracorporeal shockwave lithotripsy (SWL) failure or stone in closed calyx and diverticulum. The exclusion criteria were more than two Percutaneous accesses, cases with prior diversion of the upper urinary tract (nephrostomy tube or double J stent), significant perforation of thecollecting system, ureteralobstruction in addition to renal anomaly. By using exclusioncriteria, 45 patients were excluded from the study.All procedures were performed by one expert endo-urologist.All PCNL were done in prone position.One or two accesses were created under fluoroscopicguidance using air or contrast medium to delineate pelvicalyceal system.
Weused Bull’s eye technique to createaccess. We used a 18G needle to enter the calyces. Then a guidewire was placed, andwe performed dilation and placed an Amplatz sheath. Thetract was dilated using Alken’sdilators. The stone was disintegratedby ballistic lithotripsy and then extracted. Aftercompletion of stone removal, a double J stent and nephrostomy tube was placed in group 1 (standard), in group 2 (tubeless) only a double J stent was placed, whereas in group 3 (Stubeless) neither a nephrostomy tube nor a double J stent was placed.The nephrostomy tube was removed after 24 hours,Foley’s catheter was removed after 48 hours and double J stent after10 days. A study by was considered as a reference study for sample size [6,7].
The randomization allocation was done by using random number generator, and allocation concealment was done by sequentially numbered opaque sealed envelope which was opened at the end of stone removal.Hemodynamically stable patients and those whose painwas controllable with oral paracetamol medications wereconsidered for hospital discharge after 48 hours. Before discharge renalultrasonograpy and X-ray KUB was done to rule out urinoma or any residual stones.In addition, 1 month later, they were asked telephonically about return to normal activity. Then, the three groups werecompared with regard to the operative time, preoperative and post operative haemoglobin values, preoperative and post operative creatinine values, transfusion rate, postoperative pain score and analgesics requirement, complications, duration of hospital stay and stone free rate.The data were gathered and analyzed by Student t test andchi-square test. P value <0.05 was considered to indicate statistical significance(Table A-F).
There was significant difference in the mean percentage increase of the serum creatinine post operatively, which was highest in the totally tubeless group (6.8%) & least in the tubeless group (0.7%).
There was no significant difference in the mean pain score between the groups. There was significant difference in the mean surgery time between standard vs tubeless/totally tubeless, but there was no significant difference in the mean surgery time between tubeless & totally tubeless.
There was significant difference in post operative temporary urinary leakage between standard vs tubeless/totally tubeless, but there was no significant difference in post operative temporary urinary leakage between tubeless & totally tubeless.
Results
There was significant difference in the mean surgery time between standard vs tubeless/totally tubeless, but there was no significant difference in the mean surgery time between tubeless & Stubeless. There was significant difference in the mean percentage increase of the serum creatinine post operatively, which was highest in the totally tubeless group (6.8%) & least in the tubeless group (0.7%). There was significant difference in the percentage drop of haemoglobin between the groups, which was highest in standard (7.4%) & least in the tubeless group (5%).28%, 6% and5% of the cases in the standard, tubeless andStubeless group had complications.
Discussion
The objective of the PCNL operation is to cure patients with renal and upper ureteral stones with minimal morbidity and hospital stay. In early days tubeless PCNL was thought to have several limitations and was restricted to highly selected cases [6,7]first described “tubeless” PCNL which involved placement of a ureteric stent without nephrostomy [8]. In recent reports, most of these limitations have been overcome.
Nowadays, tubeless PCNL can be performed with multiple punctures, simultaneously in bilateral disease and even in solitary kidneys [9]. A nephrostomy may be effective in controlling parietal&parenchymableeding, whereas it is not effective in controlling bleeding from a arterial source which may need angio-embolization. Randomized studies showed no significant clinical advantages of using tissue sealants or coagulation of bleeding points to minimize urinary extravasation and bleeding [10, 11].Goh and Wolf proposed “almost totally tubeless” PCNL wherein an externalized ureteric catheter was retained for 1-2 days and they concluded that PCNL without nephrostomy is effective, safe, and reduced the morbidity [6].In some reports only sub costal punctures can be left tubeless [12] while for others tubeless supracostal punctures are advantageous in terms of reduction of length of hospital stay and pain [13,14]. In our study there was no significantdifference for tubeless PCNL between supra costal & infra costal punctures.Regarding operative time, no significant differences were found between the tubeless group and the standard group[15]. In another study there was significant difference in the operative time between the Stubeless group and standard group favouring Stubeless group[16,17]. In a similar study the mean operation time in the standard PCNL group (53.37±5.54 min) was significantly higher than in the totally tubeless PCNL group (50.32±3.83mins)[18].
In our study there was significant difference in the mean surgery time between standard vs tubeless or Stubeless (34.6+/-10.4mins Vs 29.1+/-7.3mins or 30.3+/-5 mins), but there was no significant difference in the mean surgery time between tubeless & totally tubeless. Surgery time was more in the standard group due to the additional time needed to place the double J stent and nephrostomy tube.Bleeding is a major complication after PCNL requiring transfusion. Studies show a transfusion rate of 3 -12% post PCNL [19-21]. Some studies show no significant difference exists for the need of blood transfusion between the groups [15]. Another study showed a transfusion rate of 10% & 20% in standard & totally tubeless groups [18,22].
In our study the need for transfusion was maximum in the standard group (4%) and least in the totally tubeless group (2%). However severe intraoperative bleeding requiring to abandon the procedure was encountered in 2 cases in the standard group.In our study 1 case had peri-renalhematoma in the standard group which was managed conservatively with no need of transfusion[23] reported that renal parenchymal thickness in access line is more significantly correlated with duration of urinary leakage than grade of hydronephrosis. In our study we did not find any significant correlation of the parenchymal thickness with complications.Studies have shown that in tubeless PCNL group there is significant reduction in postoperative pain and analgesic requirement as compared to standard PCNL or even small tube group [18,22,24,25].In our study there was no significant difference in the pain score and analgesic requirements between the groups. Studies show that there is no significant difference in post operative fever between the groups [15,22]. Another study showed higher incidence of post operative fever in cases with a nephrostomy [26]. In our study there was no significant difference in post operative fever between the standard, tubeless andStubeless PCNL groups.In a study by [27] there was no significant difference in the serum parameters between tubeless & Stubeless. Another study showed that the mean Haemoglobin drop in the standard &Stubeless group were 1.51±1.89 mg/dL and 2.27±3.88 mg/dL which was not significant [18]. Whereas in our study there was significant difference in the creatinine change between standard vs tubeless vsStubeless groups (2.8% vs 0.7% vs 6.8%). Also there was significant difference in the mean haemoglobin drop in the standard vs tubeless vsStubeless groups (7.4% vs 5% vs 6%).
A study of Stubeless PCNL showed 100% stone free rate[28]. A meta analysis of standard and tubeless PCNL showed no significant difference in the stone free rate between the groups [29]. The global CROES study showed a stone free rate of 75.7% [30]. Similarly, in our study the stone free rate for Stubeless PCNL was 100%. Whereas stone free rate in the standard and tubeless groups was 96% and 98% [31] reported that tubeless PCNL was effective and insertion of a ureteric catheter was sufficient for drainage and the complication rate was 9.9%. Another study [24] reported more frequent complications in the standard PCNL method in comparison with the tubeless technique.The meta analysis [29] showed no significant difference in complications between standard and tubeless groups. In our study there was significant difference in the complication rate among the groups which was 28% in the standard group, 6% in the tubeless group and 5% in the Stubeless group[25] compared tubeless and standard PNL and showed that tubeless procedure reduces postoperative urinary leakage. The problem of urine leak post PCNL varied from 0 to 11.1% with reduced urine leak in tubeless groups as compared to standardgroup [29]. In our study there was significant difference in post operative temporary urinary leakage which was 12%, 3% and 4% in standard, tubeless and Stubeless groups.
Studies report reduced hospital stay in tubeless PCNL group compared with groups with either a small or a big nephrostomy tube[15,17,22,24,32].Another series of Stubeless PCNL reported a mean hospitalstay of 2.8 days[5].In contrast, two years after this study, Winfield and colleagues showed that Stubeless PCNL prolongs hospital stay with an increase in complication rates [6]. In contrastanother study showed the mean hospitalization time was significantly lower in the Stubeless PCNL group (1.25±0.49 days) than in the standard PCNL group (2.95±1.17 days) [18]. In our study the mean hospital staysin standard, tubeless & Stubeless groups was 51.84+/-13.52 hours, 48.88+/-3.37 hours & 48.88+/-3.37 hours with no significant difference. The onlyabsolute contraindications for PCNL are uncorrected coagulopathy[33]and an untreated urinary infection. Even for special indications like children, obesepatients or large stone burden on both sides, a tubelessprocedure seems to be feasible with reduced postoperativemorbidity [14,34].
Althoughthere is currently no consensus on the need for postoperativerenal drainage after PCNL, the published data suggest thetubeless procedure as the method of choice when the surgeons account for six criteria [16]: (1) less than two accesstracts, (2) no significant perforation of the collecting system (3) no need for a second-look procedure, (4) no significantintraoperative bleeding, (5) an uncomplicated procedure,and (6) no intrathoracic violation.
The possible limitation of the tubeless procedure is that it precludes secondary procedures for the treatment of residual stones. However, alternatively, residual calculi can be safely managed by ESWL or retrograde intracranial surgery by use of flexible ureter scope.With the intent of reducing postoperative discomfort and pain, hospital stay, and cost, the Stubeless PNL procedure has gained popularity in recent years. Appropriate patients should be selected for totally tubeless PNL. We believe that this procedure will be acceptable only when safety has not been sacrificed. We believe that uncomplicated percutaneous nephrolithotomy can be performed without leaving a nephrostomy tube or ureteral stent. We also believe that the major advantage for patients undergoing totally tubeless PNL is avoiding a additional procedure of stent removal, absence of stent-related flank pain and dysuria.
Conclusion
Tubeless & totally tubeless (stubeless) PCNL techniques have equally good stone clearance with less complications and less post op temporary urinary leakage as compared to standard PCNL. Tubeless &Stubeless PCNL had significantly less surgery time as compared to standard PCNL.
|
Mean age(years) |
38.15+/-13.84 |
|
Mean BMI(kg/m2) |
21.87+/-2.11 |
|
Sex (male) n (%) |
461 (69.3%) |
|
Laterality |
|
|
Left |
329 (49.5%) |
|
Right |
336 (50.5%) |
|
Mean kidney size (cm) |
|
|
Length |
9.97+/-1.38 |
|
Width |
4.93+/-0.79 |
|
Previous history of stone surgery |
|
|
1)Yes |
38 |
|
2) No |
627 |
|
Mean stone size (mm) |
20.7+/-4.94 |
|
Mean stone enhancement(HU) |
1208.33+/-318.06 |
|
Mean stone surface area (mm2) |
319.59+/-238.36 |
|
Mean Guy’s stone score |
1.56+/-0.82 |
|
Mean access time (seconds) |
38.98+/-17.11 |
|
Mean fluoroscopy time (seconds) |
228.2+/-28.58 |
|
Mean total surgery time (mins) |
32.94+/-9.73 |
|
Mean tract size (Fr) |
21.67+/-1.52 |
|
No. Of tracts |
|
|
1) One |
276 (92%) |
|
2)Two |
21 (7%) |
|
3) Three |
3 (1%) |
|
Access |
|
|
1) Supra costal |
174 (58%) |
|
2)Infra costal |
126 (42%) |
|
Mean pre op Hb(mg/dl) |
12.13 |
|
Mean post op Hb(mg/dl) |
11.41 |
|
Mean % drop in Hb |
5.94% |
|
Mean pre op creat |
1.04 |
|
Mean post op creat |
1.05 |
|
% change in creat |
0.83% |
|
Mean pain score |
3.65+/-1.22 |
|
Mean hospital stay(hours) |
51.25+/-10.17 |
Table A:Patient Demographics (mean +/- SD).
|
Mean stone size (mm) |
Mean stone surface area (mm) |
Mean Guy’s stone score |
|
Standard |
20.59+/-4.4 |
317.19+/-221.78 |
|
Tubeless |
19.05+/-4.61 |
236.18+/-204.43 |
|
Totally tubeless |
18.87+/-3.7 |
233.32+/-127.63 |
|
p value |
0.83 |
0.77 |
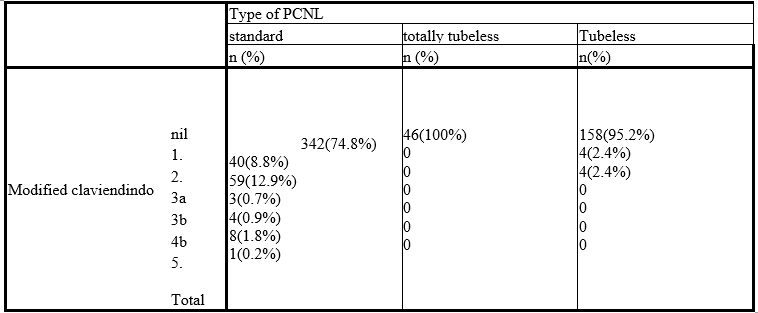
Table B:Comparing preoperative parameters across the groups.
|
- |
Pre-op Hb (mg/dl) |
Post-op Hb (mg/dl) |
P value |
Percentage Change in Hb |
||||
|
Mean |
Standard Deviation |
Mean |
Standard Deviation |
Mean |
Standard Deviation |
|||
|
Type of PCNL |
Standard |
12.1 |
1.1 |
11.3 |
1.2 |
<0.001* |
-7.4 |
5.7 |
|
Tubeless |
12.2 |
1.1 |
11.7 |
1.2 |
<0.001* |
-5.0 |
4.1 |
|
|
Totally Tubeless |
12.5 |
1.0 |
11.8 |
.8 |
<0.001* |
-6.0 |
3.4 |
|
|
|
P value |
0.041* |
<0.001* |
|
<0.001* |
|||
Table C: Comparison of mean Hb changes.
|
- |
Pain Score |
Surgery time(mins) |
|||
|
Mean |
Standard Deviation |
Mean |
Standard Deviation |
||
|
Tubeless |
Standard |
3.7 |
1.3 |
34.6 |
10.4 |
|
Tubeless |
3.5 |
1.1 |
29.1 |
7.3 |
|
|
Totally Tubeless |
3.4 |
1.0 |
30.3 |
5.0 |
|
|
|
P value |
0.207 |
<0.001* |
||
Table D:Comparison of pain score and surgery time.
|
- |
Mean hospital stay+/-SD (hours) |
Mean tract size +/- SD (Fr) |
Stone free rate |
Blood transfusion |
Urinary leakage |
|
Standard (n=100) |
51.84+/-13.52 |
21.72+/-1.6 |
96% |
4% |
12% |
|
Tubeless |
48.48+/-3.37 |
21.72+/-1.11 |
98% |
3% |
3% |
|
Totally tubeless |
48.48+/-3.37 |
21.32+/-1.11 |
100% |
2% |
4% |
|
p value |
0.23 |
0.034 |
0.07 |
0.81 |
0.001 |
Table E:Comparison of post-operative outcomes.
|
Modified clavien Dindo score |
Standard (n=100) |
Tubeless (n=100) |
Totally tubeless (n=100) |
p value |
|
Nil |
72 (72%) |
94 (94%) |
100 (100%) |
|
|
1 -Transient elevation of serum creatinine -post op fever |
9(9%) |
3 (3%) |
2 (2%) |
- |
|
2 -temporary urinary leak -UTI |
13 (13%) |
3 (3%) |
3 (3%) |
- |
|
3a -Perirenal hematoma |
1 (1%) |
0 |
0 |
- |
|
3b -Severe intra op bleeding |
2 (2%) |
0 |
0 |
- |
|
4b -urosepsis |
2(2%) |
0 |
0 |
- |
|
5 -Death |
1 (1%) |
0 |
0 |
- |
|
Total no. Of complications
|
28 (28%) |
6 (6%) |
5 (5%) |
0.001 |
|
Note:*One patient may have more than one complications 28% ,6% and 5% of the cases in the standard, tubeless & totally tubeless group had complications. |
||||
Table F:Comparison on complications by Modified Clavien system.
Citation: Yelikar A (2020) Do we really need to place any tubes after PCNL? The Era of Stubeless (stent+tube less) PCNL. J Urol Ren Probl: JURP-100009