Journal of Urology and Renal Problems
(ISSN 2652-4805)
Case Report
Intractable Decompression Haematuria from the Bladder; A Rare Complication and Difficult Management: A Case Report
Tourky M*
Department of Urology, Morriston Hospital, Morriston, Swansea, UK
*Corresponding author: Mohamed Tourky, Department of Urology, Morriston Hospital, Morriston, Swansea, UK.
Citation: Tourky M (2020) Intractable Decompression Haematuria from the Bladder; A Rare Complication and Difficult Management: A Case Report. J Urol Ren Probl: JURP-100007
Received date: 25 March, 2020; Accepted date: 27 March, 2020; Published date: 06 April, 2020
Abstract
Urinary retention is one of the commonest urological presentations. Chronic urinary retention is insidious in onset, high pressure chronic retention occurs with bladder volume more than 800 mls and an intravesical pressure of over 30 cm H2O, accompanied with hydronephrosis (55,56). Over the time this leads to renal failure. Acute-on chronic urinary retention occurs when the patient suddenly stops passing urine.
Keywords: Bladder; Chronic urinary; Renal failure
Introduction
The immediate management of urinary retention is urethral catheterisation to allow free drainage of urine from the bladder. Haematuria has been described following bladder drainage in 2% to 16% of high-pressure chronic urinary retention [1-3] treated by decompression and is generally self-limiting. Intractable haematuria from the bladder can be life threatening, management remains a difficult clinical problem, especially when the blood transfusion fails to keep in pace with blood loss [1].
We present a case of an 82-year-old-man who had significant haematuria, post decompression as treatment for high pressure chronic retention.
Case presentation
82-year-old Gentleman with a background of Angina admitted with Difficulty passing urine, found to be in urinary retention and acute kidney injury. He had a background of long standing obstructive urinary symptoms that have gone worse over the last few weeks. The patient was catheterised; residual volume was not recorded.
It is of note that a couple of months prior to his admission he had an ultrasound scan as a part of investigations for lower urinary tract symptoms arranged by his GP; which showed mild bilateral hydronephrosis and post voiding residual volume of 1274 mls (Figure 1).
His kidney function on admission was deranged; with a creatinine of 365 μmol/L; which improved consequently on catheterisation (Figure 1) Subsequent visible haematuria with clots developed. Ultrasound scan confirmed mild bilateral hydronephrosis and shadows were seen within the bladder suggestive of clots (Figure 2). The patient was transferred to a central hospital within the same trust for monitoring. His haemoglobin dropped significantly, down to 6.2 g/dL, with the persistent haematuria despite continuous bladder irrigation, transfused in total 30 units of RBCs and multiple fresh frozen plasma transfusions over his admission period which lasted for just over a month (Figure 3).
(Figures 1,2) demonstrating the variation in creatinine and Haemoglobin levels respectively. After three days of continuous haematuria despite continuous bladder irrigation, compensated with blood transfusion, rigid cystoscopy and bladder washout was performed on day 4.A three-way catheter was left in the bladder and bladder irrigation was restarted.
On day 6 another rigid cystoscopy and bladder washout with cystodiathermy took place with no significant control of haematuria. At 0500 am on day 7, a CT scan was performed with no unexpected findings; confirming clots in the bladder with bilateral mild hydronephrosis and no renal source of bleeding was identified. Hence, an Aortogram was performed followed by right internal iliac artery embolisation (Figure 3).
Haematuria persisted despite right internal iliac emoblisation. On day 8, open cystostomy with bladder packing and urinary diversion with bilateral nephrostomies and bilateral ureteric stents was done. On day 10, repacking of the bladder, insertion of a drain into the bladder was performed. On day 11, left internal iliac artery emobolisation was done in order to control the ongoing haematuria (Figure 4).
Bladder Packing was removed under general anaesthetic three days later. A cystogram on day 31 showed leakage from the bladder base. Drain was taken out 5 days later and patient was discharged with a stable Haemoglobin and kidney function; Hb 10.8 g/dL and creatinine 115 μmol/L. A cystogram was performed on day 42 showing no leakage from the bladder (Figure 6).
Discussion
After decompression of the obstructed urinary bladder, haematuria, hypotension, and post obstructive diuresis may occur but these complications are rarely clinically significant [3]. After quick, complete relief of lower urinary tract obstruction, haematuria occurs in 2 to 16% of patients; however, clinically significant haematuria is rare [3] and haematuria is usually self limiting. Traditionally gradual decompression was employed to reduce the risk of haematuria, Use of an IV giving set to achieve gradual decompression has also been advocated [6], it was proven, on a controlled randomised trial, that there is no statistically significant difference between gradual and rapid emptying of the bladder for urinary retention [2].
Several treatments have been suggested for intractable haematuria; Intravesical alum irrigation;
Several treatments have been suggested for intractable haematuria; intravesical alum irrigation; intravesical formalin; hydrostatic pressure; embolisation; hyperbaric oxygen for radiation cystitis; Sodium pentosanpolysulphate for chronic gross haematuria [5]. Urinary diversion was also suggested to control haematuria.
Severe “Decompression haematuria” requiring blood transfusion, despite being a very rare complication, is a life threatening complication that can be very difficult to manage. Early identification of at risk patients and evacuating the bladder of clots is essential to control further bleeding. Embolization has a significant role in controlling intractable haematuria.
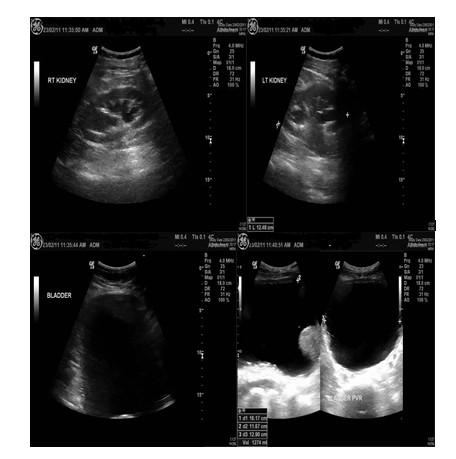
Figure 1: Pre admission Ultrasound scan showing bilateral mild hydronephrosis and large post voiding residual volume.
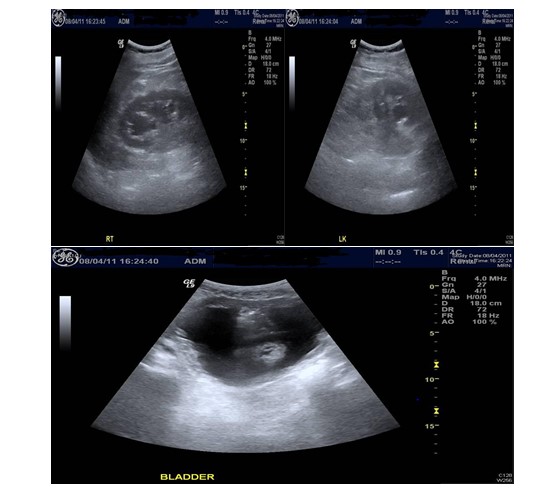
Figure 2: Ultrasound scan on admission shows bilateral hydronephrosis and shadows within the bladder suggestive of bladder clots.
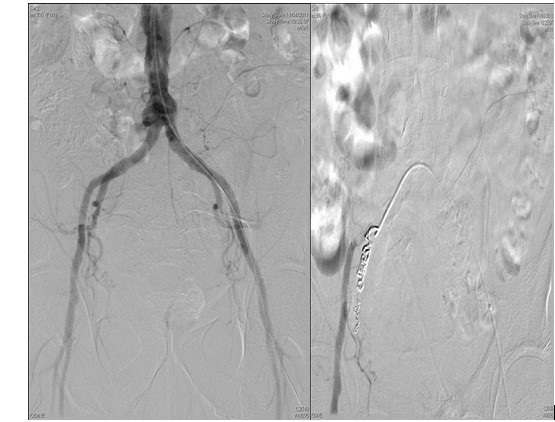
Figure 3: Aortogram followed by right internal iliac artery embolization.
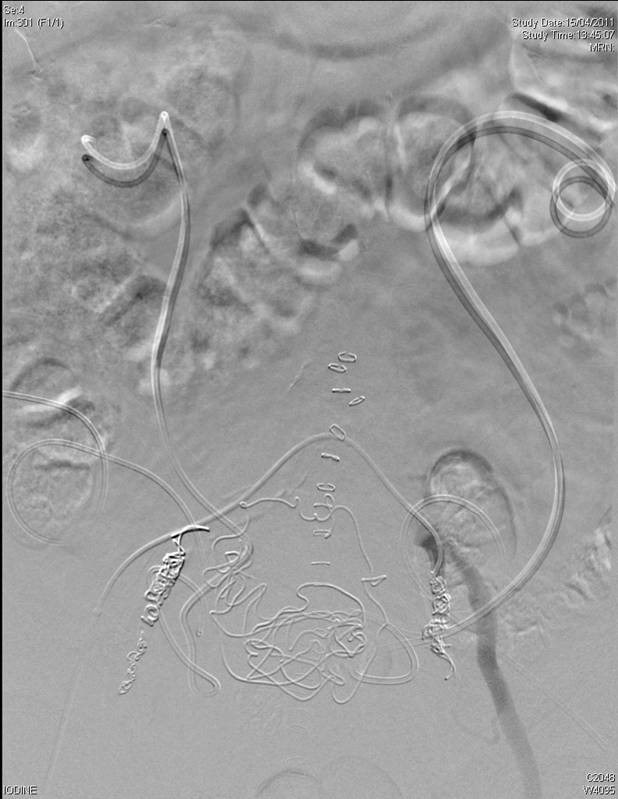
Figure 5: Left internal iliac artery embolization.

Figure 6: A cystogram showing no leakage form the bladder.
Citation: Tourky M (2020) Intractable Decompression Haematuria from the Bladder; A Rare Complication and Difficult Management: A Case Report. J Urol Ren Probl: JURP-100007