Journal of Surgery and Insights
(ISSN 2652-4643)
Review Article
The Moufarrege Total Posterior Pedicle or the Functional Pedicle
Moufarrege R1, El Yamani MEM2, Mansouri M2, Bouchard S2 and Alaoui AA2
1Department of Plastic Surgery, Université de Montréal, Canada
2Faculty of Medicine, Université de Montréal, Canada
*Corresponding author: Richard Moufarrege, Department of Plastic surgery, Université de Montréal, Québec, Canada, Telephone: (514) 944-6688/Fax: (514) 393-1199; Email: plasticsurg_moufar@hotmail.com
Citation: Moufarrege R, El Yamani MEM, Mansouri M, Bouchard S, Alaoui AA (2020)The Moufarrege Total Posterior Pedicle or the Functional Pedicle. J Surg Insights: JSI-100012
Received date: 21 February, 2020; Accepted date: 29 February, 2020; Published date: 06 March, 2020
Abstract
It is well known That Lifting and Reduction Mammaplasties leave, as side effects, a certain number of inconveniences among which the loss of the erogenous sensation of the nipple as well as the impairment of the breastfeeding function. The Total Posterior Pedicle created by Moufarrege allows the conservation of these functions contrary to all previously described Pedicles in the Plastic Surgery Literature.
Keywords: Breast pedicle; Functional pedicle; Lifting mammoplasty, Moufarrege Total posterior pedicle; Reduction mammoplasty; total posterior pedicle
Introduction
In the domain of reduction or lifting mammoplasty, an essential element is required for a successful surgery: the nipple-areola complex pedicle [1]. For a long time, this pedicle used to serve only as a tool to preserve the viability of the nipple and the areola. This was its sole purpose; and until now, all traditional mammoplasty techniques stick to this basic function without claiming any advantage or any goal beyond it [2-4]. This role showed a tendency to evolve in the early 1970s with the upcoming of the inferior pedicles promoted by McKissock (1971), followed by Robbins (1976) who started to include respectively 15 % and 25% of the remaining gland parenchyma in their nipple areola complex pedicle [5,6]. This was the embryo of a functional pedicle, but not more than an embryo. Since 1979, Moufarrege created his Total Posterior Pedicle using all the remaining gland as Pedicle for the nipple-areola complex: with this, the functional pedicle was born [7] (Figure 1).
Functions of the Breast
It is extremely complex to define breast functions. We list a few functions the breast can accomplish:
Breastfeeding: As mammals, the first function that comes to our mind is breastfeeding [8].
Aesthetical: Apart from breastfeeding, the human breast and especially the women breast, is a beauty attribute that plays a certain esthetical role. Even though it is not physiological, this role could be considered as one of the functions we expect the human breast to fulfill.
Sexual Role: The female breast also has a sexual role not only by the attraction it can exert on the partner but most importantly by its excitability through the nipple-areola complex, that generates erogenous sensations. This function is carried out by the 4th, 5th and 6th inter-coastal nerves [9-11] (Figure 2).
Dark green: the tree intercostal nerves responsible of erogenic sensation of the nipple entirely preserved in the total pedicle.
Light green: Subcutaneous network responsible of skin sensitivity.
Breast Vulnerability: Aside from the benefits we listed above, women breasts have a serious and preoccupying neoplastic risk, which varies in function of the breast region [12] (Figure 3).
Vascular Security: This function has traditionally been the most preoccupying concern for breast surgeons, since they decided to cease Thorek nipple-areola grafts. Often vascularization is successful, but it can yield variable outcomes. We find, depending on cases, techniques and series, that nipple losses can vary between 2 and 10% with traditional pedicle techniques [13,14].
Function in the Moufarrege Total Posterior Pedicle
Breastfeeding: Apart from certain hormonal and hereditary factors, it is fair to associate post-op breastfeeding capacity with the quantity of conserved mammary gland still attached to its ducts draining to intact nipples [15].
It is also fair to expect low breastfeeding function in pedicles made of dermis and subcutaneous tissue. In contrary, we can expect an improved breastfeeding function in techniques relying on pedicles made of secretory glands if these are connected through milk ducts to the nipple-areola complex. A good breastfeeding function is unrealistic when relying on most of superior pedicle techniques. Indeed, the small glandular mass included in these pedicles can in no way produce and drain enough milk to the nipple [15] (Figure 4).
Inferior pedicles have more chance of preserving a certain degree of lactation when compared to superior pedicles. Indeed, the McKissock technique is supposed to preserve around 15% of the remaining gland in the pedicle [6, 16]. The other 85% are sequestered here and there under the skin and cannot fulfill lactation. We can expect breastfeeding to be partially functional, relying on the 15% of remaining gland still available in the pedicle (Figure 5).
The Robbin technique provides the pedicle with almost 25% of the remaining gland. The other 75% are thus sequestered under the skin and do not contribute to breastfeeding [5, 15]. We expect, in the last case, a breastfeeding function corresponding to 25% of the remaining gland (Figure 5).
Techniques relying on narrow posterior pedicles display the same limitations as inferior pedicles, albeit these do not contain as much gland as inferior pedicles. These posterior pedicles contain mainly connective tissue and perforating arteries [17]. We cannot precisely assess the proportion of glands included in these pedicles. However, we can estimate the quantity of gland from 2 to 10%, thus we can apply the same principle of the rate of successful breastfeeding as proportional to the volume of gland included in the pedicle.
In the Moufarrège Total Posterior technique, the pedicle is constituted of all the remaining gland. No gland is sequestered without any connexion with the principal part of the gland included in the posterior pedicle(7). Moreover, the way the pedicle is shaped allows the whole remaining gland to drain milk towards the nipple in a centripetal fashion [18] (Figure 6).
We can thus consider that the conserved gland after reduction -which is fully located in the Total Posterior Pedicle- participates entirely to the breastfeeding function. This gland represents 100% of the remaining breast tissue, which explains the integrally preserved lactation capacity in the Total Posterior Pedicle (Figure 4). A retrospective study realized on nearly 1000 patients operated by Total Posterior Pedicle technique showed equal ability to breastfeed between operated and non-operated patients [18] (Figure 7).
Aesthetics: The large pedicle-gland in the Moufarrege mammoplasty is a flexible mass stemming from the same block, which, once surrounded by skin acting as an extensible elastic envelope, will form a breast that will mimic the shape of a drop of water on a vertical wall. The absence of clusters of sequestered gland here and there under skin, as one can find in all other mammary reduction techniques, prevents improper and irregular shape [19].
The gland will behave like a block of gel held by an elastic scaffold and will present a smooth and pure shape.
On the other hand, the conservation of a thickened dermic arch under the nipple will provide the breast a structure that will keep segment III from elongating. This property of the Moufarrege total posterior pedicle is very important and prevents the breast from deforming by pseudoptosis, which is an elongation of segment III and an exaggeratedly high nipple presentation associated with improper angulation (upwards instead of horizontal) [3] (Figure 8).
The Sexual Role after Total Posterior Pedicle Mammoplasty: Classically, mammary reduction automatically means loss of nipple erogenous sensation, this function depending on intercostal nerves IV, V and VI [9]. These nerves also ensure the contraction of small muscular structures in the nipple and areola. For these nerves to fulfill their nerve influx conduction role, there must be continuity of these nerves from their exit at the spinal cord to their ending at the nipple. These nerves run along the lateral thoracic muscular aponeurosis until they reach the center of the breast and dive posteriorly to anteriorly in it to the nipple (Figure 2).
Any manipulation interrupting the path of these nerves will prevent them to fulfill their function [20-22]. If one considers other techniques apart from the Total Posterior Pedicle, there is none that keeps these intercostal nerves intact (Figure 9).
Even techniques relying on inferior pedicles as the McKissock and Robbin neglect these nerves which could be partially included in inferior pedicles [2] (Figure 10).
In the Total Posterior Pedicle mammoplasty, we include in the technique the preservation of areolar tissue on the lateral aspect of the thorax on which run the three intercostal nerves IV, V et VI. Preservation of these nerves grants nipple erogenous sensation and contractility of small muscles in the nipple-areolar complex (Figure 11).
If, by any chance, areolar tissue is altered, the technique has not been performed properly. In this case, there could be a decrease in erogenous sensation at the nipples or even absence of this sensation if all three intercostal nerves are cut during the procedure, although this is a rare situation. Once these nerves are cut there is no way for them to regenerate.
However, even in traditional techniques where nipple erogenous sensation is lost, it is possible for the patient to regain sensation in the nipple and areola after a few years. This new sensation, caused by the growth of cutaneous nerves in the vicinity, is only tactile and non-erogenous. Only the continuity of intercostal nerves IV, V and VI as in the Moufarrege Total Posterior Pedicle can preserve erogenous sensation in the nipple [10].
Security of the Nipple- Areolar Complex (NAC): In a series of 10 000 mammoplasties performed with the Moufarrège Total Posterior Pedicle, there was no nipple necrosis, which is exceptional and impossible to expect in all the other mammoplasty techniques. This vascular security can be explained by the preservation of perforating arteries which feed the total pedicle and by the absence of constraints on the pedicle as in the techniques based on dermal-fatty pedicles [7] (Figure 11, 12).
The Total Posterior Pedicle as a Protection against Malignancy: In the Total Posterior Pedicle mammoplasty, most of resected tissue stems from both superior and inferior external quadrants. A very small resection is performed in the lower internal quadrant, responsible for 20% of breast cancers [23].
However, the complete resection of both superior and inferior external quadrants in the Moufarrege Total Posterior Pedicle ensures the removal of tissue with known neoplastic potential. 60% of breast cancers occur in the superior and inferior external quadrants in non-operated patients. If these two quadrants are removed, breast cancer incidence should fall drastically. A retrospective study on a cohort of 956 patients all operated by the same surgeon using the Moufarrege Total Posterior Pedicle shows a 64% decrease in breast cancer incidence in patients over 35 years [24-29] (Figure 3).
Conclusion
The Moufarrege Total Posterior Pedicle is the only known functional nipple-areola complex pedicle. There is no other mammoplasty technique in literature that allows to preserve all the previously mentioned functions except the Moufarrege Total Posterior Pedicle: security of the nipple-areola complex, preservation of breastfeeding function, preservation of erogenous sensation of the nipple, protection against cancer in a 64% proportion in patients over 35 years old. All these advantages make the Total Posterior Pedicle a FUNCTIONAL PEDICLE.
Disclosures
The authors have no conflict of interest to declare.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
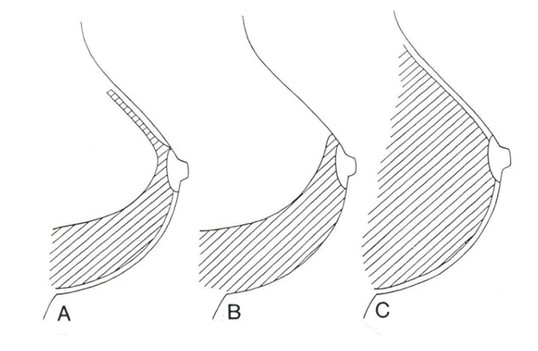
Figure 1:
A: McKissock: pedicule contains 15% of remaining gland
B: Robbins: pedicule contains 25% of remaining gland
C: Moufarrege: pedicule contains 100% of remaining gland

Figure 2: Neural network in the breast transverse section. Schematical path of nerves in the breast.
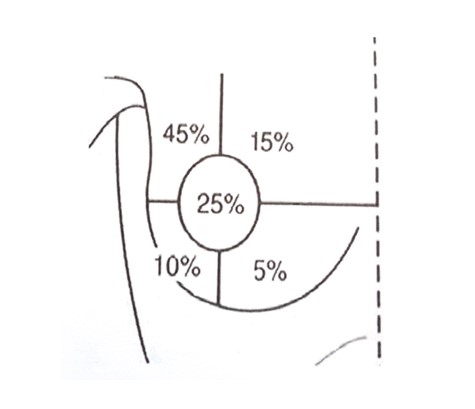
Figure 3: The percentage of incidence of breast cancer in different quadrants of the breast.
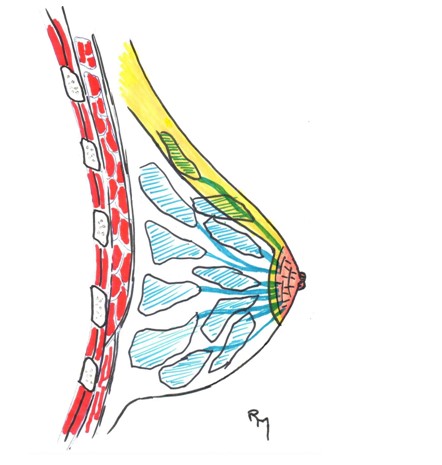
Figure 4: Galactophoric system. In upper pedicle techniques, a very poor lactogenic network is conserved.
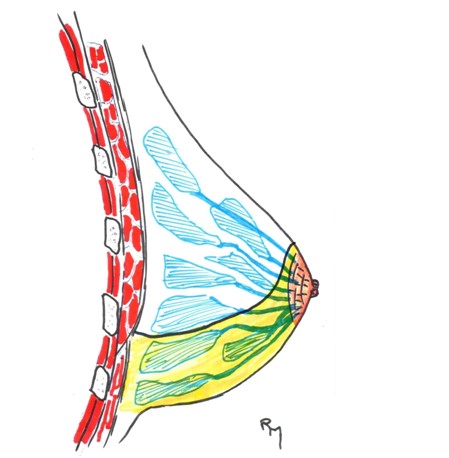
Figure 5: Lactation after reduction,sagittal section. Inferior pedicle techniques allow a few galactophoricacinis in the pedicle to drain in the NAC.
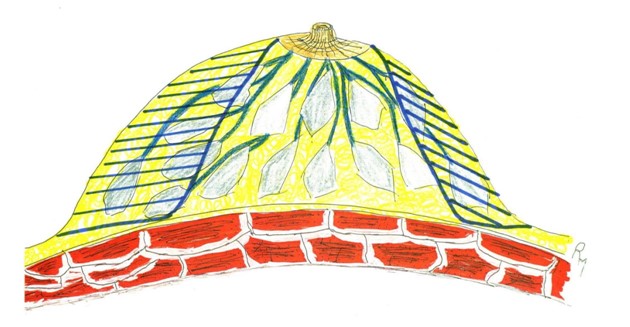
Figure 6: Galactophoric system-transverse section. All remaining gland in the total Posterior Pedicle will allow its galactophoric system to drain normally in the NAC.
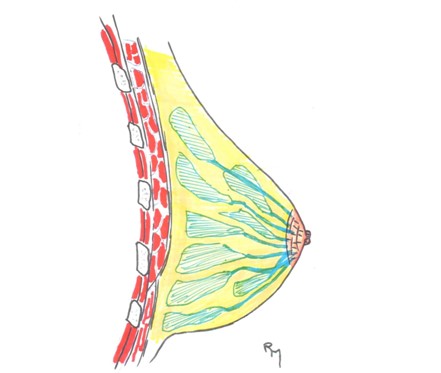
Figure 7: All galactophoric system remains in continuity with the nipple in the Moufarrege Total Posterior Pedicle.

Figure 8: Sagittal section of the reconstructed breast after reduction; note the plication of the inferior dermal tissue which will act as an inferior vault avoiding stretching and pseudo ptosis.
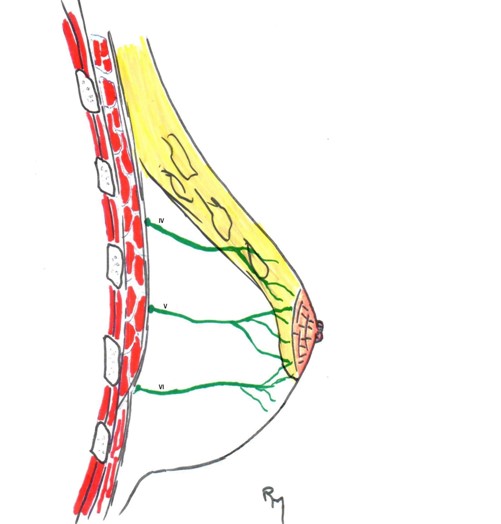
Figure 9: Superior pedicle, sagittal section;There is no chance to include any of the intercostal nerves responsible of the erogenic sensation of the nipple.
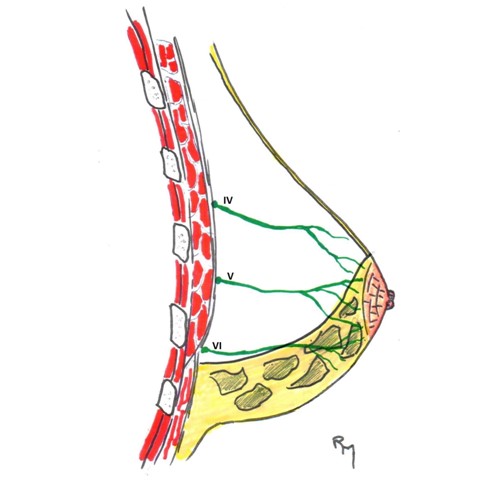
Figure 10: Inferior pedicle mammaplasies( Mckissok), sagittal section. Little chance to include one of the intercostal nerves responsable of erogenic sensation of the nipple, i.e, the VI.
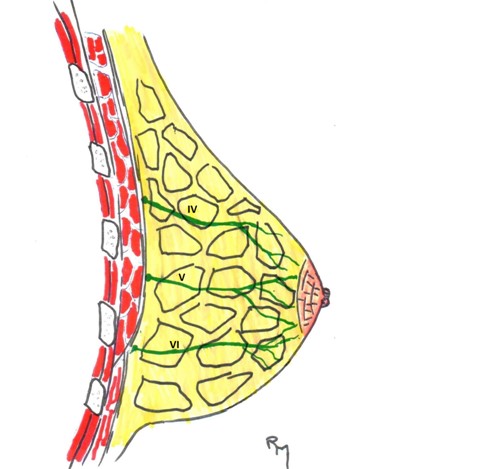
Figure 11: Total posterior pedicle, sagittal section. The three intercostal nerves IV, V, VI nerves responsable of erogenic sensation of the nipple included in the remaining.
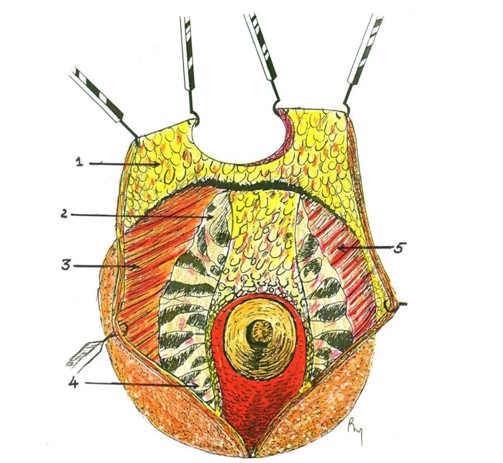
Figure 12: Frontal view after resection.
Citation: Moufarrege R, El Yamani MEM, Mansouri M, Bouchard S, Alaoui AA (2020)The Moufarrege Total Posterior Pedicle or the Functional Pedicle. J Surg Insights: JSI-100012.