Annals of Medical & Surgical Case Reports
ISSN 2652-4414
Volume 02; Issue 03
Case Report
Pyoderma Gangrenosum with Renal Failure : A Case Report
Laamari K*, Elloudi S, Mrabat S, Douhi Z, Baybay H and Mernissi FZ
Departement of Dermatology, University Hospital Hassan II, Fes, Morocco
*Corresponding author: Kaoutar Laamari, Departement of Dermatology, University Hospital Hassan II,Fes, Morocco.
Citation: Laamari K, Elloudi S, Mrabat S, Douhi Z, Baybay H, et al. (2020) Pyoderma Gangrenosum with Renal Failure : A Case Report. Ann Med &Surg Case Rep: AMSCR-100048
Received date: 13 March, 2020; Accepted date: 18 March, 2020; Published date: 25 March, 2020
Abstract
Pyoderma gangrenosum (PG) is an ulcerative disease of the skin of unknown etiology. we report here an association with renal failure
Keywords: Autoimmune; Chronicrenal failure; Renal failure; Skin; Ulcerative disease
Introduction
Pyodermagangrenosum (PG) starts with folliculocentricpustules. The appearance of these pustules or nodules is followed by ulceration with sharply circumscribed, violaceous and necrotic pustules with raised edges. The disorder is frequently associated with various systemic diseases that include inflammatory bowel diseases, haematological disorders and rheumatological conditions. The cause remains unknown, but PG is considered to represent reactions a gainst an antigen or an autoimmune reaction. The clinical concept of PG has broadened and four variants have been described: ulcerative, pustular, bullous and vegetative. We report here an unusual form of PG with ulceration, which was associated with chronicrenal failure.
Case report
A 48-year-old woman presented with a painfulery thematouslesion of 6 months in her arms and leg. She was referred for evaluation of tender bullae and nodules on her extremities that rapidly progressed to ulcers with purulent and necrotic base and irregular and under mined borders. Lesions had been present for the previous four months and the patient also complained of fever (38º C) and abdominal pain. Hermedical history revealed a persistent anemia and renalfailure. On physicalexamination, splenomegaly and pallor of ocular mucosa were detected (Figure 1).
At admission, the patient presented with several erythematousulcers, from which bloody pus wasowing. The clinical course of each lesion was as follows: initially, the lesion consisted of a few pea-sizederythematous nodules, at the top of which bloody pus discharged through sinuses, after that, the lesions becomes ulcerative. Histology showed spindle cells and small vessel proliferation with lymphocytic infiltration consistent with PG. Unfortunetly, the patient died before the start of the treatment of renalfailure.
Discussion
Pyodermagangrenosum (PG) is an ulcerative disease of the skin of unknown etiology. The association of PG with infection, autoimmune disease, inflammatory bowel disease, malignancy, and drugs suggests a hyper sensitivity reaction. The initial hypothesis, which has not been supported by experimental data, includes an immune-complex vasculitis, T-cell activation, and altered neutrophil function. It is currently thought that cytokine dysregulation accounts for most of the clinico pathological changes seen in PG [1,2].
The skin lesions of PG may be single or multiple and chronic or recurrent. The lesions occur most commonly on the leg, especially the peritibial area, but can develop in any part of the body. The initial lesionusuallybegins as follicularerythematous papules or pustules, or inflammatory nodules. The lesionthenforms an ulcerwith a purulent base and a ragged under mined, violaceous gunmetal color border, which spread speripherally [3]. Pyodermagangrenosumwas first reported [4]. Four clinical and histological variants have been recognized: ulcerative, pustular, bullous and vegetative. Among these clinical variants, rates of progression and associated diseases, as well as histological changes, can vary considerably [5].
Biopsy of an earlylesion of PG demonstrates a dermal neutrophilicabscess. Later stage lesions show epidermal necrosis and ulceration, superficial dermaledema and a dense mixed dermal infiltration thatmayextend to panniculitis. Histological examination of the advancing, inflamed border reveals dense perivascular lymphatic inflammation, which may at times beassociated with vascular destruction. None of these histological featur esispatho gnomonic for PG. No laboratory finding is diagnostic of PG and investigations should focus on identifying associated diseases, if any and excluding lesions that may simulate PG. The frequency of misdiagnosing PG is approximately 10% [6].
Differential diagnosis should include infections, neoplasias, vasculitis, ulcers secondary to peripheral venous or arterial insufficiency and factitious dermatitis. Bacterial cultures are required to rule out infectious processes [7]. PG should be approached as a multisystemic disease frequently associated with an underlying internal disorder. PG involvement is primarily cutaneous but with potential visceral extension.
Conclusion
?e association between PG and renal failure is extremely rare. We reviewed the literature and we found few cases with acute renal failure. PG is a challenging medical condition to treat and an extensive work up is required to identify any potential underlying associated disease.
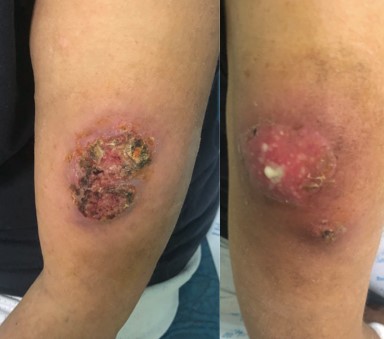
Figure 1: Ulcers with purulent surface.
Citation: Laamari K, Elloudi S, Mrabat S, Douhi Z, Baybay H, et al. (2020) Pyoderma Gangrenosum with Renal Failure : A Case Report. Ann Med &Surg Case Rep: AMSCR-100048