Journal of Surgery and Insights
ISSN 2652-4643
Case Report
The Fasciocutaneous Propeller Flap Based on a Perforating Branch of the Ulnar Artery to Repair Radial Forearm Free Flapdonor Site: A Case Report
Mangialardi ML1,2*, Vitagliano S1and Salgarello M1,2
1Fondazione Policlinico Agostino Gemelli IRCCS, Rome, Italy
2UniversitàCattolica del SacroCuore, Rome, Italy
*Corresponding author: Maria Lucia Mangialardi, Fondazione Policlinico Agostino Gemelli IRCCS, Rome, Italy
Citation: Mangialardi ML, Vitagliano S, Salgarello M(2020) The Fasciocutaneous Propeller Flap Based on a Perforating Branch of the Ulnar Artery to Repair Radial Forearm Free Flap donor Site : A Case Report. J Surg Insights: JSI-100013
Received date: 06 March, 2020; Accepted date: 19 June, 2020; Published date: 22 June, 2020
Introduction
Radial forearm free flap (RFFF) currently represents a workhorse in head and neck reconstruction. The main disadvantage of this flap is its donor site morbidity. The most used technique to repair the RFFF donor site is a split-thickness skin graft that often results in poor aesthetic and functional outcomes, causing cosmetic deformity and reduced wrist mobility. In this article we describe a case of RFFF donor site repair using a propeller flap based on a single perforating branch of ulnar artery in a 67-year-old patient affected by a squamocellular carcinoma on the left lateral tongue. In our opinion this technique offers a consistent tendons and nerves protection, a better quality of scar and avoids the reduction of wrist mobility, resulting in a better aesthetic and functional result.
Keywords: Donor site; Ulnar perforator propeller flap
Introduction
Radial fore arm free flap (RFFF) was first described by Yang et al [1] and currently represents a work horse in head and neck reconstruction. The main advantages of RFFF are its pliability and thinness, a suitable pedicle length and a favorable vessel size that perfectly match with neck vessels. On the other side, the main disadvantage of RFFF is the significant donor site morbidity that hesitates in a scar so apparent that is difficult to accept for many patients.
The most used technique to repair the donor site is a split- thickness skin graft. However the flexor tendon paratenon is an unfavorable bed for a split-thickness skin graft [2-3], resulting often in a delayed wound healing with tendon exposure. Furthermore, graft retraction causes poor aesthetic and functional results [2-4]. Long-term consequences are cosmetic deformity [2-4], reduced wrist mobility, wrist or hand weakness[4-5], sensory deficits[3,6,7] and persisting pain [2,8]. Moreover the need of a skin graft to cover the donor site implies a supplemental scar. In this article we describe a case of RFFF donor site repair using apropeller flap based on a single perforating branch of ulnar artery.
Case Report
A 67-year-old female patient affected by a squamocellular carcinoma on the left lateral tongue underwent a left partial glossectomy and left selective neck dissection of levels I-IV. At the end of the resection the defect was extended to the floor of mouth measuring 4.5 × 6.5 cm, including the excision of the lesion with 1 cm around its borders to ensure that the margins were free of malignancy.
Reconstruction of the intraoral defect was performed using a left RFFF. The choice of the donor site side was based on patient dominance (right-handed) and on preoperative Allen test. RFFF design was based on defect size and reconstructive needs resulting in a 6.5 × 4.5cm defect (Figure 1).
A supra fascial dissection was performed under Tourniquet control. Ulnar perforator propeller flap: the inter muscular septum- between flexordigitorum superficial is and flexor carpi ulnaris was marked by a line drawn from the pisiform to the medial epicon- dyle. An intraoperative Doppler signal mapping was performed on this line. When a pulsatile, loud and high pitched signal was detected by the probe, a marking point was made (7.2cm from the pisiform). The perforator branch was dissected in the septum (Fig- ure 2).
A flap of 5.5 × 7cm was designed and rotated of 90 degrees in order to cover the defect on the palmarwrist caused by the RFFF.
The donor site of ulnar artery perforator flap was closed by the advancement of the local skin. A little defect of 2.5 × 1.5cm on the proximal part of the forearm was reconstructed by a full-thickness skin graft harvested on the inner face of the arm.
Discussion
Ulnar artery based transposition flap (UBTF) was first described by Elliot et al [9]to repair a RFFF donor site. Potet et al [10] used the ulnar artery based flap as a “keystone” to reconstruct small and medium radial forearm donor site. Moreover, Hsieh et al [11] described a case series of 10 patients undergone a RFFF donor site repair by a bilobed flap based on ulnar artery perforator. The surgical technique included bilobed flap harvesting and the rotation of 90 degrees, using the large lobe to close the donor site of the RFFF and the small lobe to close the donor site of the large lobe. In this series all donor defects were closed without major complications. However, in our opinion this technique offers a poor aesthetic outcome because of multiple curved scars. Shoaib [12] used an ulnar artery perforator based islanded V-Y flap for RFFF donor site repairin 5 cases. The RFFF design was orientated transversely along the distal volar aspect of the wrist where the skin is thinner, around wrist creases. All 5 flaps were successfully harvested and completely closed the defects. In two cases the medial superficial veins and the medial cutaneous nerve were divided in order to allow flap advancement but in both cases a postoperative edema was reported.
Subsequently, Jaquet [13] compared 22 patients who had split-thickness skin graft with 22 patients who had ulnar based transposition flap closure showing a significantly better wrist extension in the UBTF group. However the technique described by Elliott, can be used only to repair small defects (8 × 4cm). Lastly, ulnar perforator flaps can be used also for coverage of secondary tendon exposure after RFFF[14].
In our opinion the use of the ulnar perforator flap as a propeller allows the closure of small to medium-size defects thanks to the large rotation arc on the dissected perforator. In our case donor site was partially reconstructed by using full-thickness skin graft. However, grafted zone was placed in a “fix” area where the eventual retraction will not cause any functional problem, constituted only by muscle, a favorable bed for graft healing. Moreover the scar resulted by the graft was placed in a more hidden zone (proximal and not distal).
We believe that this technique allows a better flexor tendons coverage compared to STSG. Furthermore, the large rotation arc of propeller flap, compared to advancement consents to minimize tension at the reconstructed site.
Conclusion
The use of the fasciocutaneous propeller flap based on a perforating branch of the ulnar artery to repair small or medium-size defects offers a consistent tendons and nerves protection, a better quality of scar and avoids the reduction of wrist mobility,resulting in a better aesthetic and functional result (Figure 3).

Figure 1: RFFF harvested resulting in a 6.5 × 4.5cmdefect on the distal portion of the wrist.
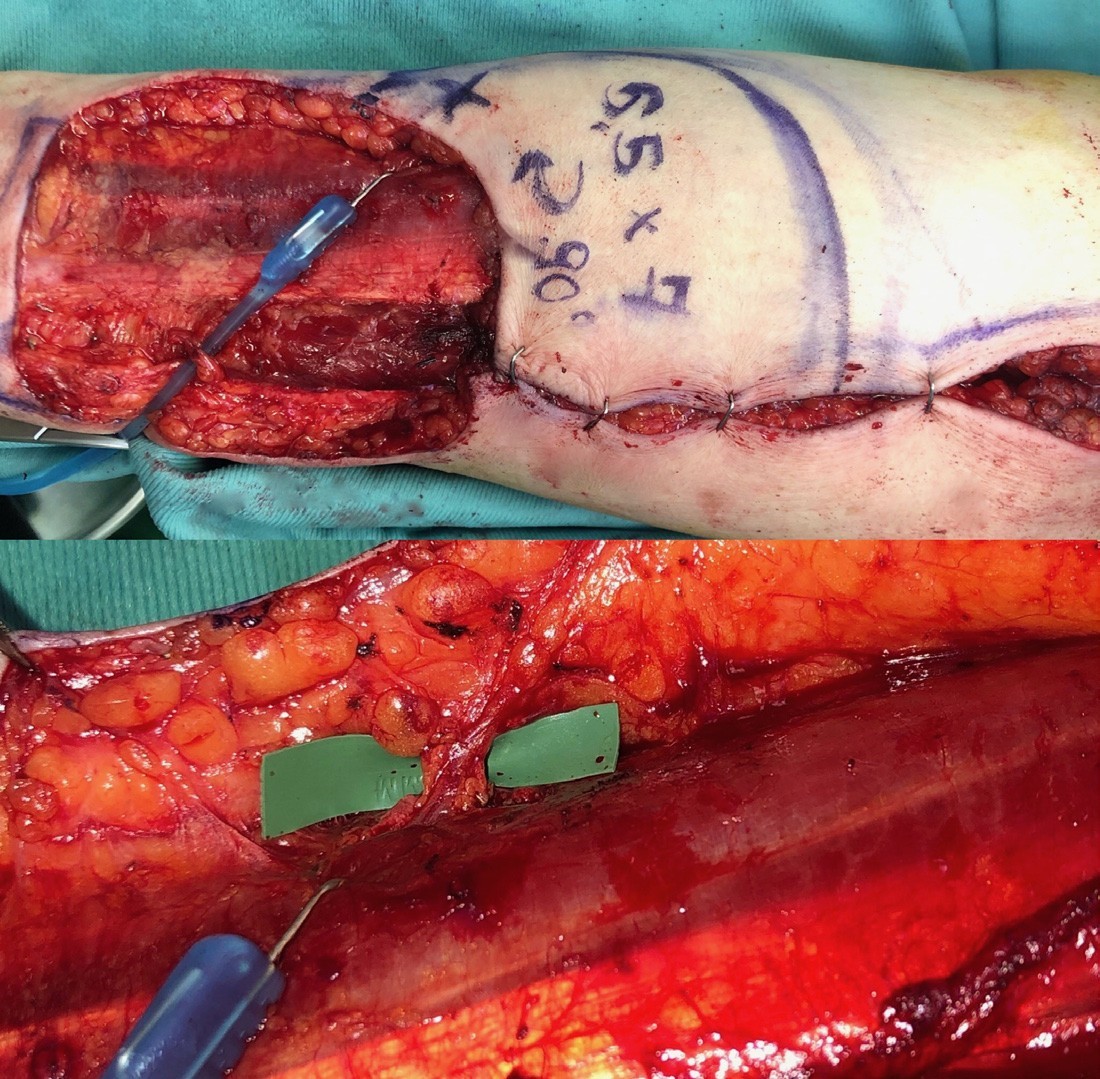
Figure 2a: Fasciocutaneous propeller flap design. “X”: marking point based on the pulsatile pitched signal detection. 2b: Ulnar perforator.

Figure 3:Fasciocutaneous propeller flap was rotated (90°). A full- thickness skin graft was used to repair the proximal area (1.5 × 2.5).
Timmons MJ, Missotten FE, Poole MD, Davies DM (1986) Complica- tions of radial forearm flap donor sites. Br J PlastSurg 39: 176-178.
Brown MT, Couch ME, Huchton DM (1999) Assessment of donor-site functional morbidity from radial forearm fasciocutaneous free flap har- vest.Arch Otolaryngol Head Neck Surg 125:1371-1374.
Kerawala CJ and Martin IC (2006) Sensory deficit in the donor hand after harvest of radial forearm free flaps. Br J Oral MaxillofacSurg 44:100-102.
Sardesai MG, Fung K, Yoo JH, Bakker H (2008) Donor-site morbidity following radial forearm free tissue transfer in head and neck surgery. J Otolaryngol Head NeckSurg 37:411-416.
Elliot D, Bardsley AF, Batchelor AG, Soutar DS (1988) Direct closure of the radial forearm flap donor defect. Br J PlastSurg 41:358-360.
Potet P, De Bonnecaze G, Chabrillac E, Dupret-Bories A, Vergez S, Chaput B (2020) Closure of radial forearm free flap donor site: A comparative study between keystone flap and skin graft. Head Neck 42:217-223.
Hsieh C-H, Kuo Y-R, Yao S-F, Liang C-C, Jeng S-F (2004) Primary clo- sure of radial forearm flap donor defects with a bilobed flap based on the fasciocutaneous perforator of the ulnar artery. PlastReconstrSurg 113:1355-1360.
Shoaib T, Van Niekerk WJ, Morley S, Ellabban MA, Soutar DS (2009) The ulnar artery perforator based islanded V-Y flap closure of the ra- dial forearm flap donor site. J PlastReconstrAesthetSurg 62:421-423.
Jaquet Y (2012) Radial forearm free flap donor site morbidity ulnar- based transposition flap vs Split-thickness skin graft. Arch Otolaryngol Head Neck Surg 138:38-43.
Foissac R, Benatar M, Dassonville O, Bozec A, Poissonnet G, Camu- zard O (2017) Coverage of tendon exposure after radial forearm free flap by the Dorsoulnar artery perforator flap. OtolaryngolHead Neck Surg 156:822-827.
Citation: Mangialardi ML, Vitagliano S, Salgarello M(2020) The Fasciocutaneous Propeller Flap Based on a Perforating Branch of the Ulnar Artery to Repair Radial Forearm Free Flap donor Site : A Case Report. J Surg Insights: JSI-100013