Emergency Medicine and Trauma Care Journal
(ISSN 2652-4422)
Research Article
Epidural Cervical Anesthesia for Orthopedic Upper Limb Surgeries. A Pilot Study with 10 Patients
Imbelloni LE1*, Miranda M2, Soares ARA3, Pistarino MA4 and Morais Filho GB5
1Anesthesiologist of Hospital Clínicas Municipal de São Bernardo do Campo, Brazil
2Anesthesiology of Hospital Clínicas Municipal de São Bernardo do Campo, Brazil
3Resident in Anesthesiology of Hospital Clínicas Municipal de São Bernardo do Campo, Brazil
4Resident in Anesthesiology of Hospital Clínicas Municipal de São Bernardo do Campo, Brazil
5Master in Labour Economics, UFPB, Statistician of the Complexo Hospitalar Mangabeira, João Pessoa-PB, Brazil
*Correspondening author: Luiz Eduardo Imbelloni, Anesthesiologist of Hospital Clínicas Municipal de São Bernardo do Campo, Brazil.
Citation: Imbelloni LE, Miranda M, Soares ARA, Pistarino MA, de Morais Filho GB (2020) Epidural Cervical Anesthesia for Orthopedic Upper Limb Surgeries. A Pilot Study with 10 Patients. Emerg Med Trauma. EMTCJ-100033.
Received date: 24 March, 2020; Accepted date: 26 March, 2020; Publication date:31 March, 2020
Abstract
Background: Cervical epidural anesthesia (CEA) using local anesthetic is a well-established technique for the surgeries in the neck, chest and upper arms. The aim of the present pilot study with 10 patients was to observe the safety of continuous CEA using 2% lidocaine plus 0.5% bupivacaine for humeral and clavicle fractures.
Material and Methods: In a prospective pilot study with 10 patients, we evaluated the possibilityof performing a orthopedic upper limbs surgery under continuous cervical epidural anesthesia at C7-T1 level using association of lidocaine with bupivacaine in equal volumes and epidural catheter. Block onset time, success rate, analgesia, sensory and motor block extent, changes in hemodynamic variables, and complications were assessed.
Results: All 10 orthopedic surgery procedures were successfully performed under continuous CEA. The upper margin of sensory block was C3 in all patients. Sensory block was registered in 10 patients in the supraclavicular and axillary nerves, in 8 patients in the intercostobrachial, in 7 patients in the radial, in 6 patients in the musculocutaneous, in 4 patients in the median, in 3 patients in the ulnar and in 2 patients in the median antebrachial cutaneous. No patient had cardiocirculatory changes.
Conclusion: Use 15 mL of 2% lidocaine and 0.5% bupivacaine for CEA for humeral and clavicle fractures is safe. It provides good surgical anesthesia with lesser degree of motor blockade and no cardiovascular changes.
Keywords: Anesthetic Local;Brachial plexus; Bupivacaine;Cervical epidural block; Lidocaine; Orthopedic upper limb surgery
Introduction
Upper extremity trauma is one of the most common types of injuries seen in emergency medicine. In most services, surgeries, when indicated, are performed with brachial plexus block in its various approaches. Epidural anesthesia is one of the most versatile and extensively utilized regional anesthetic techniques. It is used not only for surgery, but also for obstetric and trauma as well as acute and chronic pain states.
Cervical epidural analgesia (CEA) is an analgesic technique, potentially useful for surgeries involving the upper body. This can be achieved by directly accessing the cervical epidural space at the cervical interspaces. First reported in 1933 [1], perioperatively, CEA has been used for carotid artery, thyroid,breast, airway, upper limb and other head and neck surgeries [2]. Recently, we selected this technique of CEA for correction of bilateral humeral fracture in order to avoid bilateral brachial plexus blockwhich would require a large volume of local anesthetic [3].
The aim of the present pilot study with 10 patients was to observe the safety of continuous CEA using 2% lidocaine plus 0.5% bupivacaine for humeral and clavicle fractures.We expected the after sensory evaluation of the various nerves of the upper limb and the degree of motor block, perform general anesthesia by the beach chair position required by the surgery.
Materials and Methods
Ten patients (6 men and 4 women) with a mean ageof 32.5±13.5 yr, undergoing humeral or clavicle surgery under CEA. The protocol was registered in Brazil platform (CAAE: 68179817.8.0000.5186). After ethical committee approval and after obtaininginformed consent from patients, this study was carriedout in SUS Hospitals. Routine laboratory investigations and electrocardiogram (EKG) were normal.
Routine continuous monitoring for (ECG, NIBP, HR, RR, SpO2) before and every five minutes after the block. Patients were sedated with intravenous fentanyl (1.0 μg/kg) and midazolam (1 mg) before blockade. Patients were in a sitting position with the head tilted forward and the spine of the C7 vertebral is identified (Figure 1).
After skin preparation and disinfection, while the patient wasin the sitting position, 2 mL of lidocaine 1% was usedfor local infiltration of the skin and subcutaneous tissuein C7 and T1 intervertebral space. An 18G Tuohy needle is inserted in the C7-T1 interspace perpendicular to the skin, and was performed using the hanging drop techniquevia midline approach and a total of 15 mL of 7.5 mL 0.5% bupivacaine and 7.5mL2% lidocaine both with epinephrine (1:200.000). After local anesthetic injection in the cervical epidural space, a catheter with was advanced 4 cm cranially into the epidural space. The number of attempts to puncture the epidural space, anesthesia latency was assessed in loss of sensation in the supraclavicular nerve, the occurrence of failures, the extent of sensory block in eight nerves of the upper limb (Figure 2)and motor block (MB) were evaluated according to the scale: 1=absence of MB, 2=almost complete MB (possible movement, but not against resistance) and 3=complete MB (no movement) at 20 minutes. In reason with the beach chair position, was associated general anesthesia using tracheal intubation, after propofol (1-3 mg/kg), fentanyl (1μg/kg), 0.1 mg/kg cisatracurium and placed in mechanical ventilation and 2% sevoflurane.
Four hours after the CEA, the first dose of 5 mL solution 0.1% bupivacaine is given by catheter, followed by a new injection with the same dose every 6 hours on the 1st day postoperative. The catheter was removed on the 2ndpostoperative day. Patient did not have any complication either during surgery or in postoperative period. Post-anesthetic visits the patient did not report any painful complaint. Some data are presented as mean±SD, and others in number and between parentheses percentage.
Results
All 10 procedures were successfully performed under evaluation of CEA blocked nerves and induced general anesthesia. The demographic data of the 10 patients are shown in Table I. The success in CEA localization with needle 18G at the first attempt occurred in all of the patients.
The median of the onset of sensory block in loss of sensation in the supraclavicular nerve was 2:05 minutes. The median time of duration of surgery was 2:26 hours.The duration of the average analgesia of the first dose was 3:44 hours(Table II).
The upper margin of sensory block was assessed in C3 dermatome in all patients, and the minimal extent was T2. In all patients, the sensory fibers of cervical and brachial plexus were completely anesthetized. (Table III).
Motor block by Bromage modified range for upper limb at 20 minutes was level 1 in 5 (50%) and level 2 in 5 (5%). The level 3 was not observed in any patients. Bilateral partial motor block of the upper extremities was noted in all patients in the same evaluation as the operated limb (decreased mobility of fingers, wrist, and forearm).
At 20 minutes no patient presented Horner’s syndrome, dysphonia and none patient experienced difficulty with breathing. At this time all patients received general anesthesia. No patient had cardio circulatory changes (bradycardia or hypotension). There was no case of dura mater puncture or blood observed in the catheter.
After the end of the surgical procedure and after extubation no patient had Horner’s syndrome or respiratory distress. All patients were followed for 30 days’ follow-up and no local or systemic complications were observed. Regarding the technique used, all patients were satisfied.
Discussion
Our observations in the pilot study indicate that surgery on upper limb can be performed under continuous CEA in the beach chair position associated with general superficial anesthesia, without cardio circulatory and respiratory changes.CEA is a relatively rarely used alternative for surgery involving the upper limbs.
Recently we have demonstrated a case of bilateral humeral fracture undergoing surgical treatment under continuous CEA. In the case report we performed the CEA with 2% lidocaine associated with 0.5% bupivacaine, without occurrence of hypotension and bradycardia[3]. The association with general anesthesia under laryngeal mask is justified by the position of the patient and the possibility of long-term surgery. Administration of a local anesthetic (with or without opioid) into the cervical epidural space results in anesthesia of the cervical plexus (C1-C4), brachial plexus (C5-T1), phrenic nerve (C3-C5) and superior thoracic dermatomes. In all 10 patients, there was no phrenic nerve block clinically assessed after extubation.
At the cervical level, two methods are commonly used to confirm entry into the epidural space. The loss of resistance method relies on detection of the ability to inject solution as the needle tip penetrates the ligamentum flavum or the hanging drop technique relies on the sub atmospheric epidural pressure to draw solution into the needle hub [4]. For access the cervical epidural space we preferthe hanging drop technique.
CEA produced high-quality anesthesia and excellent postoperative analgesia in dermatomes from C2 to T8 and has a favorable effect on hemodynamic parameters due to cardiac sympathetic blockade resulting in a prolonged coronary perfusion time and reduced left-heart after load[5].
Because innervation of the arm comes from different nerves, the extent of blockade is best assessed by evaluating functions unique to each terminal nerve. Each region of the eight nerves was evaluated resulting in complete block in 10 patients in the supraclavicular and axillary nerves, in 8 patients in the intercostobrachial, in 7 patients in the radial, in 6 patients in the musculocutaneous, in 4 patients in the median, in 3 patients in the ulnar and in 2 patients in the median antebrachial cutaneous. The objective of the study was not to evaluate thoracic dermatomes for analgesia.
Cervical epidural anesthesia results in blockade of the cardiac sympathetic fibers and consequently mildly decreases heart rate, cardiac output and myocardial contractility. The mean blood pressure is unchanged or decreased, depending on the peripheral systemic vascular changes.Despite the association of continuous CEA and general anesthesia, no cardio circulatory or respiratory complications were observed within 24 hours of catheter use.
In a prospective, randomized fashion, 81 patients were selected to compare the efficacy and safety of local anesthetic under CEA using 10 mL of lidocaine (1%), bupivacaine (0.25%) and ropivacaine (0.5%) for thyroid surgery [6]. The lignocaine group required significantly more epidural top-ups compared with the other two groups. Most studies have successfully conducted surgeries under CEA using 10–15 mL of local anesthetic volumes. In view of the fact that orthopedic surgery requires greater muscle relaxation for the surgical procedure, 7.5 mL of 2% lidocaine was associated with 7.5 mL 0.5% bupivacaine both with epinephrine in a volume of 15 mL, without occurrence of hypotension and bradycardia. Use of higher concentrations of bupivacaine 0.5% or lignocaine 2% with dose of >15 mL results in excessive bradycardia and hypotension [7].The association with general anesthesia is justified by the position of the patient and the possibility of long-term surgery.
In a retrospective analysis of 394 patients, Dural puncture occurred in 2 (0.5%) and epidural venous puncture in 6 (1.5%) cases [6]. In another study, the authors reported migration of local anesthetic solution into subarachnoid space in 6 (2.8%), failed epidural puncture in 3 (1.4%), and blood observed in the epidural catheter in 4 patients (1.8%) [2]. Despite our pilot study in 10 patients, we did not observe any of the complications reported by the two articles for carotid artery surgery [7,8]. Bilateral partial phrenic nerve block is also a possible complication of CEA, a fact reported in 3 patients (0.8%) [7], complication not observed in the first 24 hours in our continuous CEA study for orthopedic surgery.
Regional anesthesia has a wide area of choices, especially when selecting the surgical procedure to be performed, either elective or emergency. The best position for puncture CEA is sitting, his neck bent head, this allows the alignment of the vertebrae, better exposure of the processes and the intervertebral spaces. Identification of space: it can be with the technique of the hanging drop or loss of strength with saline, use of air could cause pain for the likely migration into the ventricles and make pneumocephalus [9].Applied neck surgeries, upper limbs and thoracic surgery and anesthesia, analgesia or in combination with general anesthesia, depending on the needs.The approach between the C7-T1 spinous processes has been found to have clinical application in the head, neck and upper limb orthopedic surgery.
Conclusion
In this pilot study with lidocaine plus bupivacaine for CEA associated with general anesthesia, it provides acceptable surgical anesthesia with lesser degree of motor blockade that offers the hemodynamic stability. So in the hands of an experienced anesthesiologist, CEA may be a suitable choice for upper limbs orthopedic surgery. If there is no need for the beach chair positions it can be an alternative to general anesthesia.

Figure 1:Anatomic landmarks for the Epidural Cervical Anesthesia.C7-T1, spinous processes of the seventh cervical and first thoracic vertebrae.Site of puncture (needle and catheter/entry site).
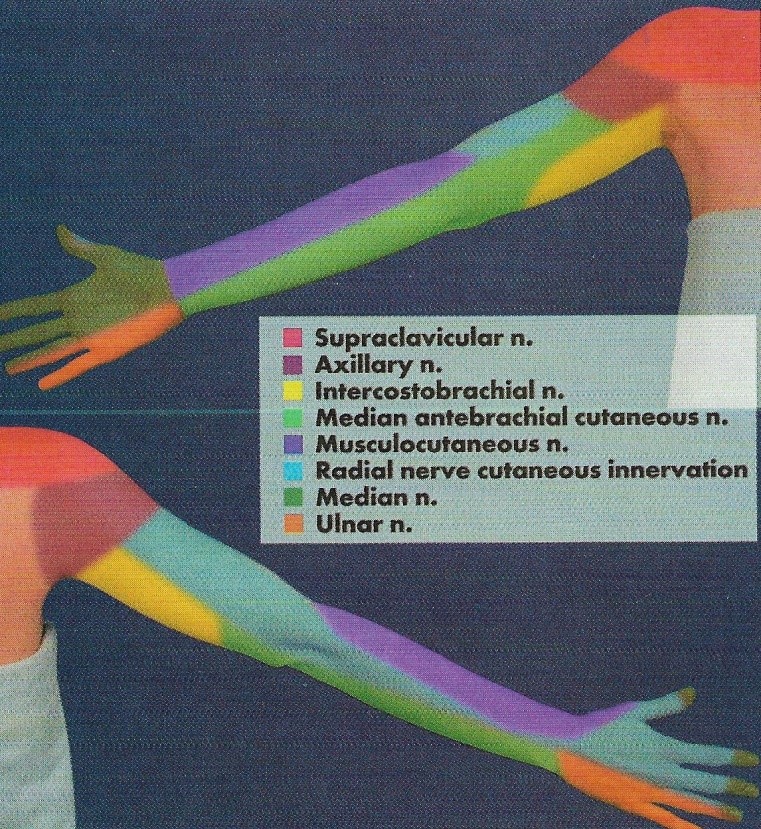
Figure 2:Peripheral nerve innervation (anterior and posterior surfaces).
|
Variables |
Results |
|
Age (years) |
32±13 |
|
Weight (kg) |
66±11 |
|
Height (cm) |
161±9 |
|
Gender: Male/Female |
6 / 4 |
|
Physical Status: ASA (I/II) |
6 / 4 |
Table I: Demographics data.
|
Variables |
Results |
|
Onset Anesthesia (min) |
2:05±0:26 |
|
Surgical Duration (hours) |
2:26±0:35 |
|
Analgesia Duration First Dose (hours) |
3:44±0:29 |
|
Failure Block |
No |
Table II: Onset Anesthesia, Surgical and Analgesic Length Failure Block.
|
Variables |
20 minutes |
|
Sensory Block |
|
|
Supraclavicular n. |
10 (100%) |
|
Axillary n. |
10 (100%) |
|
Intercostobrachial n. |
8 (80%) |
|
Median antebrachial cutaneous n. |
2 (20%) |
|
Musculocutaneous n. |
6 (60%) |
|
Radial n. |
7 (70%) |
|
Median n. |
4 (40%) |
|
Ulnar n. |
3 (30%) |
|
Motor Block |
|
|
MB 1 |
5 (50%) |
|
MB 2 |
5 (50%) |
|
MB 3 |
0 |
Table III: Effects of Cervical Epidural Anesthesia in 20 minutes.
Citation: Imbelloni LE, Miranda M, Soares ARA, Pistarino MA, de Morais Filho GB (2020) Epidural Cervical Anesthesia for Orthopedic Upper Limb Surgeries. A Pilot Study with 10 Patients. Emerg Med Trauma. EMTCJ-100033.