Annals of Pediatrics and Child Care
(ISSN 2652-4473)
Research Article
Effects of Long Term Orthotic Intervention on Gross Motor Function in Children with Spastic Cerebral Palsy
Good friend K 1,2, Liu XC 1,3*, Zvara K 1,2, Embrey D 4, Brandsma B 4 and Tassone C1,3
1Center for Motion Analysis, Children’s Wisconsin, Medical College of Wisconsin, USA
2Department of Physical Medicine and Physical Rehabilitation, Children’s Wisconsin, Medical College of Wisconsin, USA
3Department of Orthopedic Surgery, Children’s Wisconsin, Medical College of Wisconsin, USA
4Children’s Therapy Unit at Multicare Good Samaritan Hospital, Washington, USA
*Corresponding author: Liu XC, Department of Orthopedic Surgery, Children’s Wisconsin, Medical College of Wisconsin, USA, Tel: 414-337-7323; Fax: 414-337-7337; Email: xliu@chw.org
Citation: Good friend K, Liu XC, Zvara K, Embrey D, Brandsma B, et al. (2020) Effects of LongTerm Orthotic Intervention on Gross Motor Function in Children with Spastic Cerebral Palsy. Ann Pediatr Child Care: APCC-100013
Received date: 29 February, 2020; Accepted date: 21 March, 2020; Published date: 30 March, 2020
Abstract
Effects of Long Term Orthotic Intervention on Gross Motor Function in Children with Spastic Cerebral Palsy Objective: This study aims to investigate the inter-rater reliability between two centers, and assess the impact of long term use of 3 different orthoses (SMO, HAFO, SAFO) on function using the GMFM66. Design: A cohort, case-controlled study was performed with 23 children with a GMFCS level between 1 and 4 were prescribed one of three types of orthoses by their provider (SMO, HAFO, or SAFO). GMFM was measured before and after prescription of orthotic, and after 2-year of orthotic use. Results: The Pearson correlation coefficient for the GMFM with orthoses was found to be 0.97 with a 95% CI of 0.90 to 0.99 and in the barefoot condition it was 0.96 with 95% CI of 0.86 to 0.99. When the data of both groups was combined, the Pearson correlation coefficient was 0.97 with a 95% CI of 0.92 to 0.98. The Spearman correlation coefficient was 0.95. Significant improvements in GMFM scores were noted in the SAFO orthosis (p=0.013) and SAFO Barefoot conditions (p=0.035) as well as in the HAFO barefoot condition (p=0.001). Conclusion: This study supports that, in long term follow up, SAFO and HAFO may improve biomechanical alignment during gait and functional skills for children with spastic CP.
Keywords: Gait; GMFM; Orthotic Devices; Cerebral Palsy
Abbreviations
AFO : Ankle foot orthoses
CP : Cerebral palsy
CI : Confidence Interval
HAFO : Hinged anklefoot orthoses
GMFM66 : Gross Motor Function Measure 66 Assessment
IRB : Institutional Review Board
SAFO : Solid ankle foot orthoses
SMO : Supramalleolar orthoses
Introduction
Cerebral palsy (CP) is the most common motor disability of childhood with a reported US prevalence ranging from 2-3.1 per 1000 live births [1]. These children often develop multiple orthopedic disorders of the lower extremities that make mobility a challenge. The prognosis for gross motor function is highly variable but is often accompanied by disturbances of sensation, cognition, communication, perception and/or behavior or seizure disorders [1]. Secondary to deviated gait kinematics, gait compensation of the pelvis can result in deviated spine kinematics [2]. The natural history of gait in children with CP is delayed acquisition and gradual deterioration in childhood and adolescence without intervention [3]. The goal of orthopedic providers is to maximize the child’s ability to interact with their environment utilizing the least invasive intervention. The starting point is often at the level of contracture and deformity prevention. This can be done through a variety of methods including orthopedic procedures, serial casting, medication (oral, injectable, or intrathecal), physical/occupational therapy, and orthoses. Orthoses are a conservative method employed to decrease primary impairments of inappropriate joint movements/alignment, prevent secondary impairment of contracture and to facilitate functional activity [4]. It is often used in combination with other interventions to maximize/maintain benefits.
Solid ankle foot orthoses (SAFO), hinged ankle foot orthosis (HAFO), and supramalleolar orthoses (SMO) are some of the more common orthoses used. The least restrictive, supramalleolar orthosis, captures and controls the hind foot in children with excessive pronation or supination during stance phase and improves segmental alignment. The hingedankle foot orthosis (HAFO)allows forforward movement of the tibia over the weight bearing leg during stance resulting in more natural ankle dorsiflexion. Increased dorsiflexion facilitates transitional activities such as sit to stand, floor transfers, as well as ascending/descending stairs. The solid ankle foot orthosis (SAFO) provides the most stability across the ankle. It has been shown to increase functional mobility by decreasing plantar flexion contractures and improving gait kinematics such as stride length, cadence, and energy efficiency [5, 6].
Several measures have been used to assess the impact of AFOs on gait and mobility. Gait kinematics such as step length, cadence, velocity, and joint range of motion are often measured, however, does not add up to a child's function. Although many gross motor function evaluation tools have been developed, few fulfill the requirements of reliability and validity and while still maintaining the responsiveness required to assess children with CP [1]. The Gross Motor Function Measure (GMFM66) is a standardize dassessment with demonstrated reliability, validity and responsiveness to functional changes as a result of assistive devices and/or orthoses [7, 8]. The GMFM66 is made up of66 test items grouped into 5 dimensions (A-E): A- lying and rolling (4 items); B- crawling and kneeling (10 items); C- sitting (15 items); D- standing (13 items); and E- walking, running & jumping (24 items). Using the best values from three trials, each item is scored from 0 (cannot initiate) to 3 (completes independently). Percentage scores are calculated for each group yielding scores from 0-100% [1].
Previous studies looked at the impact of orthoses on gait parameters and many demonstrated significant improvements in range of motion, kinematics and efficiency [6, 9, 10]. The impact of orthoses on function is less clear [11] studied the effect of lower extremity orthoses on function as measured by Dimension D& E of the GMFM88 in 34 ambulatory children with spastic CP. Both groups improved over the four-month testing period, but no significant difference between the group that received the orthoses intervention and physical therapy and the control group that just received physical therapy [5] assessed the effect of AFOs including SAFO,HAFO, and posterior leaf orthoses (PLFO) on kinematic and function variables in 30 children with spastic hemiplegia and found no changes in gross motor function in any of the orthotic groups. Additional studies and [12, 13] found similar results when they studied the effects of HAFO, dynamic AFOs and HAFO respectively on function. A subsequent study by, [9] found significant gains in function as assessed by Dimension E of the GMFM66 in all AFO configurations (SAFO, HAFO, PLSO) compared to the barefoot condition when they assessed 16 ambulatory children with spastic diplegia ages 4 to 11 years [14] followed 257 children with cerebral palsy and found a significant improvement in walking, running, and jumping measures. Finally, [10] found that when the gait of 10 children who used Dynamic AFOS (a thinner, less rigid AFO) and regular AFOs was compared to barefoot trials, the result was overall improve gait kinematics, stride length, and power. Overall, the majority of the studies evaluated the difference at a single session or at most over a few months and did not compare AFO and barefoot conditions. The purpose of this study was to: 1. Investigate the inter-rater reliability between two centers, using the intraclass coefficient (ICC) and correlation coefficients. 2. Assess the impact of long term use of 3 different orthoses (SMO, HAFO, SAFO) on function as measured by Dimension E of the GMFM66 over a three-year period.
Materials and Methods
A convenience sample of twenty-three children with Spastic Cerebral Palsy, mean age of 9.4 years (4.5 to 13.1) and 60.9% male were split into 3 groups: SMO, HAFO, SAFO base on the type(s) of orthoses prescribed by their primary provider. Participants were classified as having hemiplegia (n=7), diplegia (n=14), triplegia (n=1), or quadriplegia (n=1). The participants mean GMFCS level was 1.9 with a range of level 1 to level 4. Table 1 shows the distribution of AFO types, minimum, maximum and average GMFCS levels of the participants by AFO category. Patient testing occurred at one-year intervals for a period of 3 years.
Inclusion criteria included a diagnosis of spastic cerebral palsy, age between 4.5 and 18 years, ability to stand and ambulate with and without assistive device, daily use of orthoses, and ability to follow directions to complete assessments. Exclusion criteria include orthopedic, neurological/ tone reducing procedure within the past 6 months. Eligible subjects were recruited from Children’s Hospital of Wisconsin and Children’s Therapy Unit at MultiCare Good Samaritan Hospital in Washington. Informed consent was obtained from parents or guardians prior to participation and approved by the IRB of Children’s of Wisconsin and MultiCare Good Samaritan Hospital.
At each visit, participants were tested using Dimension E of the GMFM66 that included 24 motor skills with and without orthoses. During testing with orthoses, subjects were tested wearing shoes over the orthoses. During the barefoot assessment, subjects were tested barefoot with the exception of one who was allowed to wear a shoe with a lift to correct leg length discrepancy. The GMFM66 was administered using standard instructions and subjects were allowed to use assistive devices during both testing conditions. 4 children use assistive devices; anterior walkers (2), posterior walker (1) and loftstrand crutches (1). Assessments were performed on the same day for each participant, except for one child whose first assessments was completed in two sessions one week apart due to non-compliant behavior.
Data Analysis
Inter-rater reliability was measured using video recordings from Center 1 of 12 assessments with AFOs and 13 assessments without AFOs. Video recordings were score by a physical therapist at Center 2. GMFM assessments from Center 2 were scored by two physical therapists that came to consensus for each item and no video assessments were used. Pearson and Spearman coefficients were calculated to allow comparisons to reliability previously published reports. The ICC was utilized a more rigorous measure of reliability. The GMFM66 results were analyzed using a linear trend statistics, p<0.05.
Results
The Pearson correlation coefficient for the GMFM with orthoses was found to be 0.97 with a 95% CI of 0.90 to 0.99 and in the barefoot condition it was 0.96 with 95% CI of 0.86 to 0.99. The spearman correlation coefficient was found to be 0.96 in both the orthoses and barefoot groups. When the data of both groups was combined, the Pearson correlation coefficient was 0.97 with a 95% CI of 0.92 to 0.98. The Spearman correlation coefficient was 0.95. The intraclass coefficient (ICC) for the total group was 0.96 with a 95% CI of 0.92 to 0.98. Table 2 highlights our results. When looking at the linear trend across the entire three-year testing period, significant improvements in GMFM scores were noted in the SAFO orthosis (p=0.013) and SAFO Barefoot conditions (p=0.035) as well as in the HAFO barefoot condition (p=0.001), see Figures 1, 2. When a direct year 1 to year 3 comparison was assessed statistically significant improvements were again demonstrated in the SAFO orthosis (p=0.017), SAFO barefoot (p=0.017) and HAFO barefoot groups (p=0.0006).
Discussion
Ankle foot orthoses are widely used to decrease impairments and improve function [4]. There is conflicting evidence in the literature regarding if and which orthoses provide maximal functional benefit. Our findings suggest that SAFO and HAFOs provide a positive impact on functional gross motor skills for children with spastic CP. Gross motor function as measured by Dimension E of the GMFM66 improved significantly over a three-year period in the HAFO and SAFO groups. The SAFO had the largest impact; which may be due to a lower initial level of function. Smaller improvements may demonstrate more dramatic gains on the GMFM66. Interestingly, the HAFO group demonstrated significant improvement when measured in the barefoot condition. One explanation is that the orthosis created appropriate alignment, improved muscular balance and normalized movement patterns which carried over to the barefoot condition. No significant improvement was found in either of the SMO groups (Figure 3), a finding consistent with [15]. This group had higher initial levels of functioning and thus may have required larger clinical gains to see significant GMFM66 changes.
Study Limitations
There were several limitations to our study. The small sample size and even smaller group size for each category reduced the power of the study. Missing data points limited our ability to make statistical inference/conclusions from the results. The wide range in ages (4.5-13.1years) of subject may have impacted the results. Younger children are developing at a faster rate which may impact their function. Two data collection sites in combination with the ambiguity of published GMFM66 administration instructions with regards to the use of orthoses and assistive devices may have caused inconsistent scoring across subjects. The data cannot be generalized to other dimensions of the GMFM66 as only the upright functions of walking, running and jumping on Dimension E were addressed.
Future Research
Continued research into the long-term effect of orthoses on gait and function is necessary. Studying larger sample sizes or over extended periods time may provide helpful insight into the acquisition of developmental milestones and maximizing therapeutic benefit of orthoses. In our study, functional activities included in Dimension E of the GMFM66 were evaluated. All of these items required a standing start position. Clinical experience suggests that performance on floor mobility tasks while in AFOs differs compared to barefoot performance. Dimension D of the GMFM66 includes tasks with a variety of starting positions and transitional activities. Comparison of functional performance on Dimension D and E of the GMFM66 would require clinician to assess multiple types of functional activities when prescribing AFOs for children with spastic cerebral palsy.
Conclusion
For children with spastic cerebral palsy, orthotic intervention is an important management strategy. By design orthoses may restrict joint movement and specific muscle activation patterns to improve biomechanical alignment during gait and functional skills. This study adds the component of long term follow up to support the application of Solid and Hinged AFOs to improve function in ambulatory children with cerebral palsy.
Acknowledgement
We would like to thank Dr. Tarima, Ph.D, Division of Biostatistics, Medical College of Wisconsin in the support of statistical analysis and Rebecca Boerigter, MS, for manuscript editing. This work was supported by the National Institute on Disability and Rehabilitation Research (NIDRR), grant number: H133G060155.
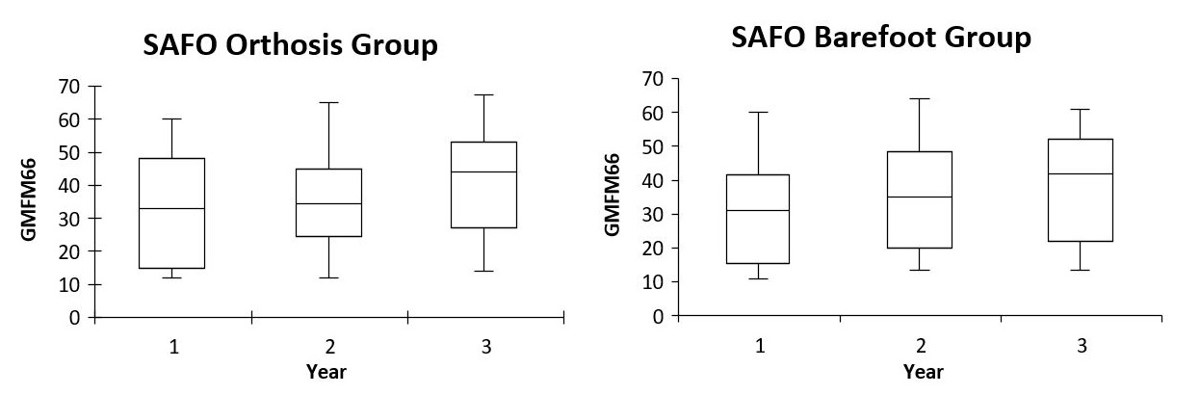
Figure 1: 3 year follow-up of GMFM66 scores for Dimension E in SAFO orthosis and barefoot groups. (significant differences between year 1 and 3, p<0.05). Charts show mean, maximum, minimum, and 95% CI.
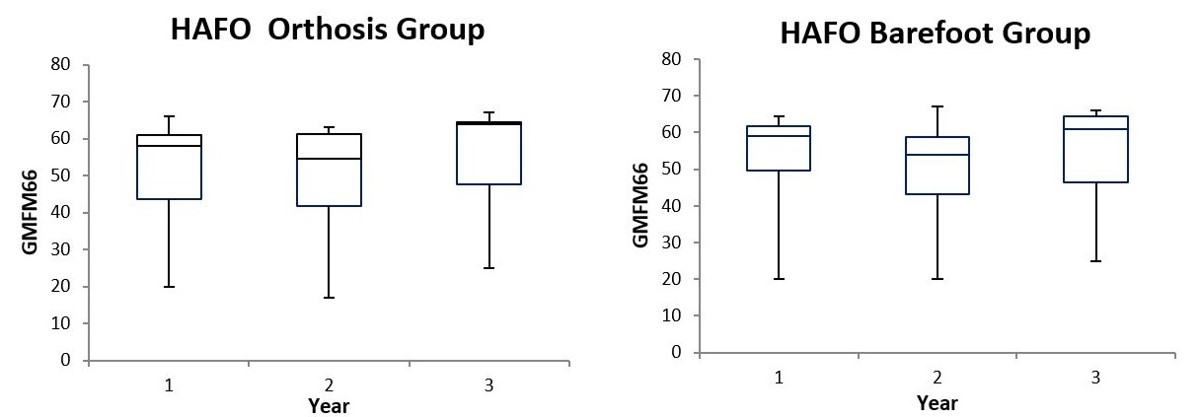
Figure 2: 3 year follow-up of GMFM66 scores for Dimension E in HAFO orthosis and barefoot groups. (significant differences for barefoot between year 1 and 3, p<0.05). Charts show mean, maximum, minimum, and 95% CI.
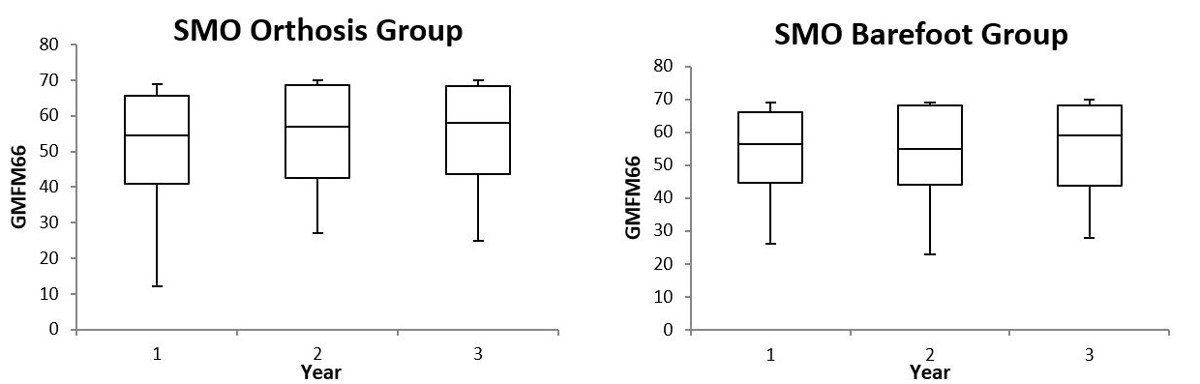
Figure 3: 3 year follow-up of GMFM66 scores for Dimension E in SMO orthosis and barefoot groups. Charts show mean, maximum, minimum, and 95% CI.
|
- |
# of Patients |
# of AFOs |
Min GMFCS |
Max GMFCS |
Mean GMFCS |
|
SMO |
9 |
12 |
1 |
3 |
1.7 |
|
SAFO |
6 |
10 |
2 |
4 |
2.8 |
|
HAFO |
9 |
16 |
1 |
4 |
1.6 |
|
Total |
24* |
38 |
1 |
4 |
1.9 |
|
Note: SMO-Supramalleolar orthosis SAFO- Solid Ankle foot orthosis HAFO- Hinged ankle foot orthosis *total of 24 is due to two types of orthoses used by one subject. |
|||||
Table 1: Orthoses Distribution and GMFCS levels.
|
SMO |
HAFO |
SAFO |
||||
|
- |
Orthosis |
Barefoot |
Orthosis |
Barefoot |
Orthosis |
Barefoot |
|
Linear Trend(p-value) |
0.602 |
0.124 |
0.222 |
0.001 |
0.013 |
0.035 |
|
Y1 to Y3(p-value) |
0.664 |
0.186 |
0.178 |
0.0006 |
0.017 |
0.017 |
Table 2: Comparison of Mean GMFM in orthotic/barefoot conditions over 3 year period (p-value).
Citation: Good friend K, Liu XC, Zvara K, Embrey D, Brandsma B, et al. (2020) Effects of LongTerm Orthotic Intervention on Gross Motor Function in Children with Spastic Cerebral Palsy. Ann Pediatr Child Care: APCC-100013