Journal of Surgery and Insights
(ISSN 2652-4643)
Research Article
Comparison of the Initial D-Dimers Concentration Determined in a Patient Group with Coxarthrosis or Gonarthrosis and in a Group with Femoral Bone Fracture
Lukasz Kacprzak1,2, Piotr Bytniewski2,3
1Department of Pharmacodynamics, Medical University of Lodz, Poland
2Department of Anaesthesiology, Health Maintenance Organization in Turek, Poland
3Faculty of Physical Education and Health Preservation, The State School of Professional Higher Education in Konin, Poland
*Corresponding authors: ?ukasz Kacprzak, Department of Pharmacodynamics, Medical University of Lodz, Poland.
Piotr Bytniewski, Department of Anaesthesiology, Health Maintenance Organization in Turek, Poland, Faculty of Physical Education and Health Preservation, The State School of Professional Higher Education in Konin, Poland.
Citation: Kacprzak L and Bytniewski P (2020) Comparison of the Initial D-Dimers Concentration Determined in a Patient Group with Coxarthrosis or Gonarthrosis and in a Group with Femoral Bone Fracture. J Surg Insights: JSI-100021.
Received date: 12 June, 2020; Accepted date: 02 July, 2020; Published date: 07 July, 2020
Abstract
Introduction: D-dimers are the products of fibrin degradation by thrombin, factor XIIIa and plasmin. Their blood concentration is used in clinical diagnostics for venous thromboembolism (VTE) which involves deep vein thrombosis (DVT) and pulmonary embolism (PE).
Purpose: Surgical operations within the femoral bone are one of the most often performed ones in orthopedic wards. In order to determine an impact of bone injury on the risk of occurrence of a thromboembolic disease we compared the preoperative concentration of D-dimers between a group of patients hospitalized due to femur fracture and a group of patients hospitalized due to coxarthrosis or gonarthrosis.
Material and methods: The study involved overall 404 patients, divided into two groups. The first group enrolled 283 patients who underwent elective surgery on the femoral bone: total hip replacement (THR) and total knee replacement (TKR) due to osteoarthritis of large joints. This group was divided into detailed subgroups to determine the difference in the impact of a degenerated joint on D-dimer concentration. The second group enrolled 121 patients who underwent surgery due to femoral fracture. All patients underwent a physical examination for an occurrence of varicose veins in lower limbs. No clinical features of venous thromboembolism were found in patients qualified for the study, based on examination of the venous system in lower limbs, which was supplemented by ultrasound examination. Pre-operation blood concentrations of D-dimers were measured in all participants.
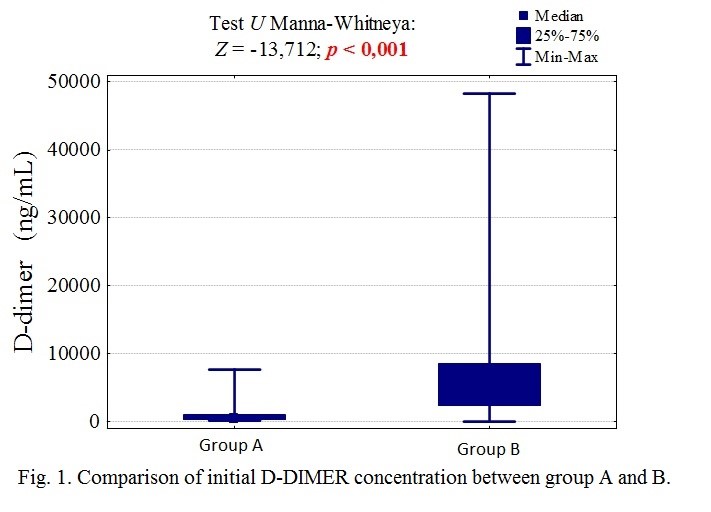
Results: In patients undergoing scheduled surgery due to coxarthrosis or gonarthrosis D-dimers concentrations ranged between 122 and 7712 ng/mL, with a mean of 822.3 ng/mL (SD 811.2 ng/mL). It was markedly lower than that found in patients with femur fracture: range from 23.6 to 48340 ng/mL, mean 8793.2 ng/mL (SD ± 10358.6 ng/mL).
Conclusions: It is suggested that elevated D-dimers levels observed in patients with femur fracture are not associated with an increased risk of occurrence of a thromboembolic disease.
Keywords: D-dimers, Total hip replacement, Total knee replacement, Femoral fracture
Abbreviations
VTE : Venous Thromboembolism
DVT : Deep Vein Thrombosis
PE : Pulmonary Embolism
THR : Total Hip Replacement
TKR : Total Knee Replacement
DHS : Dynamic Hip Screw
PFN : Proximal Femoral Nail
BMI : Body Mass Index
ASA : American Society of Anesthesiologists
Introduction
D - dimers were discovered in the 1970s, and their blood concentration was used in a clinical practice in the 1990s. They are protein product of fibrin degradation by thrombin, factor XIIIa and plasmin. Determination of plasma D - dimers concentration is used in diagnosis of venous thromboembolism (VTE), which includes deep vein thrombosis (DVT) and pulmonary embolism (PE). Low concentration of D - dimers allows to exclude the ongoing thromboembolic process, which indicates a large negative predictive value of this laboratory test. The commonly used cut-off value is a concentration below 500 ng/mL, while higher concentrations indicate clinically significant VTE and such cases require in-depth diagnostics. Although D-dimers are formed by degradation of fibrin, fibrin itself is not only associated with venous thromboembolism. Increased fibrin production, which is manifested by elevated D-dimers concentration, can also be seen in other clinical conditions such as cancer, infection, ongoing inflammation, surgery, injuries, hemorrhages, extensive burns, stroke, aortic aneurysm rupture, ischemia, heart disease, myocardial infarction, rheumatoid arthritis, pregnancy and the postpartum period, as well as in elderly patients, patients with hematomas, extensive bruising and many others. [26]. Different methods used for measuring D-dimers concentration have a specificity of 93-95%, while their sensitivity is only about 50% [1,2]. Some authors suggest the correction of the D-dimers concentration determination for the patient's age using the cut-off age (in years) x 5 or x10. This allows increased specificity of the study among older patients [3,4,5].
Surgical operations within the femoral bone are one of the most often performed ones in orthopedic wards. In case of elective surgeries we deal with total hip replacement (THR) and a total knee replacement (TKR). However, in cases of of fractures, it is necessary to use an appropriate prosthesis or osteosynthesis using a dynamic hip screw (DHS) or a proximal femoral intramedullary nail (PF). All these procedures are at risk of thromboembolic complications [6,7]. In order to determine the impact of bone injury on this type of risk we compared the preoperative concentration of D-dimers between a group of patients hospitalized because of a femoral fracture and a group of patients hospitalized because of coxarthrosis or gonarthrosis.
Patients and Research Methods
In this retrospective study we analyze medical records of patients, who were operated at Orthopedics Department of SPZOZ in Turek (Poland) between August and November, 2011. Bioethics Committee of Medical University of ?odz allowed for data analysis; decision number: RNN/249/19/KE, issued: 14/05/2019.
Patients who were excluded from the analysis:
Before qualifying for the study, data were obtained from the subjects by means of an interview and physical examination. The interview included past and accompanying chronic diseases, their current condition and undertaken therapy. The patients were examined in terms of the condition of the respiratory and circulatory systems and occurrence of varicose veins in lower limbs. No clinical features of venous thromboembolism were found in patients qualified for the research, based on examination of the venous system in lower limbs, which was supplemented by ultrasound examination.
Medical records of two groups of patients were analyzed. The first group enrolled 283 patients hospitalized due to osteoarthritis of the hip or knee, including 186 women and 97 men, at the age between 29 and 87 years. The mean age was 65.59 years. This group was labeled as group “A” and was divided into detailed subgroups to determine the difference in impact of the degenerated joint on the D-dimer concentration. The subgroups were labeled as “H” for the hip joint and “K” for the knee joint.
The second group enrolled 121 patients hospitalized for a femoral fracture, including 97 women and 24 men. The age ranged between 48 and 99 years and the mean age was 77.38 years. Body mass index (BMI) was calculated for all patients. This group was labeled as group “B”. Characteristics of both main groups of patients in terms of age, sex, BMI, operation risk assessment and type of surgery are presented in (Table 1). The operational risk associated with the occurrence of serious complications or death during or after anesthesia was determined according to the ASA scale [8]. The study included only preoperative determination of D-dimers concentration, as the surgery by itself could increase their levels [9]. Concentration of D-dimers in blood plasma was measured by an enzyme immunoassay test VIDAS D-Dimer Exclusion, conducted in VIDAS immunology analyzer (BioMérieux, Marcy-l'Étoile, France) and based on marking fibrin degradation products (FbDP), using an enzyme-linked fluorescent assay (ELFA).
Data collected from both groups were analyzed using Statistica 10 (Statsoft Dell, Tusla, OK, USA). P <0.05 was considered statistically significant. Comparison between groups in this study were done by applying Student's t-distribution and Mann-Whitney U tests.
Results
Among 283 patients with osteoarthritis of the hip or knee (group A) D-dimers' levels ranged between 122 and 7712 ng/mL, with the mean of 822.34 ng/mL (SD ± 891.2 ng /mL). The mean preoperative D-dimers’ concentration for women in this group was 896.9 ng/mL ± 988.0, while in men 679.4 ng/mL ± .648.6. The average BMI in this study group was 29.22 ± 4.7 kg/m2. The comparison of age, BMI and preoperative D-dimer concentration of women and men in group A did not show any statistically significant differences. The data have been shown in (Table 2).
Analysis of data did not show statistically meaningful correlations between BMI or ASA qualification of patients and pre-operative D-dimers' concentration.
The patients of group “A” were further analyzed depending on the joint affected by osteoarthritis. Subgroup “H” consisted of 193 patients who underwent cementless or cemented hip replacement. The hip replacement group consisted of 133 men and 60 women with mean age of 65.2 ± 10.7 years and mean BMI of 28.6 ± 4.6 kg/m2. The mean preoperative D-dimers' level for this group was 879 ± 943 ng/mL. The second subgroup, “K”, consisted of 90 patients that underwent total knee replacement. The mean age within this group was 66.5 ± 7.8 years and mean BMI 30.5 ± 4.7 kg/m2. The mean preoperative D-dimers' level for this group was 701 ± 760 ng/mL. A direct comparison of both subgroups showed statistically significant differences in BMI (p = 0.001) and pre-operative D-dimers' concentration (p = 0.044). These data are presented in (Table 5). A higher BMI occurring in patients operated on due to osteoarthritis of the knee may be associated with a greater load on this joint which results from excessive body weight. In contrast, osteoarthritis of the hip correlates with a higher range of preoperative D-dimers' concentration. It is most likely related to the size of the affected joint.
Among 121 patients with femur fracture (group B) D-dimers' levels ranged between 23.55 and 48340 ng/mL, with a mean of 8793.2 ± 10358.6 ng/mL. The mean preoperative D-dimers' level for women in this group was 8463.2 ± 9653.2 ng/mL, while in men 10126.6 ng/ml ± 12983.5 ng/ml. The difference of average age between men and women in group B was statistically significant (p=0,0005). The difference of average BMI between men and women in group B was statistically significant (p<0,0001) The comparison of preoperative D-dimer concentration of women and men in group B did not show any statistically significant differences The data have been shown in (Table 3).
The obtained data do not indicate any meaningful correlations between the analyzed parameters.
The statistical difference in overall preoperative D-dimers' concentration between the two groups is statistically significant (p <0.001). The femoral fracture causes a higher preoperative D-dimer concentration in patient’s blood than chronic arthritis of large joints. These data are shown in (Table 4 and Figure 1). The increase of D-dimer concentration in the study group was not associated with an increased risk of thromboembolic disease. No clinical features of venous thromboembolism were found in patients based on examination of the venous system in lower limbs, which was supplemented by ultrasound examination.
Discussion
Preoperative blood level of D-dimers presented in the present study shows how much fracture may increase this parameter compared to a chronic degenerative process. Similar results were obtained by Hagiwara et al. who showed correlations between the concentration of D-dimers at the time of admission to the hospital and the severity of an injury according to Injury Severity Score [10]. Yu-Jun Zhu et al. demonstrated elevated concentrations of D-dimers in various types of injuries, regardless of the part of the body [11], it is difficult to determine whether observed by us differences between men and women result from gender or general health condition of patients in the studied population.
In the previous research by Bytniewski et al. conducted on a group of 47 patients at the age of 29-82, who were treated for coxarthrosis and underwent total hip replacement (THR) using both cemented and uncemented prostheses, the initial preoperative D-dimers' concentrations exceeded the reference value of 500 ng/mL in 37 out of 47 patients, with a mean value ranging from 1077.2 to 2075.5 ng/mL, depending on the age group [26]. Thus, the cited data indicate that an increase in D - dimers concentration after surgery is not associated with a higher risk of thromboembolic disease. In line with this, Wa?ko et al. demonstrated that concentration of D-dimers before scheduled hip replacement is above the limit (500 ng/mL), but does not correlate with the risk of thromboembolic events. Thus, D-dimers should be considered as an acute phase proteins [12].
Degenerative disease may be considered a factor of hypercoagulability leading to an increase of laboratory parameters, including blood D-dimers levels [13,14]. According to Mameli and Marongiu, patients with rheumatoid arthritis who demand orthopedic intervention, are at a similar risk of thromboembolic complications than a general population taking appropriate prophylaxis into account [15]. In turn, Mukubo and Kawamata argue that patients suffering from rheumatoid arthritis have a higher preoperative concentrations of D-dimers than patients operated due to hip joint osteoarthritis [25]. The issue undoubtedly requires further research.
One should bear in mind the necessity of correction of the cut-off point, taking into account patients' age (age in years x 10ng/over 50 years old), which can be observed in the group of patients operated due to osteoarthritis of the hip or knee [16-18].
Liu et al. point out the difference in the magnitude of increased the concentrations of D-dimers which were dependent on a fracture’s location; the highest changes are observed in cases of fractures localized, close to the femoral bone (mean concentration of D-dimers: 2448 ± 1961 ng/mL) [19]. Differences may result from the diversity of the population or the size of the studied subjects. Other authors also indicate the impact of femoral fracture on functioning of coagulation system. So, not surprisingly, it is difficult to interpret D-dimers levels in patients suffering from trauma [20-21].
While examining patients hospitalized for femur fracture prior to the surgery Luksameearunothai et al. did not observe significant differences in D-dimers levels between patients who developed deep vein thrombosis (DVT) and the remaining ones. All injured patients had a significantly elevated concentrations of D-dimers [22]. It should also be borne in mind that older patients may suffer from previously recognized thromboembolic disorders. Therefore, when clinical symptoms occur, other diagnostic tools, such as Doppler ultrasonography and computed tomography with the administration of a contrast agent should be used [23]. In our study, ultrasound diagnostics excluded the ongoing thromboembolic process in both examined groups, despite the increased concentrations of D-dimers.
Niikura, et al [24] claim that in the group of patients who incurred a high-energy fracture, the concentration of D-dimers is of significant importance in the diagnosis of thromboembolic complications.
Our study has numerous limitations. First of all, this is a retrospective analysis conducted in one medical center only. Despite a significant number of patients included in the research, it would be vital to perform a multi-center research.
Conclusions
Declarations
Ethics approval and consent to participate
The Bioethics Committee of the Medical University of Lodz allowed the study and analysis of the collected data; Decision number: RNN / 249/19 / EC, issued: 14/05/2019.
All study participants gave informed consent to participate in the study in the form of a written questionnaire presented to them by the authors.
Consent for publication
Both authors read and approved of the final manuscript for publication in the Journal of Surgery and Insights.
Acknowledgments
All data were acquired at Department of Orthopedics and Traumatology, Health Maintenance Organization in Turek, 1 Poduchowne Street, 62-700 Turek, Poland.
Availability of data and materials
The data that support the findings of this study are available from Health Maintenance Organization in Turek but restrictions apply to the availability of the data which were used under permission of the director of medical affairs of Health Maintenance Organization in Turek for the current study, and so are not publicly accessible. However, the data are available from the authors upon reasonable request and with permission of Health Maintenance Organization in Turek.
Competing interests
The authors declare that they have no competing interests.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Authors' contribution
?ukasz Kacprzak and Piotr Bytniewski conceived of the study, participated in its design and coordination and helped to draft the manuscript. ?ukasz Kacprzak and Piotr Bytniewski carried out the design of the study and the statistical analysis. ?ukasz Kacprzak was responsible for editing the text and tables, preparation of the edition of this manuscript for publication and translation into English.
|
|
Reason for hospitalization |
|||
|
Coxarthrosis or gonarthrosis Group A (n = 283) |
Femur fracture Group B (n = 121) |
|||
|
Age (mean ± SD) |
65.60 ± 9.88 |
77.38 ± 12.43 |
||
|
Age (min) |
29 |
48 |
||
|
Age (max) |
87 |
99 |
||
|
BMI (mean ± SD) |
29.22 ± 4.70 |
25.30 ± 4.60 |
||
|
BMI (min) |
16.91 |
16.49 |
||
|
BMI(max) |
44.44 |
41.52 |
||
|
Woman |
n = 186 |
n = 97 |
||
|
Age (mean ± SD) |
66.29 ± 10.39 |
79.31 ± 11.24 |
||
|
BMI (mean ± SD) |
29.27 ± 4.8 |
21.13 ± 4,81 |
||
|
Men |
n = 97 |
n = 24 |
||
|
Age (mean ± SD) |
64.27 ± 8.70 |
69.60 ± 14.14 |
||
|
BMI (mean ±SD) |
29.11 ± 4.37 |
25.97 ± 3.60 |
||
|
Operational risk (ASA scale): |
n |
% |
n |
% |
|
I |
19 |
6,7 |
0 |
0,0 |
|
II |
87 |
30,7 |
12 |
9,9 |
|
III |
151 |
53,4 |
22 |
18,2 |
|
IV |
26 |
9,2 |
87 |
71,9 |
|
Type of surgery: |
|
|
||
|
Cementless partial hip replacement |
165 |
58,3% |
0 |
0,0% |
|
Cemented hip partial replacement |
28 |
9,9% |
0 |
0,0% |
|
DHS |
0 |
0,0% |
42 |
34,7% |
|
Total knee replacement |
90 |
31,8% |
0 |
0,0% |
|
Itramedullary nail PF |
0 |
0,0% |
37 |
30,6% |
|
Cementless total hip replacement |
0 |
0,0% |
11 |
9,1% |
|
Cemented total hip replacement |
0 |
0,0% |
1 |
0,8% |
|
Elliptical half prosthesis for hip joint |
0 |
0,0% |
30 |
24,8% |
Table 1: Characteristics of the study groups.
|
Gender
|
ASA scores |
Number of patients |
Age (years; mean ± SD) |
BMI (kg/m2, mean ± SD) |
Preoperative D-dimer concentration (ng/mL, mean ± SD) |
|
Women overall |
- |
186 |
66.29 ± 10.39 |
29.27 ± 4.87 |
896,9 ± 988.0 |
|
Women |
1 |
11 |
42.27 ± 7.78 |
25.14 ± 3.35 |
264.3 ± 126.5 |
|
2 |
55 |
62.20 ± 7.08 |
28.58 ± 4.37 |
708.4 ± 654.7 |
|
|
3 |
107 |
69.77 ± 7.82 |
30.34 ± 4.87 |
1083.46±1167.23 |
|
|
4 |
13 |
75.31 ± 6.96 |
26.,90 ± 5.24 |
694. 4 ± 431.8 |
|
|
Men overall |
- |
97 |
64.27 ± 8.70 |
29.11 ± 4.37 |
679.4 ± 648.6 |
|
Men |
1 |
8 |
52.62 ± 5.10 |
29.60 ± 5.23 |
654.8 ± 715.8 |
|
2 |
32 |
61.16 ± 8.95 |
28.33 ± 4.26 |
468.5 ± 241.3 |
|
|
3 |
44 |
66.57 ± 7.04 |
29.27 ± 4.,44 |
724.8 ± 697.6 |
|
|
4 |
13 |
71.31 ± 4.17 |
30.19 ± 4.03 |
1060.1 ± 942.8 |
|
|
Group overall |
- |
283 |
65.60 ± 9.88 |
29.22 ± 4.70 |
8224.0 ± 891.2 |
|
Women vs. men p |
0.102 |
0.786 |
0.051 |
||
Table 2: ASA scores, BMI and preoperative blood D-dimer concentrations in the group A
|
|
Group H N = 193 |
Group K N = 90 |
H vs. K p |
||
|
Sex: |
n |
% |
n |
% |
0,246 |
|
Woman |
116 |
60,1% |
70 |
78,8% |
|
|
Men |
77 |
39,9% |
20 |
22,2% |
|
|
Age |
|
|
0,295 |
||
|
M ± SD |
65,2 ± 10,7 |
66,5 ± 7,8 |
|||
|
Me [Q1; Q3] |
66 [59; 73] |
66 [61; 73] |
|||
|
Min - Max |
29 - 87 |
45 - 85 |
|||
|
BMI (kg/m2): |
|
|
0,001 |
||
|
M ± SD |
28,6 ± 4,6 |
30,5 ± 4,7 |
|||
|
Me [Q1; Q3] |
29 [25; 32] |
31 [28; 34] |
|||
|
Min - Max |
19 - 41 |
17 - 44 |
|||
|
D-dimer (ng/mL): |
|
|
0,044 |
||
|
M ± SD |
879 ± 943 |
701 ± 760 |
|||
|
Me [Q1; Q3] |
561 [353; 1036] |
455 [313; 777] |
|||
|
Min - Max |
124 - 7712 |
122 - 5237 |
|||
|
Operational risk (ASA scale): |
n |
% |
n |
% |
0,113 |
|
I |
17 |
8,8 |
2 |
2,2 |
|
|
II |
59 |
30,6 |
28 |
31,1 |
|
|
III |
97 |
50,3 |
54 |
60,0 |
|
|
IV |
20 |
10,4 |
6 |
6,7 |
|
Table 5: Characteristics and comparison of subgroups H and K.
|
Gender
|
ASA scores |
Number of patients |
Age (years; mean ± SD) |
BMI (kg/m2; mean ± SD) |
Preoperative D-dimer concentration (ng/mL; mean ± SD) |
|
Women overall |
- |
97 |
79.31 ± 11.24 |
21.13 ± 4.81 |
8463.2 ± 9653.2 |
|
Women |
1 |
- |
- |
- |
- |
|
2 |
9 |
61.78 ± 7,39 |
26.18 ± 2.85 |
6033.8 ± 4025.0 |
|
|
3 |
17 |
72.12 ± 10.41 |
25. 94 ± 4.60 |
6435.9 ±1 1360.7 |
|
|
4 |
71 |
83.25 ± 8.63 |
24.80 ± 5.06 |
9256.6 ± 9697.8 |
|
|
Men overall |
- |
24 |
69.60 ± 14.14 |
25.97 ± 3.60 |
10126.6 ± 12983.5 |
|
Men |
1 |
- |
- |
- |
- |
|
2 |
3 |
57.67 ± 7.23 |
24.6 0± 2.06 |
16268.7 ± 2545.8 |
|
|
3 |
5 |
62.60 ± 9.91 |
23.73 ± 0.88 |
9473.0 ± 10515.2 |
|
|
4 |
16 |
74.00 ± 14.43 |
26.93 ± 4.01 |
9179.2 ± 11692.2 |
|
|
Group overall |
- |
121 |
77.38 ± 12.43 |
25.30 ± 4.60 |
8793.2 ± 10358.6 |
|
Women vs. men p |
0.0005 |
<0.0001 |
0.483 |
||
Table 3: ASA scores, BMI and preoperative blood D-dimer concentrations in the group B
|
D-dimery (ng/mL): |
Overall |
Group A |
Group B |
A vs. B p |
|
M ± SD |
3210 ± 6773 |
822 ± 891 |
8793 ± 10359 |
<0,001 |
|
Me [Q1; Q3] |
772 [392; 2431] |
502 [337; 1002] |
5109 [2342; 8610] |
|
|
Min - Max |
24 - 48340 |
122 - 7712 |
24 - 48340 |
Table 4: Comparison of initial D-DIMER concentration between group A and B.
Citation: Kacprzak L and Bytniewski P (2020) Comparison of the Initial D-Dimers Concentration Determined in a Patient Group with Coxarthrosis or Gonarthrosis and in a Group with Femoral Bone Fracture. J Surg Insights: JSI-100021.