Emerging Infectious Diseases and Diagnosis Journal
Research Article
Exophytic Hydatid Cyst of Liver-an Ominous Sign
Rastogi R1*, Neha1, Pratap V1 and Bhargava S2
1Department of Radiodiagnosis,Teerthanker Mahaveer Medical College & Research Center, Moradabad, Uttar Pradesh, India
2MSY Medical College & Hospital, Meerut-Hapur Road, Meerut, Uttar Pradesh, India
*Corresponding author: Rajul Rastogi, Department of Radiodiagnosis,Teerthanker Mahaveer Medical College & Research Center, Moradabad, Uttar Pradesh, India, Email: eesharastogi@gmail.com
Citation: Rastogi R, Neha, Pratap V, Bhargava S (2020) Exophytic Hydatid Cyst of Liver-an Ominous Sign. Emerg Infect Dis Diag J: EIDDJ-100022
Received date: 04 May, 2020; Accepted date: 04 June, 2020; Published date: 15 June, 2020
Hydatid disease though has reduced in incidence worldwide including the developing world yet is still one of the dreaded diseases escaping early detection. Liver is the most involved organ with majority being asymptomatic and associated with little morbidity. Rarely, the hydatid cyst may be exophytic when it may be associated with pain and risk of rupturealong withitsmost- dreaded complication i.e. anaphylaxis.Hence, exophytic hydatid cyst is considered an ominous sign that can be diagnosed readily on widely available imaging modality i.e. computed tomography of abdomen and hence can prevent further complications.
Keywords: Exophytic; Hydatid cyst, Liver, Ominous sign
Introduction
Hydatid disease is a parasitic disease caused by Echinococcosis, mainly E. Granulosus and uncommonly by E. Multilocularis [1]. Though the prevalence of hydatid disease in developing world has reduced significantly yet it is still one of the diseases that often escape early detection. Liver is the most- commonly involved organ followed by lung with majority of the cases being asymptomatic and associated with little morbidity[2-4]. The posterior segment of the right hepatic lobe is the commonest segment to be involved.
Uncommonly, the center of the hepatic hydatid cyst may lie beyond the confines of the hepatic parenchyma producing a surface bulge with no identifiable rim of hepatic parenchyma resulting in exophytic hydatid cystwhen it may cause pain and may rupture secondary to trauma or elective surgery and many a time spontaneously leading to morbidities[5, 6].Rupture may occur into biliary tract, lung, pleural space, mediastinum, heart. pericardium and peritoneal cavity[1].The common risk factors for rupture include young age as they are more exposed to trauma, diameter more than 10 cm as intracystic pressure increases with
increasing diameter and superficial/subscapular location [2, 5]. The surface bulge is usually responsible for pain as Glisson’s capsule is innervated by sensory nerves. This may be the first warning clinical sign[2, 4, 5].The hydatid cyst is termed as subcapsular when it reaches within 10mm of the hepatic capsule or surface. This may be the first ominous radiological sign.This sign along with other can be easily detected on computed tomography of abdomenusing multiplane reconstruction images [7, 8].
Cyst when exophytic has the propensity to rupture and directly disseminate to the adjacent body cavities and organs making the disease widespread and difficult to manage. Anaphylaxis is the most-dreaded complication especially common with intraperitoneal rupture of hydatid cyst[1, 2, 4, 5]. Hence in this study, we evaluated a series of symptomatic hydatid disease of liver with computed tomography and recorded the presence of this ominous sign.
Aim of the study: To evaluate patients with symptomatic hydatid liver cyst for exophytic cyst with computed tomography of abdomen
Material and Methods
Twenty-four patients irrespective of age & sexwith symptomatic hydatid disease of liver were evaluated by triple- phase, contrast-enhancedcomputed tomography of abdomen (CT- Ab).Symptoms included pain lower chest, localized pain right upper abdomen and diffuse pain abdomen.
All patients had prior ultrasonography of liver (USG-L) and serological diagnosis of hepatic hydatidosis.The hepatic lesions were evaluated in axial, coronal and sagittal planes using multiplanar reconstruction images of CT-Ab. The presence of exophytic cystwas recorded.
Results and Observations
Among the twenty-four patients, localized right upper abdomen painwas the commonest symptom. Figure 1 shows the distribution of patients with different presentation in the form of pie-chart.
In our study, right hepatic lobe involvement was commoner than left lobe with 21 out of 24 cases showingright hepatic lobe involvement. Figure 2 shows the same.
All the twenty-four patients revealed subcapsular location of hydatid cyst of liver. Of these, only four patients revealed exophytic hydatid cyst with more than 180 degrees’ circumference in subcapsular location(Image 1).
Two of four patients with exophytic cyst revealed rupture on hepatic surface(Image 2,3).
In our study, however, none of the patients were noted with any degree of anaphylactic reaction.
In our study, 16.7% of symptomatic patients had exophytic cysts and 50% of exophytic cysts had contained rupture at the time of presentation.
Discussion
Hydatid disease has a global incidence of nearly 1-200 per one lac population with hepatic disease incidence of 22-72% [9, 10]. Prior to era of cross-sectional imaging, the early and correct diagnosis of exophytic hydatid cyst of liver was often delayed with attention being drawn only by complications.Rupture of hydatid cyst of liver is not only associated with significant morbidity but also with dreaded complication of anaphylaxis.With the advent of computed tomography, it is now possible to image and evaluate the hydatid cyst from all around using isotropic multiplane reconstruction images[11].
The characteristic radiological ominous sign is exophytic hydatid cyst which may revealperihepatic rupture, adherence to diaphragm and mural thickening with lobulations of cyst [10]. The most common sites of exophytic hydatid disease with secondary rupture and spread is bare hepatic area and gastrohepatic ligament [11]. CT-Ab can detect abovefeatures including beak-sign in very large exophytic cyst (breaking of hepatic parenchymaaround the cyst suggesting hepatic origin) in early stage to prevent further complications[7]. During the process of evolution, there may be calcification within the cyst representing the evolving death of the parasite seen as curvilinear or ring-like calcifications in one-third patients on radiography but more sensitively with CT-Ab[12]. Not much medical literature exists on the ominous sign except for isolated case reports or series[12, 13].
In our study, we tried to evaluate the significance of symptomatic hydatid cyst of liver and its further radiological evaluation by CT-Ab to detect this ominous sign at an early stage preventing further complications. Our study reinforces the significance of exophytic cyst as ominous radiological sign.
Exophytic cysts have to be treated on emergency basis as it will not only prevent anaphylaxis but will also minimize the risk of secondary peritoneal hydatidosis [2, 4, 5]. The standard mode of treatment for exophytic hydatid cyst is complete surgical excision of the intact cyst [13, 14]. Medical treatment with albendazole is reserved for inoperable, recurrent and extrahepatic disease [13, 15].
Conclusion
Computed tomography of abdomen is an extremely useful modality for imaging of symptomatic hydatid cysts of liver to detect its exophytic nature which is an ominous signthat may not be apparent clinically or may even escape detection on routine ultrasonography of abdomen. Hence, it should be used routinely in such patients to prevent further complications.
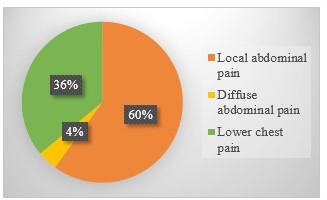
Figure 1: Distribution of Patients Based on Location of pain.
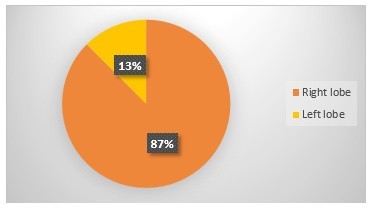
Figure 2: Distribution of Patients Based on Hepatic Lobar Location.
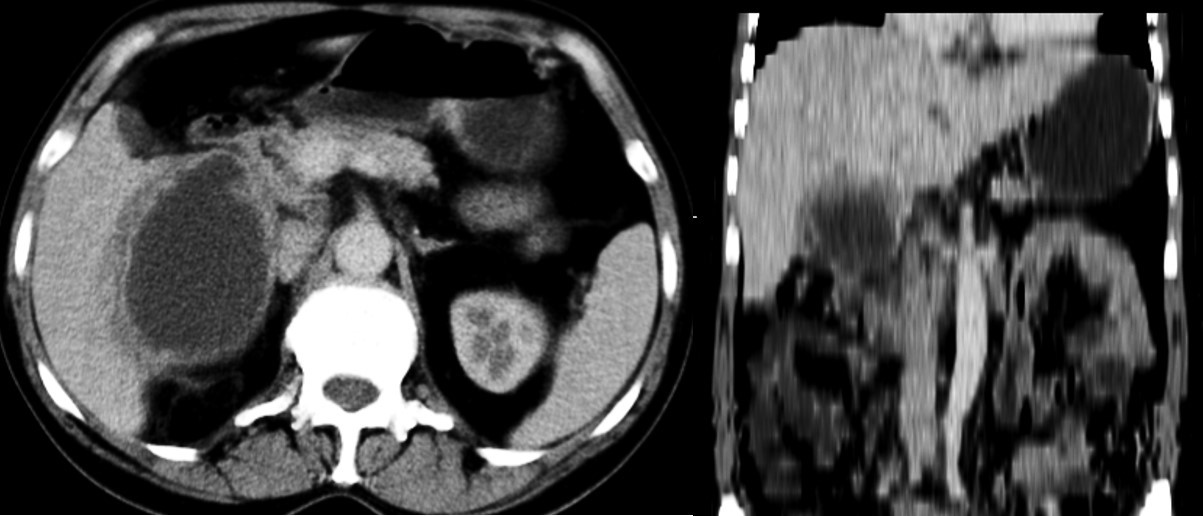
Image 1: CECT images in axial (left) and coronal (right) planes show large active exophytic hydatid cyst growing in Gastrohepatic ligament.

Image 2: CECT abdomen image in axial plane shows healing exophytic hydatid cyst with rupture in perihepatic space.

Image 3: CECT abdomen image in axial plane showing healing exophytic hydatid cyst in bare area of liver rupturing in to perihepatic space.
Citation: Rastogi R, Neha, Pratap V, Bhargava S (2020) Exophytic Hydatid Cyst of Liver-an Ominous Sign. Emerg Infect Dis Diag J: EIDDJ-100022