Annals of Medical & Surgical Case Reports
(ISSN 2652-4414)
Case Report
Challenges Associated with Caring for the Elderly Hip Fracture Patient at the Epicenter of the COVID-19 Outbreak in the United States: A Case Report
Dankert JF*1+, Lott A1+, Haskel JD1, Behery O1, Crespo A1, Ganta A1,2 and Konda SR1,2
1Department of Orthopedic Surgery, NYU Langone Health, NYU Langone Orthopedic Hospital, New York, USA
2Department of Orthopedic Surgery, Jamaica Hospital Medical Center, New York, USA
+Authors contributed equally to the production of the manuscript
*Corresponding author: John F. Dankert, Department of Orthopedic Surgery, NYU Langone Health, NYU Langone Orthopedic Hospital, New York, USA.
Citation: Dankert JF, Lott A, Haskel JD, Behery O, Crespo A, et al. (2020) Challenges Associated with Caring for the Elderly Hip Fracture Patient at the Epicenter of the COVID-19 Outbreak in the United States: A Case Report. Ann Med &Surg Case Rep: AMSCR-100057
Received date: 11 April, 2020; Accepted date: 27 April, 2020; Published date: 08 May, 2020
Abstract
The SARS-COV-2 (COVID-19) pandemic has presented orthopedic surgeons with unprecedented challenges in the care and management of patients with traumatic musculoskeletal injuries. Early intervention must be balanced with the risks these patients face during admission to a clinical environmental where others with active COVID-19 infections are receiving care. Although hospital centers have taken measures to limit intermingling of symptomatic and asymptomatic patients in the acute setting, avoiding exposure to a communicable airborne illness is a difficult endeavor given the volume of patients presenting with respiratory symptoms. We present a case report of an elderly patient who sustained a hip fracture, initially did well post-operatively, but eventually succumbed to complications related to the COVID-19 virus.
Keywords: COVID-19; Elderly patients; Intertrochanteric hip fracture; Novel 2019 SARS-COV-2; Outcomes after hip fracture repair; Pandemic; Resource management
Introduction
The first case of SARS-COV-2 (COVID-19) was confirmed in New York City on March 1st, 2020 [1]. As of April 8th, 2020, there have been 80,204 confirmed cases of COVID-19 and 4,260 death attributed to COVID-19 in New York City. Deaths have predominantly occurred in patients aged 75-years and older, but individuals in the 18-44-years old age group have also died due to complications related to the illness. The virus has a vast presentation profile with some patients reporting fever, cough, myalgias, fatigue, and shortness of breath whereas others also have gastrointestinal symptoms [2-5]. Patients also appear to have a varied reaction to the infection. Many individuals with a confirmed infection have been able to return home, remain quarantined, and return to their usual state of health after several weeks with symptomatic management. Other patients have rapidly deteriorated requiring supplemental oxygen or intubation. Mortality rates have varied between 39% and 72% for patients admitted to an intensive care unit [4]. Detecting and preventing spread of COVID-19 has been further complicated by its median incubation time of 4-5 days, extending up to 14 days, after exposure.
Efforts have been undertaken in New York City to limit the spread of the virus through “social distancing”, temporary closure of public spaces including parks, gyms, and restaurant dining areas, and businesses enacting “work-from-home” policies [6]. Despite these measures, musculoskeletal injuries have continued to occur, albeit at a decreased rate, and present a difficult challenge to the orthopedic surgeon. Not only must the orthopedic surgeon develop and enact a treatment plan for these patients, but he or she must balance the risks associated with the COVID-19 infection against immediate care for the fracture or soft tissue injury. Even if patients are not actively infected with COVID-19, admission to the hospital places them in close proximity to the virus from other patients or health care workers. The lack of a predictable hospital course and effective therapy for COVID-19 has stressed the importance of limiting patient exposure to clinical environments and decreasing admission length-of-stays [7].
Here we present a case report of an elderly patient with multiple medical comorbidities who presented to our hospital with a hip fracture. Although he did not have frank COVID-19 symptoms on presentation, he was found to be positive for the virus after his procedure and eventually succumbed to complications secondary to the viral illness. His case demonstrates the rapid progression of COVID-19 in high-risk patients and the need for multidisciplinary care for patients in this clinical environment.
Case Description
Our patient was a 95-year old male with past medical history significant for coronary artery disease with three stents, hyperlipidemia, peptic ulcer disease, peripheral neuropathy, and previously treated pulmonary tuberculosis who presented to a level one trauma hospital in Queens, New York, with left hip pain after a fall on March 23rd, 2020. At baseline, he had low functional demands; he mobilized with a rolling walker, but could not walk more than 1 block at a time without needing to rest. Imaging demonstrated a left intertrochanteric hip fracture and the orthopedic surgery team was consulted for assistance with management (Figure 1).
He had no recent fevers or chills, cough, shortness of breath, or chest pain upon presentation. Nevertheless, he was provided a surgical mask out of precaution while in the emergency department. The internal medicine team evaluated the patient in the emergency department, provided perioperative recommendations, and determined him to be medically optimized for surgical intervention. He was admitted to the orthopaedic surgery service with co-management from the internal medicine team.
On hospital day one, he underwent repair of his left intertrochanteric hip fracture with a short cephalomedullary nail without complication (Figure 2).
He initially did well post-operatively and was working towards discharge to a subacute rehabilitation facility. However, his progress was hampered by intermittent asymptomatic hypotension and urinary retention. On hospital day three, his vital signs signed triggered a sepsis alert. Pertinent laboratory values at the time included a white blood cell count of 5.6 K/µL with 81.7% neutrophils and 13.9% lymphocytes, hemoglobin of 11.6 g/dL, platelets of 75 K/µL, lactate of 1.1 mmol/L, D-dimer of 3350 ng/mL, C-reactive protein of 20.6 mg/dL, ferritin of 553 ng/mL, and procalcitonin of 0.10 ng/mL. A chest radiograph demonstrated diffusely increased lung markings concerning for bilateral pneumonia not seen on his pre-operative imaging (Figure 3).
Follow-up computerized tomography imaging of his chest revealed “ground-glass” infiltration in his bilateral lungs(Figure 4).
His only symptom at the time was a new cough and intermittent mental status changes without any recorded fever. He was transferred to an isolation room on the internal medicine service and a COVID-19 nasopharyngeal screening test was obtained. Over the next day, he developed increased oxygen needs and he was provided supplemental oxygen through a non-rebreather mask. His COVID-19 test came back positive on hospital day four. He was started on hydroxychloroquine therapy, but azithromycin was held due to an elevated QTc on his electrocardiogram. His clinical status continued to worsen and through discussions with the patient and his son, the decision was made to continue comfort care and not attempt any invasive resuscitation. He expired on hospital day six.
Discussion
The COVID-19 pandemic has created unique challenges when caring for geriatric trauma patients. This case of a geriatric hip fracture patient who developed COVID-19 and subsequently died highlights several of the issues that orthopedic surgeons are encountering when caring for this already at-risk population.
As many cases of COVID-19 are asymptomatic, it has been difficult to identify cases given the lack of universal testing in the United States. Currently, only patients with symptoms or known exposure are being tested (family members of patients with known COVID-19 or health care workers with known exposures). Furthermore, as blood, sputum, feces, urine, and nasal samples all demonstrate different positive testing rates, even patients with negative test results may have the virus regardless if they are experiencing symptoms consistent with COVID-19 [8,9]. As these asymptomatic patients may not be isolated when they enter the health care system given their lack of symptoms, they are at high risk for transmitting the disease. Anecdotally, at our institution, patients with continued symptoms, cough and/or fever, are being tested repeatedly to confirm that a patient is truly negative while beginning empiric treatment at the time of symptoms. The question of whether to test/isolate all patients that require admission to the hospital such as hip fracture patients for COVID-19 remains, particularly for high risk patients in cities with high case reports.
A large factor in preventing the spread of COVID-19 is the use of adequate precautions by both hospital staff members and patients. Patients under investigation (PUI) or tested positive for COVID-19 should be placed in negative pressure rooms and wear a mask. In addition, hospital staff should wear protective equipment consisting of N95 masks, gowns, and eye protection. These measures prevent the spread of the virus, but are often not always available. For example, as hospital systems are at capacity with patients, there is not always room for patients to be properly isolated especially in the emergency room setting. These areas are often open and do not have the capacity to provide negative pressure isolation rooms for each patient. In the case of this particular patient, as he was afebrile and was not experiencing symptoms at the time of admission, he was not placed in isolation and spent several hours in the communal emergency room prior to being admitted to the floor. Furthermore, in this institution, the surgical floor rooms are double occupancy rooms. With this case, it is unclear if the patient presented to the hospital as an asymptomatic carrier or if he was exposed to the virus while hospitalized.
The use of anesthesia and intubation has been a topic of discussion in the treatment of patients with COVID-19 or PUI COVID-19. It is known that patients with COVID-19 who require intubation often have prolonged ICU stays requiring mechanical ventilation for weeks. However, the outcome of patients who require intubation for a surgical procedure as opposed to respiratory compromise is not known. Presently at our institution, there has been a push to avoid intubation for surgical procedures unless necessary to avoid any possible trauma to the pulmonary system. In the case of this patient, the hip fracture fixation procedure was performed with local anesthesia and sedation. This intraoperative anesthesia protocol using monitored anesthesia care and soft-tissue infiltration with local anesthesia has been used for the past year at our institution for patients with severe co-morbidities who are unable to undergo spinal or general anesthesia. Preliminary results from our institution also demonstrate a decrease early narcotic usage and increase in early ambulation which is particularly important in patients with comorbidities, such as cardiac and pulmonary issues.
Lastly, there is currently no literature on the mortality rate of hip fracture patients with COVID-19 and those that develop resultant atypical pneumonia. Pneumonia is a known complication of patients who are hospitalized with hip fractures and preventing the development of pneumonia is one of the reasons why hip fracture repair is considered an urgent procedure and should be done if the patient is medically stable within 24-48 hours of admission [10]. Furthermore, the mortality of hip fracture patients who develop post-pneumonia has been cited as 43% at 30 days compared to the roughly 10% overall 30-day mortality risk [11,12]. It is unknown if this mortality rate increases and by how much when the cause of pneumonia is COVID-19. Given the recent nature of the crisis, most of the research is anecdotal with limited formal studies. However, in a recent study of 10 fracture patients with COVID-19 infections in Wuhan, China, the authors cited a high mortality rate of 40% [13]. Furthermore, 7 out of the 10 fracture patients had a nosocomial infection, also highlighting the need strict infection-control measures. The need for large-scale research is essential to further understand outcomes of fracture patients with COVID-19 so as to better take care of these challenging patients in addition to providing patients and family members with accurate outcome information.
Conclusion
The COVID-19 pandemic has presented unique challenges to the practicing orthopedic surgeon in treating elderly patients with acute musculoskeletal injuries. In the asymptomatic patient, efforts must be taken to ensure that he or she is protected from other individuals infected with the virus. When treating patients demonstrating symptoms, the orthopedic surgeon must engage a clinical team including internal medicine, anesthesiology, infectious disease, pulmonology, palliative care, and the hospital’s ethics committee to ensure that the patient is medically optimized, surgery is scheduled in a safe and timely manner, and end-of-life care is discussed for what has proven to be an often deadly illness. We presented our patient as an example of the rapid deterioration that has often been observed in high-risk patients with a COVID-19 infection. Personal protective equipment for both the surgeon and patient, isolation rooms, multidisciplinary teams, and early discharge planning are all modalities that the orthopedic surgeon must engage to appropriately care for patients in this difficult hospital environment.



Figure 1: Radiographs of the patient’s left intertrochanteric hip fracture. (A) Anteroposterior pelvis radiograph. (B) Crosstable lateral radiograph. (C) Traction view.
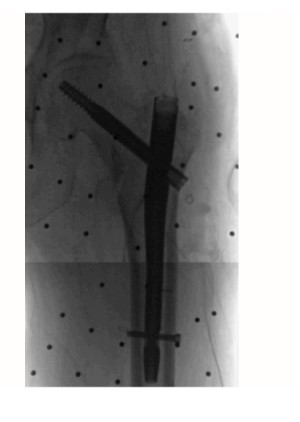
Figure 2:Stitched intra-operative fluoroscopy images after repair using a short cephalomedullary nail.
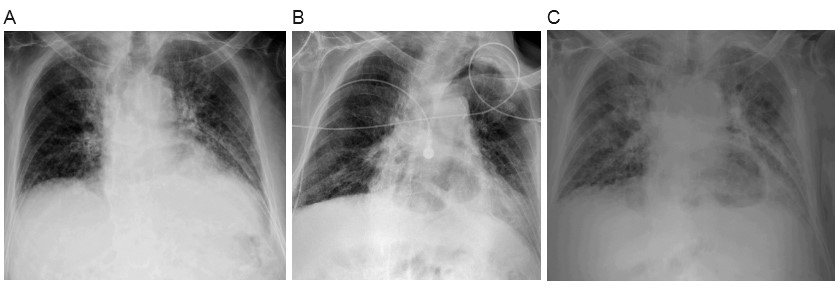
Figure 3: Sequential chest radiographs. (A) March 23rd, 2020. (B) March 25th, 2020. (C) March 26th, 2020.
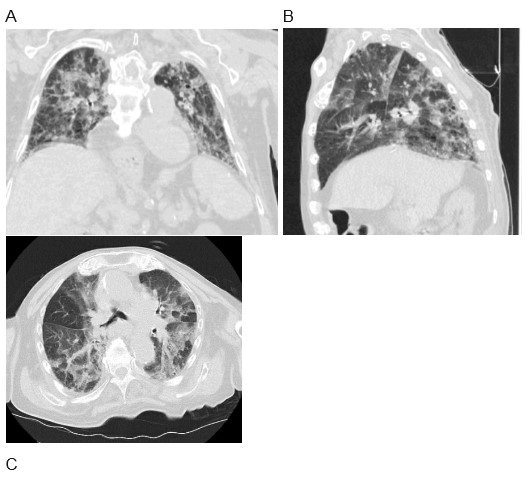
Figure 4: Computerized tomography of patient’s chest from March 26th, 2020. (A) Representative coronal view. (B) Representative sagittal view. (C) Representative axial view.
Citation: Dankert JF, Lott A, Haskel JD, Behery O, Crespo A, et al. (2020) Challenges Associated with Caring for the Elderly Hip Fracture Patient at the Epicenter of the COVID-19 Outbreak in the United States: A Case Report. Ann Med &Surg Case Rep: AMSCR-100057