Current Updates in Dermatological Problems
Interaction between Dimethylpolysiloxane and Autologous Plasma Triggering in Vitro Inflammation in Cultured PBMC
Harlim A1*, Mujadid F2 and Wibowo H3
1*Departement of Dermatovenereology, Christian University of Indonesia, Gajah mada 193A, Jakarta 1120, Indonesia
2PT Kimia Farma (persero), Tbk. Jakarta, Indonesia
3Departement of Parasitology and Research Laboratory, University of Indonesia, Jakarta, Indonesia
*Corresponding author: Harlim A, Departement of Dermato and Venereology, Christian University of Indonesia, Indonesia. Tel: +62816854083.
Citation: Harlim A, Mujadid F, Wibowo H (2018) Interaction Between Dimethylpolysiloxane and Autologous Plasma Triggering in Vitro Inflammation in Cultured PBMC. Curr Updates Dermatol Probl: CUDP-100001.
Received Date: 30 October, 2018; Accepted Date: 12 November, 2018; Published Date: 06 December, 2018
1. Abstract
The data obtained from this study try to explain the mechanism of cellular immune response of dmps-injected recipients with in vitro-based method to get the description of immune responses that occurs in the body due to exposure to dmps which can lead to granuloma formation, followed by fibrosis. pbmc is taken from normal patients and patients with granulomas due to injection of dmps. And then, it was cultured for 72 hours with rpmi treatment as a negative control, pha and lpsas a positive control, dmps only and dmps with the addition of autologous plasma. The purpose of the pbmc culture was to describe the activity of tnf-a, ifn-γ, il-6, il13, il-10 and pbmc proliferation. There was no significant increase (p> 0.05) in proliferation of lymphocytes and monocytes in the dmps-treated group, both in normal patients and patients with granulomas. The role of autologous plasma was not observed in increasing cell proliferation. Nonetheless, autologous plasma had a role in increasing activity of tnf-a and il-6 significantly (p <0.05) in response to dmps exposure in both of patients. The data of this study indicated that dmps was able to trigger non specific inflammatory activity mediated by tnf-a and il-6 and it depended on each individual plasma proteins. Specific cellular immune response due to dmps exposure, as lymphocyte and monocyte proliferation, was not observed.
2. Keywords: DMPS; Lymphocyte; Monocyte; TNF-a; IL-6; PBMC
3. Introduction
Dimethylpolysiloxane (DMPS) or better known as liquid silicone is a synthetic polymer that contains silicone element and was introduced in the UK in early 1900. DMPS was used as a cosmetic ingredient and filling material in body reconstruction, based on its special chemical physical properties. As a filling material, DMPS has higher viscosity than water, but lower than other filling materials, and stable in a wide range of individual body temperature. Acute toxicity study of DMPS by FDA was revealed that DMPS was not toxic. Therefore, it is used widely in pharmaceutical, medical and cosmetic purposes. In addition, other biocompatible polymers, such as fat, hyaluronic acid, collagen, poly-L-lactic acid, and calcium hydroxyl apatite are not as good as DMPS [1,2].Initially, DMPS was not considered as an antigenic element, so that DMPS was recommended as a filling material and not expected to cause inflammation, but it was not entirely correct. Some cases showed that DMPS was not completely inert to biological systems. Face injection with DMPS on a few individuals cause chronic inflammation [1]. At injection site, granuloma was formed and followed by fibrosis within a period of six-month up to 28 years after the application of DMPS. In some cases, granuloma formation did not occur after injection of DMPS [2-5]. In Indonesia, The Indonesian Association of Plastic Surgeons (PERAPI) reported 249 cases of inflammation due to the use of liquid silicone in the past three years to 2009 and stated that the cases were only 15% of the total incidents [6]. Inflammation that occurs can be caused by several possibilities. First, the inflammation occurs as a result of injecting errors or contaminants contained in DMPS.1 If so, inflammation appearing after DMPS application cannot be considered as a specific result caused by DMPS exposure. Second, inflammation may be caused by silica which is the result of oxidation of DMPS in the tissue. Silica is known as a causative factor of inflammation through the activation of Nod-like receptor (NLR) in macrophages. Activation of NALP3 inflammasom due to the interaction between silica with NLR will induce the secretion of IL-1β by macrophages which is one of inflammatory mediators [7]. However, DMPS is a stable material, so the oxidation process is doubtful whether it will happen or not in the body [1]. DMPS is a polymer molecule that has the possibility to be recognized by B lymphocytes and activated through the T-independent pathway. This is supported by a research conducted by Kossovsky et al [8] who discovered the presence of antibodies with high avidity in patients with silicone breast implants, with an incidence of 1.7% of population. The antibodies caused deposition of complement proteins and initiated a inflammation through increasing of vascular permeability, histamine secretion by mast cells, and recruitment of inflammatory cells [9]. Iribarren et al [4] also showed that in vivo exposure to DMPS was able to induce macrophages to secrete Nitric Oxide (NO) which is one of the inflammation mediators. In addition, DMPS also potentially increase the expression of the receptor Vβ chain of T lymphocytes that plays a role in the incidence of cytokines storm [2]. Based on all of the data, immunogenicity status of DMPS should be reexamined. Immunogenicity of DMPS could be evaluated through both non-specific immune system and the specific immune system in the body. In vitro-approached through PBMC (Peripheral Blood Mononuclear Cells) cultured, followed by evaluation of cytokine secretion could be used to observe the cellular immune response arising from DMPS exposure. In addition, the data about PBMC proliferation, particularly lymphocytes, due to DMPS exposure could be used as a parameter to observe reactivity of specific immune system with DMPS.The role of DMPS in inflammation could be observed through the ability of this molecule to induce both non-specific and specific immune system to secrete pro-inflammatory cytokines, i.e. IFN-γ, TNF-α and IL-6. These cytokines play an important role in inflammation as a response to antigen exposure in the tissue. Persistence of DMPS in the tissue caused the inflammation continue until the activity of IL-10 as a regulator of inflammation appeared. At a later stage, polarization of Th lymphocyte subsets towards Th2 was regulated by IL-6 [7]. The predominance of Th2 lymphocyte subsets could be characterized by the activity of IL-13 which was also a potency indicator of DMPS for triggering fibrogenesis in tissues [10]. Thus, dynamic activity of these cytokines could represent immune responses to DMPS exposure at every stage.Beside secretion of cytokines, the dynamic of Peripheral Blood Mononuclear Cells (PBMC) population can be a parameter to determine the components of the immune system that play a role in immune response after DMPS exposure which then determine the immunogenicity of DMPS. Thus, cytokine secretion and the dynamic of PBMC population after DMPS exposure can become parameters whether inflammation is caused by the immunogenicity of DMPS and show that DMPS is a complete antigen.
4. Method
4.1. Reagents: Phosphate Buffer Saline (PBS) pH 7,2, Ficoll-paque, RPMI 1640 Gibco, Phytohaemmaglutinin (PHA) Gibco, Lipopolysaccharide (LPS) Sigma Aldrich, Dimethylpolysiloxane 1000 cs, fetal bovine serum, Acridine Orange (AO), Trypan blue, Milliplex Map Kit #MPXHCYTO-60K, and microtube 1,5 ml Axygen.
4.2. Subject: Subjects that contributed in this research were 22 women donor who had been requested approval for their blood sample as much as 6 ml. The 11 subjects have been undergoing granuloma due to DMPS injection for a case group, whereas blood samples from 11 health women with no history of DMPS injection and granulomas as a control group. Cut off point of normal silicone level, that had been conducted by Harlim (Unpublished) was less than 437 µg / g of tissue.
4.3. PBMC Isolation and Culture: A total of 6 ml of blood subjects was collected in heparinized-tubes. PBMC isolation performed by gradient centrifugation using Ficoll at 2125 RPM, for 20 minutes and without braking. Then, cells were washed using PBS. PBMC obtained was cultured in complete medium, that contained RPMI 1640 medium, 10% Fetal Bovine Serum (FBS) and 1% penicillin-streptomycin. PBMC concentration in the culture is as much as 4x106 viable cells/ml [10, 11]. There are five treatment groups of culture, the negative control (RPMI), Positive Control Phytohaemagglutinin (PHA), positive control Lipopolysaccharide (LPS), DMPS exposure group that were cultured with complete medium (DMPS)and DMPS exposure group with the addition of 10% autologous plasma of patients that have been inactivated (DMPS+AP). Culture group was incubated at 37°C, 5% CO2 for 72 hours to observe the secretion of cytokines and lymphocyte proliferation.39 Supernatant of PBMC culture was harvested and stored at -80°C. IFN-γ, TNF-α, IL-6, IL-13 and IL-10 were measured by using Milliplex Map Kit #MPXHCYTO-60K.
4.4. Ratio of PBMC Population: Lymphocyte proliferation was observed as increasing ratio of lymphocytes to the total number of PBMC. Total number of PBMC before and after culture were calculated using Hemocytometer plate. Identification of PBMC population conducted by Acridine Orange staining technique (AO) with a concentration of 6.76 µM [12]. Observations were made using a fluorescent microscope with 495 nm wavelength. (Figure 1) Through the identification, the ratio of lymphocytes in PBMC populations for 72 hours post culture was then obtained. Total number of PBMC calculated using Trypan blue staining.
5. Result
Totally, 11 patients with granuloma due to silicone injection and 11 patients who had never been injected with silicone (normal) as the subjects of this study. Silicone level in granuloma tissue and skin was checked to ensure that the patient had received DMPS injection previously. DMPS levels of patients with granuloma were 2444.2 ± 3091.88 mg/g tissue, whereas DMPS levels of normal patients were 41.76 ± 62.65 µg/g tissue. (Figure 2) showed that the immune response against the DMPS was dominated by the ratio of TNF-α/IL-10 and IL-6/IL-10, but not by IFN-γ/IL-10. These cytokines were greatly influenced by autologous plasma components, both in normal patients and patients with granulomas. In normal patients and patients with granulomas, ratio of TNF-α/IL-10 and IL-6/IL-10 from the DMPS + AP group was higher significantly (p <0.05) than negative control and DMPS group.PBMC cultures with PHA treatment had highest levels of IL-13 both in normal patients and patients with granulomas, 71.7 ± 21.7 pg/ml and 30.4 ± 104,2 pg/ml, respectively, but did not differ significantly (p>0.05) with control negative group. The lowest levels of IL-13 wasshown in DMPS+AP group both in normal patients and patients with granulomas, 17.3 ± 1.7 pg/ml and 15.5 ± 3 pg/ml respectively, but still did not differ significantly (p> 0.05) with control negative group.(Figure 3) showed that DMPS could not induce IL-13 secretion by PBMC. In addition, there was no significant effect (p> 0.05) of autologous plasma in PBMC activity to secrete IL-13, both in normal and granuloma patients. Increasing ratio of TNF-α/IL-10 and IL-6/IL-10 as a result of DMPS exposure both in normal patients and patients with granulomas had significantly positive correlation (p <0.05) with persistency of non-specific immune system components which were dominated by monocytes (Figure 4).
6. Discussion
Dimethylpolysiloxane (DMPS) is a filling material with better biocompatibility than other molecules with the same function, such as polyurethane.2 Stability of chemical properties of DMPS makes it difficult to degrade in the tissue. In addition, DMPS was not toxic for humans. Therefore, DMPS is considered inert to the body systems, so that it is used widely in medical applications. Nonetheless, granuloma formation as a response of immune system against DMPS is found with diverse clinical onset, that DMPS is considered not fully inert [1-3]. Initial response that occurs when DMPS was injected into the body is the plasma protein adsorption which then triggers activation of the extrinsic and intrinsic coagulation system, the complement system, the fibrinolytic system, kinin system and platelets. Activation pathway of proteins adsorped on the surface of DMPS was known as Vroman effect [8]. This process generated the conditions in DMPS-injected area filled by various chemokines, cytokines, growth factors and various other substances that could modulate the immune system to trigger acute inflammation [13]. Surface of DMPS which is coated with proteins matrix then triggers infiltration of non-specific immune system components such as neutrophils, mast cells and monocytes. Monocyte attachment on DMPS surface occurs due to interaction between the β2 integrin receptor and ligands such as fibrinogen, fibronectin, IgG and complement protein, particularly C3b fragment. Integrin interaction with the ligands will initiate cytoskeleton remodeling, so adhesion of monocytes will be stronger, activate and secrete inflammatory cytokines, such as TNF-α and IL-6. Cellular immune response mediated by monocytes causes the activation of other inflammatory cells, such as neutrophils and lymphocytes, and then resulting in inflammation, synergistically [8]. In the tissue, DMPS-containing vacuoles is much bigger than the monocytes. As a result, histiocytosis occur (monocytes fusion), in order to localize and degrade DMPS. Monocyte fusion process also can occur in vitro [14]. DMPS, a stable molecule, is difficult to degrade, so monocytes attached persistently on the surface of DMPS and sustain their activity. Therefore, chronic inflammation will occur in the tissue. In this condition, shifting dominancy from Th1 in acute phase into Th2 in chronic phase occurs. Then, IL-4 and IL-13 which are products of Th2 lymphocytes interact with β1 integrin receptors on monocytes or macrophages activating these cells to become histiocytes. In addition, persistent activity of monocytes triggers oxygen and nitrogen radicalsproduction which can cause tissue necrosis around DMPS deposits [15].The observation of PBMC population using acridine orange staining showed that autologous plasma was able to maintain non-specific immune system components, which were dominated by monocytes in PBMC population. This is related to the interaction of non-specific immune system components, particularly monocytes with various plasma proteins involved in Vroman effect [8]. Moreover, the persistence of monocytes can be mediated by the activity of TNF-α that maintains monocytes in their activation state [16,17]. This process indicates that DMPS potentially causes persistency and activation of monocytes in the tissue in autologous plasma milieu.Pathological conditions in patients who have been injected with DMPS are preceded by inflammation, and followed by fibrogenesis. At acute phase, TNF-α and IL-6 have an important role [7]. TNF-α has autocrine and paracrine effect in the activation of macrophages in the inflamed tissue due to DMPS exposure, and improves the ability of macrophage to engulf DMPS (phagocytosis), whereas IL-6 triggers the recruitment of inflammatory cells, such as neutrophils to the DMPS-injected site and synthesizes acute phase of protein in the liver [7]. Korn et al [16] hypothesize that the immune system in a static condition, without any stimulus from antigen, will produce TGF-β which then induces the formation of Treg population in the periphery. When antigen is infecting the body, it will lead acute phase of proteins synthesis and inflammation begins with IL-6 induction. The activity of IL-6 then suppresses Treg differentiation and drives naive T lymphocytes to differentiate into Th17, so that inflammation occurs in the antigen penetration site.At a later stage, IL-6 will drive the inflammatory process to a chronic phase by supporting the activity of Th1 to secrete pro inflammatory cytokines, but on the other hand, IL-6 suppresses the activity of IL-12, that differentiation process of naive T lymphocyte into Th1 stops [7]. This condition will cause repetitive inflammation, but gradually, the balance of Th lymphocyte subsets activity will be shifted to Th2 lymphocyte subset.In this study, the predominant immune response due to DMPS exposure was seen in TNF-α and IL-6 activity, with highest ratio of TNF-α/IL-10 and IL-6/IL-10. The activity of both cytokines correlated with the non-specific immune system components in cultured PBMCs which was dominated by monocytes. Nevertheless, the activity of non-specific immune system seemed to be dominant in autologous plasma milieu. This suggested that the DMPS could trigger inflammatory responses, performed by non-specific immune system components in cultured PBMCs. Plasma-dependent of the non-specific immune system to trigger inflammation was proved by a significantly increasing (p<0.05) ratio of TNF-α/IL-10 and IL-6/IL-10 in DMPS group after the addition of inactivated autologous plasma (Figure 2a,2b)In normal patients, ratio of TNF-α/IL-10 and IL-6/IL-10 produced from DMPS+AP group were higher than patients with granulomas (Figure 2a,2b). It means, that IL-10 had a higher activity in patients with granulomas compared to normal patients in terms of regulating the activity of TNF-α and IL-6. This condition could be caused by differences in the characteristics of autologous plasma between normal patients and patients with granulomas. Patients with granulomas have plasma characteristics with dominant Th2 lymphocytes, such as IL-10, TGF-β, and IL-4 when entering fibrosis phase [18]. In normal patients with inflammatory plasma characteristics, inflammatory reaction is more prominent when exposed to DMPS, compared with patients with granuloma.In this study, the activity of IFN-γ by T lymphocytes was not dominant. It indicates that there is no role of T lymphocytes, particularly Th1 lymphocyte subsets through the activity of IFN-γ in inflammatory reaction due to DMPS exposure. Th lymphocyte activation may occur if the synapses between Antigen Presenting Cells (APC) with Th lymphocytes are formed and generating three signals derived from interaction of MHC class II-antigens complex with The lymphocyte receptors, costimulator signals (e.g. B7 interaction with CD28), and cytokines. Antigen can be recognized by Th lymphocytes if it is peptide antigen and its chemical complexity will determine how strong the response will be generated by the Th lymphocytes. DMPS is non-peptide polymers, so it will lead T-independent pathway [9]. Moreover, the research conducted by O’Hanlon et al [19] showed that reassembling of amino acid at CDR3 region in Th lymphocyte receptor occurred in DMPS-implanted patients. DMPS was very hydrophobic, that proteins adsorbed on its surface could be denaturated. This process would lead endogen protein to become antigenic protein due to structure changes. Dominant shifting toward Th2 subset lead to IL-13 secretion by Th2 lymphocyte. Beside its role in monocyte or macrophage fusion, IL-13 could become a marker that inflammation entered the chronic phase [8]. Data obtained from this study showed that the activity of IL-13 was seen in the DMPS group, but did not differ significantly (P<0.05) from the negative control group. Ford et al [20] revealed that IL-13 and IFN-γ were mutually synergistic in enhancing the activity of IL-6 to trigger chronic inflammation in the tissue. Nevertheless, the activity of IL-13 did not become dominant immune response to DMPS exposure. In this study, the immune response due to DMPS exposure was dominated by the activity of TNF-α and IL-6, not by IFN-γ or IL-13. In addition, there was a significant correlation (p <0.05) between the persistence of non-specific immune system components dominated by monocytes and increased level of TNF-α and IL-6 (r = 0.54 and 0.46, respectively). The data indicated the role of non-specific immune system components in dominating the cellular activity that occurred as a response to DMPS exposure, compared with lymphocytes as a specific component of the immune system. This data were in contrast with the response that occurred in the tissue. Foreign body reaction due to DMPS exposure showed monocytes and lymphocytes infiltration, and histiocytes formation in the DMPS-injected area [2]. Data of Ojo-Amaize et al [21] are also different result from ours. There was specific activity of T lymphocytes due to silicone exposure characterized by T lymphocyte proliferation. It means, that there was a possibility DMPS was able to induce specific immune response.
7. Conclusion
Immune response due to DMPS exposure was dominated by TNF-α and IL-6 activity, not by IFN-γ and IL-13. Both TNF-α and IL-6 were the result of activity of non-specific immune system components, monocyte particularly. Immune response due to DMPS exposure was induced initially by Vroman effect that occurred on DMPS surface. It means, that immune response generated on DMPS surface depended on the plasma protein profile in patients body. The activity of TNF-α and IL-6 in normal patients was higher significantly than in patients with granulomas. However the result in other cytokines was not significant. Therefore, based on the pattern of immune response, DMPS was not immunogen, but able to induce inflammation mediated by plasma protein and the activity of non-specific immune system components, particularly monocytes.
8. Acknowledgement
The Authors would like to thank the Department of Pathology, University of Indonesia, The Diagnostic and research center, University of Indonesia and the Department of Analytical Chemistry, University of Indonesia for providing research facilities needed in this study
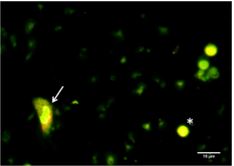
Figure 1: PBMC stained with acridine orange with 40X10 magnification. Asterix (*) sign represents lymphocyte and arrow (à) sign represent monocyte(Source: Self Documentation).
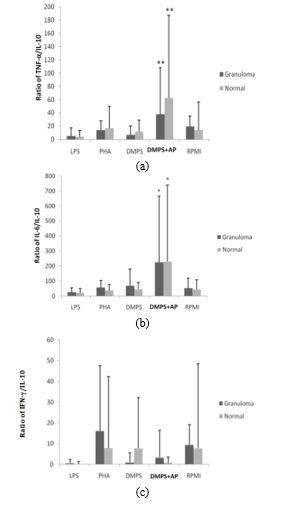
Figure 2: Ratio between pro inflammatory and anti-inflammatory cytokines. (a) Ratio between TNF-α and IL-10; (b) Ratio between IL-6 and IL-10; (c) Ratio between IFN-γ and IL-10. Asterix (*) sign represents significant differences (p<0,05) between negative control and DMPS group with other group through one-way ANOVA analysis. Double asterix (**) sign represents significant differences (p<0,05) between normal patients and patients with granuloma through independent T test.
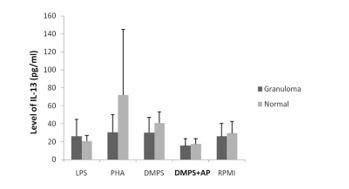
Figure 3: Level of IL-13 in PBMC cultured after 72 hours incubation in LPS, PHA, DMPS, DMPS+AP and negative control (RPMI).
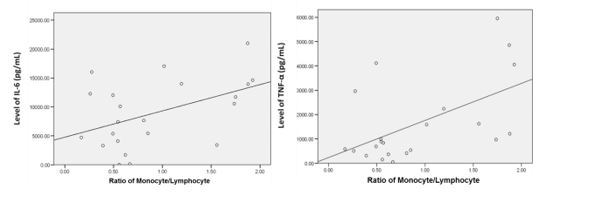
Figure 4: Correlation of monocyte ratio in PBMC population after 72 hours incubation and the level of TNF-α and IL-6 (r= 0.54 and r= 0.46, respectively).
Citation: Harlim A, Mujadid F, Wibowo H (2018) Interaction Between Dimethylpolysiloxane and Autologous Plasma Triggering in Vitro Inflammation in Cultured PBMC. Curr Updates Dermatol Probl: CUDP-100001.