Emergency Medicine and Trauma Care Journal
(ISSN 2652-4422)
Research Article
Ghanem AN*
Faculty of Medicine, Mansoura University, Egypt
*Corresponding author: Ahmed N. GHANEM, Faculty of Medicine, Mansoura University, Egypt, Tel: 00201020883243; Email: anmghanem1@gmail.com
Citation: Ghanem AN (2020) Albumin or Hydroxyethyl Starch vs Saline for Volume Replacement in Surgical Patients partly Suggest Starling’s Law is Wrong, What Replacement is there? Perspective. Emerg Med Trauma. EMTCJ-100030
Received date: 19 March, 2020; Accepted date: 21 March, 2020; Published date: 27 March, 2020
Key points
Question: The use of HES for volume replacement therapy, compared with 0.9% saline, resulted in no significant difference. This means that neither HES nor albumin substitute has oncotic effect. What is the proof Starling’s law wrong and is there replacement and what is its clinical significance?
Findings: There is physics and physiological and clinical evidence to prove Starling’s law is wrong. There is evidence to suggest that using plasma or substitute of HES is no different from saline. This demonstrates oncotic pressure does not exist. Physics research demonstrates hydrostatic capillary (dynamic lumen) pressure induces suction not filtration. Physiological evidence demonstrates that the capillary works as G tube not Poiseuille’s tube. Hence Starling’s law is wrong on both hydrostatic and oncotic pressure forces. The correct replacement is the hydrodynamics of G tube.
Abstract
Introduction and objective: A recent article in JAMA demonstrated that the use of HES for volume replacement therapy, compared with 0.9% saline, resulted in no significant difference. This affirms that oncotic pressure of albumin is a fallacy in vivo, and Starling’s law is partly wrong. Thisperspective reports the complete evidence that Starling's law is wrong, and the correct replacement is the hydrodynamic of G tube. The clinical relevance and significance is discussed.
Material and methods: The physics proof is based on G tube hydrodynamic. Physiological proof is based on study of the hind limb of sheep: running plasma and later saline through the artery compared to that through the vein as regards the formation of oedema. The clinical significance is based on 2 studies one prospective and a 23 case series on volumetric overload shocks (VOS).
Results: Hydrodynamics of G tube showed that proximal, akin to arterial, pressure induces suction "absorption" not "filtration". In Poiseuille’s tube side pressure is all positive causing filtration based on which Starling proposed his hypothesis, The physiological evidence proves that the capillary works as G tube not Poiseuille's tube: Oedema occurred when fluids are run through the vein but not through the artery. There was no difference using saline or plasma proteinsin physiological and clinical studies. The wrong Starling's law dictates the faulty rules on fluid therapy inducing VOS and ARDS.
Conclusion: Hydrodynamic of the G tube challenges the role attributed to arterial pressure as filtration force in Starling’s law. A literature review shows that oncotic pressure does not work either. The new hydrodynamic of G tube is proposed to replace Starling’s law which is wrong on both forces. The physiological proof and relevance to clinical importance on the pathogenesis of clinical syndromes are discussed.
Keywords: AKI; ARDS; Albumin vs Saline; Capillary-interstitial fluid transfer; Capillary wall; Fluid therapy; Glycocalyx, Hyponatraemia; MODS; Pre-capillary sphincter; The TURP syndrome; Starling's law; Shock; Volume kinetics
Abbreviations
ARDS : The adult respiratory distress syndrome
AKI : Acute kidney injury
BFT : Bolus Fluid Therapy
CP : Chamber Pressure
CVS : Cardiovascular system
CNS : Central Nervous system
DP : Distal Pressure
EGDT : Early Goal-Directed Therapy
FP : Flow Pressure
G tube : Porous orifice tube
HN : Hyponatraemia
HST : Hypertonic sodium therapy of 5% NaCl and/or 8.4% Sodium Bicarbonate
ISF : Interstitial fluid
ICU : Intensive care unit
LP : Lumen Pressure
MODS : Multiple organ dysfunction syndrome
NaCo3 : Sodium bicarbonate
NaCl : Sodium chloride
PV : Plasma volume
PP : Proximal Pressure
RCT : Randomized controlled trial
TURP : The transurethral resection of the prostate
VK : Volume Kinetic
VO : Volumetric Overload
VOS : Volumetric overload shocks
VOS1 : Volumetric overload shock, Type 1
VOS2 : Volumetric overload shock, Type2
WW2 : World War Two
Introduction
The authors of this article by [1] on the Effect of Hydroxyethyl Starch vs Saline for Volume Replacement Therapy on Death or Postoperative Complications Among High-Risk Patients Undergoing Major Abdominal Surgery: The FLASH Randomized Clinical Trial in JAMA are commended on their excellent powerful study and report. It is a true representation of evidence based medicine. It has inspired me to write this perspective. This study would be perfect had they included one piece of data in the result section: The volumetric balance of patients during the surgery time i.e. volumetric overload over time (VO/T)that is compared for the occurrence of morbidity and mortality of the two groups receiving Hydroxyethyl starch (HES) vs saline. There should be a significant difference between patients with morbidity and mortality, and those who do not have such complications.
Fifner mentioned in discussion: “Patients received the amount of fluid the clinician thought necessary to restore or maintain intravascular volume” I applaud the truthful reality of this statement, and believe it pinpoint precisely where the problems are (highlighted here). Thus, if the volume of the given fluid during resuscitation is quantified in relation to time (VO/T) half the battle is won, and if the scientific basis underlying the thought that mislead physician to infuse such volume is verified and rectified the battle is over. In a letter on the BMJ editorial, I mentioned that SAFE trials and analysis are concerned only with the Type of fluid, albumin or HES vs saline, while missing the important issue of volumetric balance, measured in either volumetric or gravimetric (Body Weight BW) method.
Volumetric overload (VO) over Time (VO/T) is a concept verifiable by comparing patients’ body weight on ICU to that on hospital admission or before and immediately after surgery. This reveals a staggering VO of 12-14 litres of retained fluid in the acute respiratory distress syndrome (ARDS) 7 patients! In 1967, Professor [7] documented this volumetric fluid gain in the first report on ARDS, which became later known as the multiple organ dysfunction syndrome (MODS). Such VO data have not ever been since documented in any report other than mine. My research demonstrated that multiple regression analysis has proved that volumetric overload is the most significant factor in causing the clinical picture of VOS1 of the TURP syndrome [8] (Figure 2, 3 and Table 1). Volumetric balance is consistently missed in prospective trials. Not a single prospective SAFE or other trial report volumetric data in MODS syndrome patients, ARDS or AKI!
Fluid Type and Volume, and Time of gain, have vital significance in the pathogenesis and outcome of MODSor ARDS in post-surgical patients. Type of fluid gives characteristic serum solute dilution markers. Volume is directly, while time is inversely, related to the severity. Sodium-free fluids (Type 1) or VO1 dilute all serum or extracellular fluid contents including albumin, but its best marker is hyponatraemia (HN). The well-known transurethral resection of the prostate (TURP) [8] syndrome is a “model” of many such cases of HN of albumin or crystalloids seen in clinical practice. This “model” of TURP syndrome means it can be, and has been, precisely reproduced in animals in the absence of sepsis, hypothermia and recognized shocks. Hyponatraemia of <120 mmol/l is common hospital iatrogenic complication of fluid therapy that affects men, women and children and is usually lethal.
The TURP syndrome is induced by both the irrigating fluid absorption (1.5% Glycine, Sorbitol or Mannitol) and the infused intravenous fluids such as 5% Glucose [9, 10]. A quantity of 3.5-5 litres (l), gained during 1 hour surgery, induces a classical condition of volumetric overload shock type 1 (VOS1) while 5-6l may be lethal8. The VO of 3.5l may be considered normal daily intake and is tolerated over couple of hours but when gained in one hour it becomes pathological. The condition manifests clinically with paradoxical hypotension shock (Paradoxical means hyper- NOT hypo-volaemic shock) with features unrecognizable from or identical to hypovolaemic shock except for bradycardia and transient rare elevation of arterial pressure. It also has paradoxical AKI among other features of the MODS syndrome. This must to be kept in mind in order to recognize VO/T of VOS2, induced by SAFE fluids, with scarce markers if any. This is important as the TURP procedure is currently performed in saline irrigation (TURIS), so much more VOS2 with scarce or no markers will soon appear, and is also common in patients undergoing major surgery who received overzealous saline, HES or plasma infusions.
The common thought and practice of treating physician in such paradoxical VO/T shock is to infuse further volume of either SAFE albumin or crystalloids isotonic fluid! The physician aims to elevate arterial pressure by increasing vascular volume in the belief that he/she is facing hypovolaemic hypotension shock, while data indicate VO/T shock. The action just makes it worse or irreversible shock and establishes MODS when the patient is shifted to ICU. The insult of both SAFE and crystalloids isotonic fluids may occur in resuscitating the TURP syndrome with definite characteristic serum markers and proven clinical features, or may complicate overzealous resuscitation of any recognized shock, trauma, during major surgery or in ICU patients when serum markers are scarce or nil. Nothing to guide physician at all except his thought determined by current basic teaching on vascular volume andpressure relationship on one hand, and the forces of Starling’s law regulating the capillary-ISF circulation on the other. The latter determine the type and volume of SAFE fluid used in resuscitation of shock, trauma, burns, haemorrhage and sepsis and prolonged major surgery. So the faulty Starling's law is responsible for misleading physicians into giving too mush fluids.
Sodium-based fluids (VO2) such as saline, albumin, plasma substitutes of HES and blood may also induce VO/T shock identified as volumetric overload shock type 2 (VOS2). It may complicate the resuscitation of the TURP syndrome when VO2fluids erase HN while worsening VO. The main serum marker of using saline or HES becomes hypoalbuminaemia [9] that is not as marked as HN. It also has the same clinical features of paradoxical hypotension shock and MODS Syndrome. It may complicate resuscitation of any recognized shock and fluid resuscitation during major surgery complicating both saline and plasma or substitutes of HES. The transition from hypo- to hyper-volaemic hypotension shock is hard or impossible to detect. No stop sign to show that such patient is having hyper-volaemic not hypo-volaemic hypotension shock. None to warn when the quantity needed in treating true hypovolaemia is surpassed. Vascular pressures of central venous pressure (CVP), pulmonary capillary wedge pressure(PCWP) and blood pressure (BP) changes of VO/T are identical except for bradycardia and an occasional transient initial rise of BP10. Massive plasma and blood infusions have no serum markers at al or specific vital signs except VO2 increase of body weight or calculated VO and occurrence of MODS or ARDS or AKI occurring in any combinations, but one system may predominate.
It should be realized that hypotension is not always synonymous with hypovolaemia. It is worth mentioning also that, up to this point, sepsis is as innocent as the wolf in Joseph story. A little later, sepsis will do its nasty work and further complicate MODS into its current trendy name associated with sepsis, termed the systemic inflammatory response syndrome (SIRS). The scientific basis that underlies physician’s thought while resuscitating a patient is explained later. The evidence on how and why Starling’s law10 is wrong on both forces while continuing to dictate the faulty rules on fluid therapy concerning the type and incorrect volume of fluid in resuscitation while volume is consistently missed in SAFE trials is explained here.
On the physiological issues; the direct positive relationship of fluid volume and pressure, the work of Poiseuille on flow and pressure exerted on the wall of strait uniform brass tubes, as well as the albumin oncotic pressure, were all imported by Starling10 in 1896 direct from physics to medicine at the Lancet without any physiological verification or testing what so ever! Modern clinical chemistry allowed verification of albumin oncotic pressure by [6] comparing variety of body fluids to plasma protein- there was no difference. The real ultra-structure of the capillary wall revealed by Karnovesky [5] and the pre-capillary sphincter revealed by Rhodin [11] were reported in 1967. Hence Renkin called for reconsideration of Starling's hypothesis [12] in 1986.The hydrodynamic of a porous orifice tube was reported in 2001[13]. Thus, all physiological research done before 1962 that advocated Starling’s hypothesis promoting it into law is invalid. Based on the consequences of capillary permeability to macromolecules demonstrating that oncotic pressure does not work in vivo, Renkin [12] advocated reconsideration of Starling’s hypothesis. What alternative was there then? There was none. Only an idea in mind derived from clinical observation on the use of fluids in resuscitation of shock, trauma and the TURP syndrome was communicated and reported at BMJ9 in 1985. The results of the physics study on the hydrodynamic of the G tube were completed but unreported until 2001 [13].
The direct proportional relationship of fluid volume to pressure works in the vascular system up to a limit only. This is true in physics too, if too much fluid is pushed into a reservoir above its capacity, it will burst and the volume-pressure relationship vanishes. Thus, perhaps volume replacement in shock should not exceed in total the maximum capacitance of vascular system of 7l in adult. Considering that blood loss is fatal when about half the vascular volume is acutely lost, a replacement should not exceed the lost volume after control of bleeding. After any overzealous vascular volume expansion, the excess fluid must leak out into and drown the interstitial space and cells! The most deleterious effect of such internal drowning is on the vital organs. Both vital organ signs8 and post-mortem findings [14] demonstrate the massive volume of retained fluids. This letter to Editor [14] is the only documented evidence in literature that reported the massive retained fluid volume with swollen vital organs at post mortem examination! The only article that reported retained fluid volume was the first report on ARDS by [7] in addition to the articles of mine some of which are referenced here.
Albumen oncotic pressure, no doubt, exists in vitro across membrane impermeable to its molecules. Even, in such physics experiments, oncotic pressure is too weak and too slow force to be effectively and solely responsible for fluid return into capillary lumen6. It has cell building nutritional value, how does albumin reach the cells? It must cross the capillary wall! However, the evidence that oncotic pressure works in vivo is non-existing [1-3]. The only difference between albumen or HES and saline fluids in SAFE and FLASH trials is the added albumin or starch presumed to have oncotic pressure, a function of its molecule size in relation to pore size or permeability of membrane. The pores of normal capillary wall became known [8] decades after Starling’s report on his hypothesis. Karnovesky has shown the intercellular slits between capillary wall cells to allow horse radish, a much larger molecule than albumin, to pass freely across the capillary wall [5]. As the result of these trials 1,2 demonstrated that both SAFE fluids have similar outcome, this further re-affirms that albumen oncotic pressure in clinical medicine [1,2-4], clinical chemistry [6] and modern physiology [15-17] is fallacy in vivo, simply because albumen molecules pass freely across the large pores of normal capillary membrane [5].
This may answer the BMJ slogan: Why albumin may not work. So, irrespective whether albumin has equal or worse outcome, the fact that it did not show clear superiority to saline in SAFE trials is affirmative evidence that albumen oncotic pressure is fallacy in vivo. Such fallacy has also been long proved in biochemical [6] and physiological research [15-17]. Oncotic pressure is the presumed main absorption force in capillary-interstitial fluid (ISF) transfer, and represents one half of the equation of Starling’s law [10]. Thus as it has proved wrong, the law must be wrong! This was the reason for the call to reconsider Starling’s hypothesis [12]. However, there was no existing alternative then- only an idea in mind communicated at BMJ9 in 1985. This was later verified and reported, the clinical work [8] in 1990 and physics work [13] in 2001 as well as in more recent articles [18-21], and a book [22].
Verifying the other half of Starling law equation concerning capillary arterial pressure as the filtration force was my objective. Does the capillary have positive pressure on its wall pushing fluid out? Does the flow pressure akin to arterial pressure cause filtration? Does the capillary tube act like Poiseuille’ strait uniform tube and have positive pressure on its wall that pushes fluid out through pores? The ultra-structure of capillary wall [5] and pre-capillary sphincter [11] were discovered 80 years after Starling reported his hypothesis. The capillary proved a porous orifice tube. I made several porous tubes fitted with narrow orifice mimicking the capillary with a pre-capillary sphincter on a larger scale to verify this. The G tube was surrounded by a chamber C to represent the ISF space. These porous orifice tubes were used to study hydrodynamic flow and pressure and compared to Poiseuille’s tube, particularly in relation to the side pressure exerted on its wall.
The porous orifice (G) tube hydrodynamic proves totally different to Poiseuille’s tube. There was no positive pressure exerted on the wall and no fluid filtered out over the proximal half of the porous orifice tube. The flow pressure representing arterial pressure is not responsible for filtration! It caused mainly suction maximum at the proximal part of the G tube. Thus the main force in the equation on Starling’s law concerning arterial capillary pressure filtration is also wrong. How does it work? What pushes the fluid out and what returns it in? Does the G tube hydrodynamic offer a complete hypothesis to explain the capillary-interstitial fluid exchange? How does it relate to physiology and medicine? To know the answer to these questions on a most fascinating phenomenon of the G tube, please read the articles [12,17-21] or the book [22].
So, the law dictating the scientific basis that underlies physician’s thought on vascular volume expansion at resuscitation of shock, trauma and acutely ill patients is wrong on all accounts. The most harmful part of this erroneous law is in fact that concerning arterial pressure, presumed to be the main filtration force in the capillary. This is the part that Starling thought the capillary acts like Poiseuille’s strait uniform tube, exerting positive pressure on the wall that filters fluid out.
The complete evidence that Starling's law is wrong and the correct replacement is the hydrodynamic of the porous orifice tube is summarised here, and has been reported elsewhere [23]:
Dr Starling10proposed his hypothesis >80 years prior to the discovery of the capillary ultrastructure and correct physiology which are as follows. He based his hypothesis on Poiseuille's work [24] in which the hydrostatic pressure is a positive function of the arterial pressure causing filtration, but in the G tube hydrodynamic as a porous orifice tube- akin to the capillary this pressure is different causing suction. Thus Starling's low is wrong on both forces because;
This underlies the treating physician’s thought when embarking on overzealous fluid infusion during the resuscitation of shock and prolonged major surgery. He was taught that volume expansion has direct positive unlimited relationship with pressure. It is the only way he knows off to improve capillary circulation. Well, it does not. Volume replacement is effective when an actual blood volume loss is restored to normal that is less than maximum capacity of the vascular system. After that the relation of volume to pressure is reversed. Any excess volume, vascular expansion or hypervolaemia of VO/T induces hypotension shock just like hypovolaemia does! Considering the concept of VO/T by reporting volume of fluids in future SAFE trials and verifying the scientific basis of fluid resuscitation in shock are needed for resolving the puzzle of MOVD/F syndrome or ARDS and improving outcome of surgical patients on ICU.
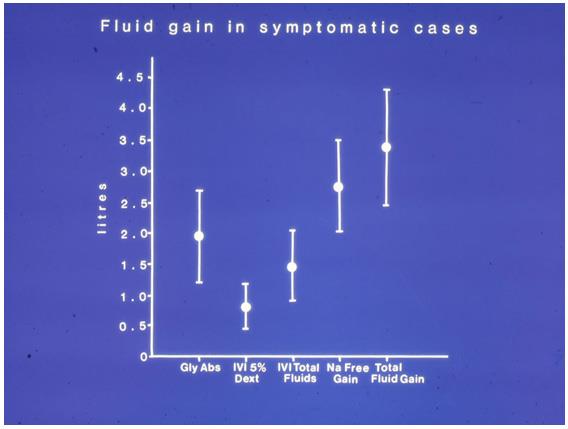
Figure 1: Shows the means and standard deviations of volumetric overload in 10 symptomatic patients presenting with shock and hyponatraemia among 100 consecutive patients during a prospective study on the transurethral resection of the prostate (TURP). The fluids were of Glycine absorbed (Gly abs), intravenously infused 5% Dextrose (IVI Dext) Total IVI fluids, Total Sodium-free fluid gained (Na Free Gain) and total fluid gain in litres.(Reproduced with permission of the author and Editorof BJU Int. from this article reference8).
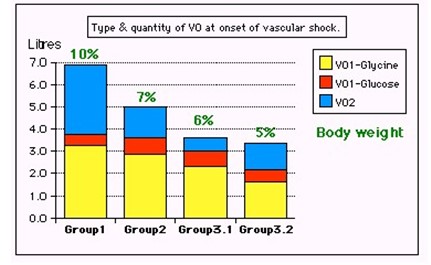
Figure 2: Shows volumetric overload (VO) quantity (in litres and as per cent % of body weight) and types of fluids. Group 1 was the 3 patients who died in the case series as they were misdiagnosed as one of the previously known shocks and treated with further volume expansion. Group 2 were 10 patients from the series who were correctly diagnosed as volumetric overload shock and treated with hypertonic sodium therapy (HST). Group 3 were 10 patients who were seen in the prospective study and subdivided into 2 groups; Group 3.1 of 5 patients treated with HST and Group 3.2 of 5 patients who were treated with guarded volume expansion using isotonic saline.(Reproduced with permission of the author from this article reference 21).
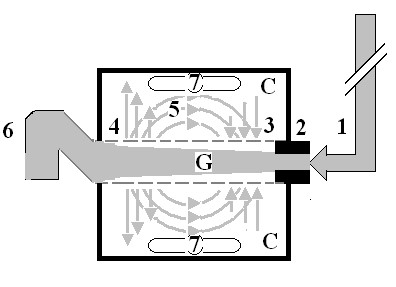
Figure 3: Shows Diagram of the porous orifice (G) tube enclosed in chamber (C) based on several photographs demonstrating the magnetic field-like G-C circulation phenomenon. The proximal inflow (arterial) pressure (1) pushes fluid through the orifice (2) creating fluid jet in the lumen of the G tube. The fluid jet creates negative side pressure gradient causing suction maximal over the proximal half of the G tube near the inlet (3) that sucks fluid into lumen. The side pressure gradient turns positive pushing fluid out of lumen over the distal half maximally near the outlet (4). Thus the fluid around G tube inside C moves in magnetic field-like fluid circulation (5) taking an opposite direction to lumen flow of G. tube. The inflow (arterial) pressure (1) and orifice (2) induce the negative side pressure energy creating the dynamic G-C circulation phenomenon that is rapid, autonomous and efficient in moving fluid out from the G tube lumen at (4), irrigating C at (5), then sucking it back again at (3), maintaining net negative energy pressure (7) inside C. The distal outflow (venous) pressure (6) enhances outflow at (4) and its elevation may turn the negative energy pressure (7) inside C into positive, increasing volume and pressure inside C chamber. (Reproduced with permission of the author from this article reference 20)
|
Parameter |
Value |
Std. Err |
Std. Value |
T Value |
P |
|
Intercept |
- |
- |
0.773 |
- |
- |
|
Fluid Gain (l) |
0.847 |
0.228 |
1.044 |
3.721 |
0.0001 |
|
Osmolality |
0.033 |
0.014 |
-0.375 |
2.42 |
0.0212 |
|
Na+ (C_B) |
0.095 |
0.049 |
0.616 |
1.95 |
0.0597 |
|
Alb (C_B) |
0.062 |
0.087 |
0.239 |
0.713 |
0.4809 |
|
Hb (C_B) |
-0.282 |
0.246 |
-0.368 |
1.149 |
0.2587 |
|
Glycine (C_B) |
-4.97E-05 |
5.98E-05 |
-0.242 |
0.832 |
0.4112 |
Table 1: Shows the multiple regression analysis of total per-operative fluid gain, drop in measured serum osmolality (OsmM), sodium, albumin, Hb and increase in serum glycine occurring immediately post-operatively in relation to signs of the TURP syndrome. Volumetric gain and hypo-osmolality are the only significant factors; fluid gain is highly significant.(Reproduced with permission of the author and Editorof BJU Int. from this article reference 8).
Citation: Ghanem AN (2020) Albumin or Hydroxyethyl Starch vs Saline for Volume Replacement in Surgical Patients partly Suggest Starling’s Law is Wrong, What Replacement is there? Perspective. Emerg Med Trauma. EMTCJ-100030