Annals of Medical & Surgical Case Reports
ISSN 2652-4414
Case Report
Cardiovascular Adverse event after the use of Varenicline: A Case Report and Literature Review
Mahida H1*, Gharia B3 and Pinnales D2
1Hackensack meridian Jersey shore University Medical Center, Neptune , NJ, USA
2Interventional Cardiologist, Hackensack meridian Jersey shore university Medical center, Neptune, NJ, USA
3University of Florida, Jacksonville, FL, USA
*Corresponding author: Hetavi Mahida, Hackensack meridian Jersey shore University Medical Center, Neptune , NJ, USA
Citation: Mahida H, Gharia B, Pinnales D (2020) Cardiovascular Adverse event after the use of Varenicline: A Case Report and Literature Review. Ann Med &Surg Case Rep: AMSCR-100071
Received date: 18 July, 2020; Accepted date: 04 August, 2020; Published date: 10 August, 2020
Background
Smoking is one of the most common risk factor for myocardial ischemia [1]. Varenicline is the drug of choice for smoking cessation and has been very effective for patients in abstained from smoking [2]. Though not much common but varenicline has been associated with cardiovascular side effect, and there had been many report about different type of adverse event. A literature review of many meta- analysis study was carried out to look for the adverse cardiovascular event associated with varenicline.
Though over the years, many studies ahs emerge which has shown that varenicline for smoking cessation is better than other medications like bupropion and nicotine patch [3] and so it remains the first line drug of choice for smoking cessation. Many articles are published which has shown the vareniciline has been associated with cardiovascular side effects; one such study showed that the incidence of cardiovascular events was 34% higher in the risk compared with the control interval (relative incidence, 1.34; 95% confidence interval, 1.25-1.44) [4]. Besides this case reports are also published indicating the cardiovascular side effect, one such unique case is presented here.
Case report
A 43-year-old man with the no past medical history except 40 yeas of smoking one pack a day presented to emergency department for severe chest pain. He was in normal sinus rhythm when evaluated by the EMS with ST elevation in the infero- posterior lateral leads (Image1).
He was emergently taken to the catheterization laboratory after been loaded with aspirin, brilinta and 4000 units of heparin. In the Cath a right femoral arterial approach was initiated and he was found to have LAD (Left anterior descending) artery to be large with 50% stenosis in proximal region and 40% in the mid region. Large circumflex with no disease. Right coronary artery (RCA) had 90% stenosis in the mid segment and it bifurcated distally into large PDA(posterior descending artery) and large posterolateral branch. There was a 40% stenotic lesion at the bifurcation.The mid RCA lesion appears to be the culprit(Image 2,3).
Patient got one drug eluting stent to the RCA and was post- catheterization was doing better and was started on beta-blocker, high intensity statin , dual antiplatelet therapy and for smoking cessation was started on varenicline and was discharge home in stable condition with list of medications as aspirin 81 mg tablet 1 tablet oral daily, atorvastatin 80 mg tablet 1 tablet p.m. daily, lisinopril 2.5 mg 1 tablet oral daily, Brilinta 90 mg tablet 1 tab twice a day, metoprolol succinate 25 mgtablet 1 tab oral daily, Nitrostat 0.4 mg tablet 1 tab sublingually q. 5minutes x 3 p.r.n. for chest pain and varenicline 0.5 mg-1 mg .Echocardiogram done post STEMI showed mild regional wall abnormalities and EF of 65%. Patient did had outpatient follow up and was adherent to his regimen and smoking cessation. But after a month of this event, he started to have again for chest pain which was a squeezing substernal discomfort, pressure-like for which he took 4 tablets of baby aspirin.Symptoms persisted for more than half an hour and so came back to emergency department. On admission, he was fund o have elevated troponin of 4.71, all the rest of the laboratory result was normal. Electrocardiogram showed normal sinus rhythm with no ST-T wave changes (Image 3). Due to his worsening pain he was taken urgently for catherization and was found to have the left anterior descending coronary artery had a subtotal occlusion in its proximal portion, a long 90% stenosis (Image 4).
The circumflex has mild luminal wall irregularities. The right coronary was dominant with evidence of a patent stent. He got one drug eluting stent to Left anterior descending artery. Due to rapid development of the symptoms a search was done to find the cause of the acute coronary syndrome. Patient was compliant with the medications as well as with the smoking cessation, and regularly took his medication varenicline. Rare side effects for drugs aspirin, metoprolol succinate, brilinta, Lisinopril and varenicline was search and found that varenicline is associated with myocardial ischemia event.
Discussion
Smoking is one of the main risk factor for coronary artery disease and it one of the most preventable cause of illness in united states[5,6]. Varenicline which is a partial agonist of α4β2 nicotine acetylcholine receptor that competitivelyblocks the receptors and only partially activates it[7]. Many clinical trials have been developed which showed efficacy of varenicline for smoking cessation[8-10]. Analysis of all this study showed that varenicline is better for smoking cessation[8-10].
Varenicline for patients after acute coronary syndrome is all effective. Data form one such study which was multicenter, double blind, randomized to varenicline and placebo for 12 weeks showed that it is efficacious in smoking cessation. However, this study saw the adverse cardiovascular event after 30 days of discontinuation of the varenicline, myocardial infarction was 2% from 151 patients in varenicline group and 151 patients in placebo group (p value 1); while unstable angina was 0.7% (p value 0.21) [2]. In EVITA trial there was 5.3 % in varenicline group(n=151) and 6% in placebo group (n=151)affected with myocardial infarctionand (2.6 % v 4%) affected with unstable angina[11]. Another systemic review and meta-analysis of randomized controlled trial which compare varenicline with placebo for smoking cessation. A total of 57 cardiovascular SAEs occurred in the 7213 patients randomized to varenicline, and 43 occurred in the 5493 patients randomized to placebo but on further pooling of the data no significant difference was found (RR 0.88, 95% CI 0.50-1.52)[12](Image5-7).
Many cases of myocardial infarction and unstable angina has been reported. One such case is where a 48-year-old male after starting varenicline for 22 days presented with NSTEMI and got catheterization with stent placement. Another one include a 62-year male with chest pain on varenicline found to have coronary artery disease with stent placement[13]. There had been many reports on cardiovascular event with varenicline which included arrhythmia and MI [14].
Also search from the FDA online website registry showed that adverse cardiovascular event at 52 weeks was associated with 2% (7 of 353) as compared to placebo group 0.9% (3 of 350) had non-fatal myocardial infarction. And 2.3% (8 of 353) in the varenicline group had a need of coronary revascularization as oppose to 0.9% in the placebo group [15]. A review of the literature showed that a study from 22 trial showed cardiovascular adverse event emergent in 0.63% (34/5431) in varenicline group and 0.47% (18/3801) in the placebo groups. And their risk difference, 0.27% (95% confidence interval-0.10 to 0.63; P=0.15), based on all 22 trials, was neither clinically nor statistically significant [16].
In our case, the patient was admitted for STEMI and was found to have culprit vessel right coronary artery which was treated and at that time his left anterior descending was only 50% occluded. He was then started on varenicline as he was active smoker and since his discharge he was compliant with varenicline and had maintain cessation from smoking. Exactly after a month he comes back reporting symptoms of unstable angina and he was readmitted for non - ST elevation MI and was taken urgently to catheterization and found to have 90% stenosis of the proximal left anterior descending artery which was intervened with a single drug eluting stent. The patient was educated to stop taking the varenicline as our search showed that it can be associated with cardiovascular side effect, though less but reported. And the patient was educated to maintain abstinence from smoking.
Conclusion
Thus, research of all this literature and case report review shows that though there is not statistically significance difference in the events of cardiovascular side effects. There are reported incidence of varenicline leading to cardiovascular side effect, which includes unstable angina/ NSTEMI, arrhythmia etc. So for any patient on varenicline having cardiovascular event, should be evaluated for its adverse event and reported. More awareness need to be created in acknowledging its adverse events.
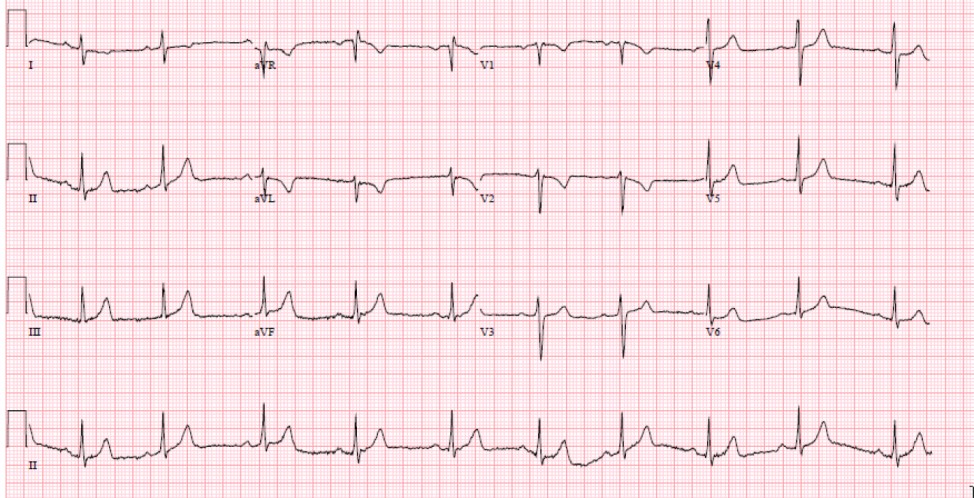
Image 1:EMS with ST elevation in the infero- posterior lateral leads.

Image 2:Large LAD with 50 % stenosis in proximal region, LCX with no obstructive coronary disease.
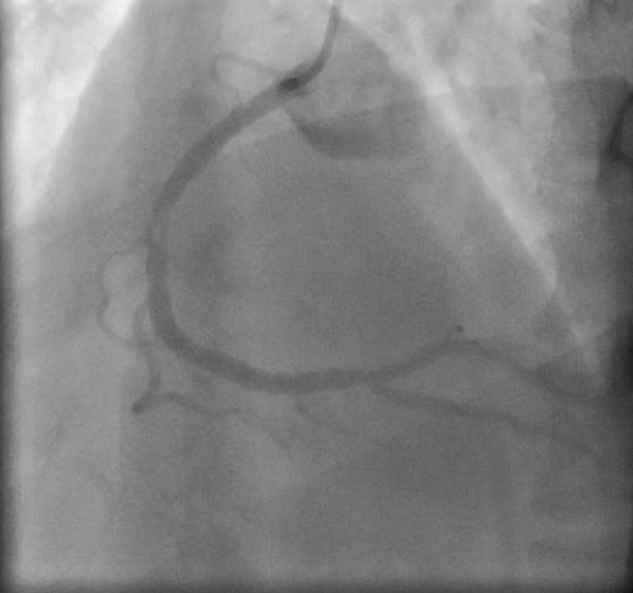
Image 3:RCA with 90 % stenosis that was stented with one DES.
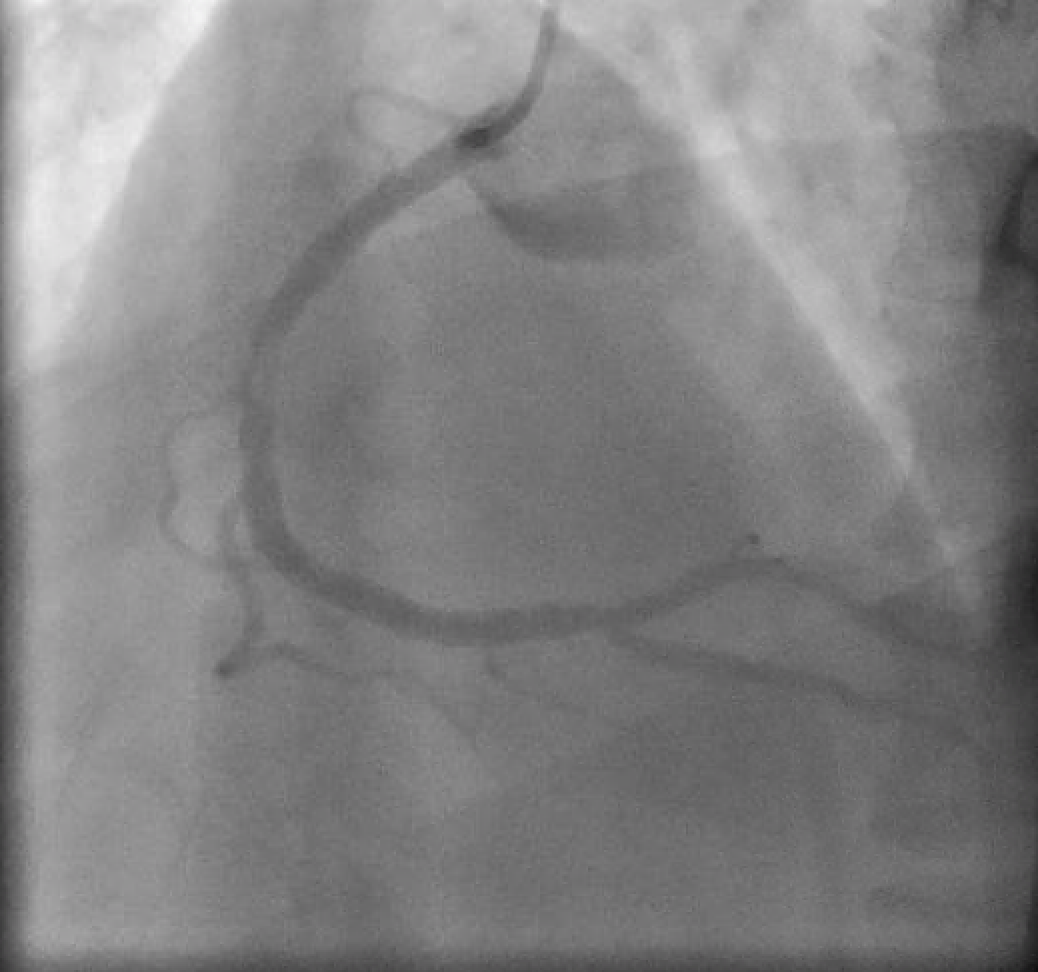
Image 4:EKG on re- admission with complain of persistent chest pain, with no significant EKG changes or ST-T wave abnormality. Patient did have positive cardiac markers blood.
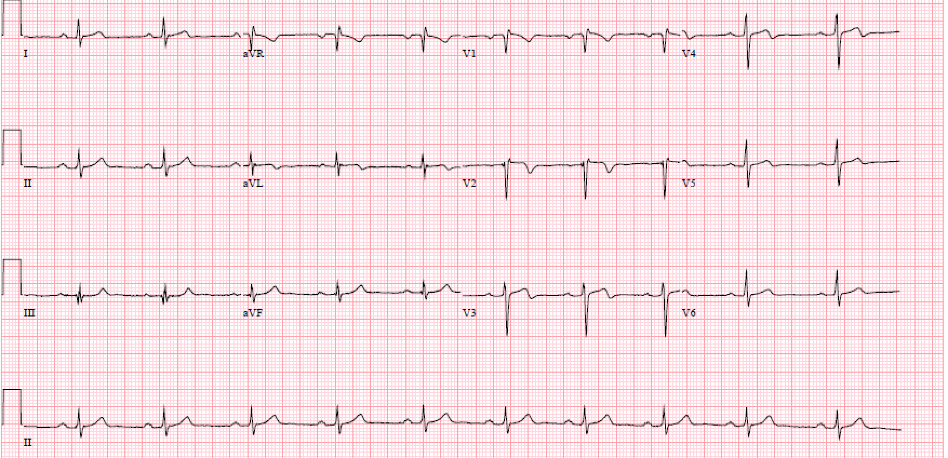
Image 5:Repeat cath showed 90 % stenosis of LAD inexactly a period of one month.

Image 6:The LAD after the guide wire, it was treated with one DES.

Image 7: RCA Was patent on repeat cath.
Citation: Mahida H, Gharia B, Pinnales D (2020) Cardiovascular Adverse event after the use of Varenicline: A Case Report and Literature Review. Ann Med &Surg Case Rep: AMSCR-100071