Journal of Surgery and Insights
(ISSN 2652-4643)
Research Article
Perioperative "Light Sedation" with Dexmedetomidine in Brachial Plexus Block During Shoulder Arthroscopic Surgery: A Case Series
Belmonte R, Cusano M, Abate C, Santo F, Di Lorenzo B, Manlio I and De Lipsis L*
Department of Anesthesia, “Sacred Heart of Jesus” Hospital, Benevento, Italy
*Corresponding author: Luca De Lipsis, Department of Anesthesia, “Sacred Heart of Jesus” Hospital, Benevento, Italy, E-mail: codelip@libero.it
Citation: Belmonte R, Cusano M, Abate C, Santo F, Di Lorenzo B, et al. (2020) Perioperative "Light Sedation" with Dexmedetomidine in Brachial Plexus Block During Shoulder Arthroscopic Surgery: A Case Series. J Surg Insights: JSI-100026
Received date: 10 August, 2020; Accepted date: 14 August, 2020; Published date: 19 August, 2020
Abstract
Interscalene brachial plexus block is a topical anesthetic technique indicated for the anesthesia/analgesia of the shoulder and of the proximal portion of the arm, used in the block of sympathetic nerves, in reconstructive surgery of the upper limb, in algodystrophic syndrome, in neoplastic chronic pain and/or in postoperative care.
Keywords: Anesthetic technique; Arthroscopic Surgery; Reconstructive surgery
Abbreviations
ASA : American Society of Anesthesiologists
ASM : Anterior scalene muscle
CAM-ICU : Confusion Assessment Method for the Intensive Care Unit
ENS : Electrical Nerve Stimulation
MSM : scalene muscle
RASS : Richmond Agitation-Sedation Scale
VAS : Visual Analogue Scale
Introduction
The “single-shot” technique is frequently used in the surgery of the shoulder; the length of the sensory and motor block depends on the anesthetic drug. The extension of the length of the sensory block with ropivacaine is suggested for a better management of postoperative pain, as well as to reduce the administration of opioids or nonsteroidal anti-inflammatory drugs.
During the surgery, the following must be ensured:
In order to obtain a more rapid onset and a longer duration of local postoperative anesthesia following brachial plexus block, dexamethasone, clonidine, and dexmedetomidine are administrated as add on therapy [2].Dexmedetomidine is an α2-adrenoceptor agonist with sedative, anxiolytic and analgesic properties, which plays a key role in intraoperative "light sedation" during topical procedures [3].
Light sedation corresponds to 0 and -2 in the Richmond Agitation-Sedation Scale (RASS); it is widely used because it guarantees optimal analgesia and minimum sedation [4]. The aim of this study is to evaluate the impact of IV administration of dexmedetomidine in shoulder arthroscopic surgery with interscalene brachial plexus block on sedation, hemodynamics, postoperative analgesia and postoperative delirium.
Materials and Methods
After obtaining their informed consent, 30 patients (age range: 30-60; ASAI e II) were recruited for elective shoulder arthroscopic surgery in rotator cuff injury using topical anesthesia with interscalene brachial plexus block. The following patients were excluded: those for whom the block was not indicated (due to coagulopathies, local infection, allergy to local anesthetic agent), and ASA III and IV patients. Technique: after monitoring vital signs and following IV administration of 0.05 mg/kg of midazolam, fentanyl 50 mcg and 0.02 mg/kg of atropine, patients were placed in a supine position, with the head turned by 45 degrees, towards the non-surgical side. USguided block was performed with ENS (Electrical Nerve Stimulation), initial amperage of 0.5 mA, with high frequency linear probe, set between 12 and 18 Mhz. After skin disinfection, the sterile probe was set on the neck in a horizontal position, on the SCM (sternocleidomastoid muscle) at the cricoid cartilage. Once the carotid artery and the external jugular vein in short-axis view were detected, the probe was laterally moved, keeping a perpendicular approach to the skin. The anterior scalene muscle (ASM) and the middle scalene muscle (MSM) were medially and laterally detected, under the SCM end.
The hypoechoic roots of C5, C6 and C7 of the brachial plexus trunks were detected between these two muscles. The 22 G needle, connected to the neurostimulator, was introduced into the target area, 2-3 cm apart, in parallel with the probe axis, in plane, in order to make sure that the needle moved in parallel with the US beam. Once the correct needle position was confirmed by ENS, amperage was reduced under 0.2 mA in order to avoid muscular clonic movements [5]. After the aspiration test, 20 ml of ropivacaine 0.75% were administered under US guidance. 20-30 minutes after the block, patients were moved to the operating room and underwent basic monitoring: continuous oxygen saturation (SpO2) and heart rate, arterial pressure (PA) every 10 minutes. 4 l/m of O2 were administered with nasal cannula and sedation with IV dexmedetomidine was performed with the following protocol [6]:
The surgical procedure began after loading dose. Average surgery time was 60 minutes. Sedation was assessed by RASS; RASS 0/-2 was the target level. At the end of the procedure, 30 mg of IV ketorolac were administered as add-on therapy. Postoperative pain was measured every 6 hours with VAS, over the next 24 hours. Analgesic therapy with IV paracetamol (1 gr, every 6 hours) with IV ketorolac rescue dose if VAS was > 4. Postoperative delirium was assessed by the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) [7].
Results
As indicated in Figure 1,2, heart rate and arterial pressure decreased during the surgical procedures after dexmedetomidine administration in comparison to baseline, with the peak at the fortieth/fiftieth minutes; no bradycardia or hypotension occurred such as to require pharmacological treatment or infusion interruption. Parameters came within normal ranges once the drug was suspended, in the recovery room, as well as RASS Score, that moved from -2 to 0 (Figure 3).
Average sedation was at -1 and -2, with no respiratory failure. SpO2 was always > 95%. Dexmedetomidine had to be suspended in three patients because RASS was -4. Postoperative VAS was significantly low during the first 8 hours. The motor block was activated after 8 hours, when limb motility was restored. VAS average value was <5. Ten patients required IV ketoralac due to VAS > 5 (Figure 4). None of the patients had postoperative delirium.No complications due to interscalene brachial plexus block were reported. Hemodynamic parameters were stable during the postoperative period. None of the patients experienced nausea, vomiting, itching or altered consciousness.
Discussion
The use of dexmedetomidine as add on IV therapy in shoulder arthroscopic surgery with brachial plexus block proved that the drug was well tolerated, fostering a prolonged operative analgesia, with no need of opioids assessed the addition of dexmedetomidine to ropivacaine in supraclavicular brachial plexus block. Both perineural and IV administration of dexmedetomidine led to an earlier onset time and to a prolonged motor and sensory block [8].
In a different study by dexmedetomidine was administered as adjuvant sedation, compared to midazolam, during shoulder surgery with brachial plexus block. The authors reported that dexmedetomidine guaranteed an earlier and prolonged occurrence of sensory and motor block with comparison to the group where midazolam was administered, with no adverse events [9].
The mechanism through which dexmedetomidine mediates IV analgesia is not fully understood. However, such mechanisms might be the same that clonidine has. Both drugs act on presynaptic α2-adrenoceptors by inhibiting the release of norepinephrine in peripheral nociceptors. Clonidine also proved to have local anesthetic effects by inhibiting nerve signal conduction through Aδ and C fibers, and by stimulating the release of enkephalin-like substances from peripheral sites. Finally, clonidine analgesic effect might be mediated via the modulation of the opioid system [10-13]. The infusion of dexmedetomidine causes a reduction of hemodynamic parameters due to the reduction of α2-mediated inotropes, with no significant side effects. This is in line with the results obtained in other studies where dexmedetomidine proved to be a valuable addition in the sedation of patients undergoing upper limb surgery with regional block [15, 16], which also guarantees a reduction of perioperative bleeding [14,15].
Intraoperative sedation plays a key role in relieving anxiety and stress response. Propofol, a common sedative agent, may cause delirium in patients undergoing heart or orthopedic surgery, especially older patients, or patients with mechanical ventilation in ICU. Dexmedetomidine proved to reduce the incidence of delirium, as well as postoperative nausea, vomiting and the use of opioids, which are able to cause it [16].
Conclusion
This study confirms that low dosage IV infusion of dexmedetomidine improves patient comfort, prevents delirium, guarantees bradycardia with hypotension without hemodynamic instability, and reduces the occurrence of postoperative nausea and vomiting. Moreover, dexmedetomidine may affect the onset time, prolong sensitive and motor anesthesia, as well as analgesia in patients undergoing peripheral block.
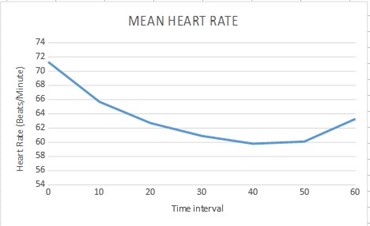
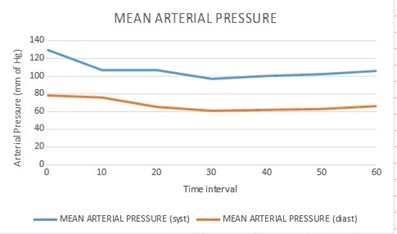
Figure 1,2: Heart rate and arterial pressure decreased during the surgical procedures.
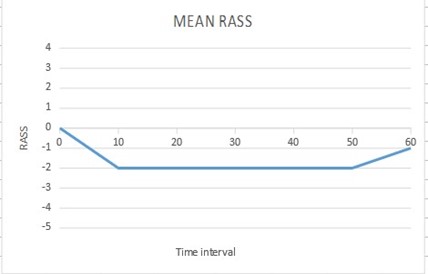
Figure 3:Parameters came within normal ranges once the drug was suspended, in the recovery room, as well as RASS Score, that moved from -2 to 0.
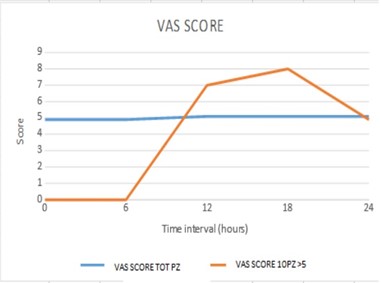
Figure 4:None of the patients had postoperative delirium.
Citation: Belmonte R, Cusano M, Abate C, Santo F, Di Lorenzo B, et al. (2020) Perioperative "Light Sedation" with Dexmedetomidine in Brachial Plexus Block During Shoulder Arthroscopic Surgery: A Case Series. J Surg Insights: JSI-100026