Emergency Medicine and Trauma Care Journal
ISSN: 2652-4422
Case Report
A Case Report in Cardiology, Emergency and Critical Care Ketotic Hyperkalemia-Induced Junctional Tachycardia Reversed with Insulin and Saline; A Case Report
Elsayed YMH*
Critical Care Unit, Fraskour Central Hospital, Damietta Health Affairs, Egyptian Ministry of Health (MOH), Damietta, Egypt
*Corresponding author: Yasser Mohammed Hassanain Elsayed, Critical Care Unit, Fraskour Central Hospital, Damietta Health Affairs, Egyptian Ministry of Health (MOH), Damietta, Egypt.
Citation: Elsayed YMH (2020) A Case Report in Cardiology, Emergency and Critical Care Ketotic Hyperkalemia-Induced Junctional Tachycardia Reversed with Insulin and Saline; A Case Report. Emerg Med Trauma. EMTCJ-100026
Received date: 10 Febraury, 2020; Accepted date: 17 February, 2020; Published date: 22 Febraury, 2020
Abstract
Rationale: Serum potassium concentration is usually elevated in the cases of diabetic ketoacidosis. Hyperkalemia is an established cause of junctional tachycardia. Insulin decreases potassium levels in the blood by redistributing it into cells via increased sodium-potassium pump activity.
Patient concerns: A middle-age Mongol male patient presented to the emergency department with diabetic ketoacidosis and junctional tachycardia.
Diagnosis: Hyperkalemia-induced junctional tachycardia in diabetic ketoacidosis.
Interventions: Electrocardiography, oxygenation, central venous pressure monitoring, and echocardiography.
Lessons: Electrolytes disturbance especially hyperkalemia is a significant serious metabolic problem in ketoacidosis. Hyperkalemia is a possible cause of junctional tachycardia in diabetic ketoacidosis.
Outcomes: Successful reversal of ketotic hyperkalemia-induced coronary artery spasm and junctional tachycardia with insulin and saline.
Keywords: Diabetic ketoacidosis; Induced junctional tachycardia; Insulin and saline; Ketotic hyperkalemia
Abbreviations
AVN : Atrioventricular node
DKA : Diabetic ketoacidosis
ECG : Electrocardiogram
ICU : Intensive care unit
SAN : Sinoatrial node
Introduction
The admission serum potassium concentration is usually elevated in patients with diabetic ketoacidosis (DKA) [1]. Potassium levels can fluctuate severely during the treatment of DKA because insulin decreases potassium levels in the blood by redistributing it into cells via increased sodium-potassium pump activity [2]. Despite a total body potassium deficit of ~ 3-5 mEq/kg of body weight, most patients with DKA have a serum potassium level at or above the upper limits of normal. In a recent series, the mean serum potassium in patients with DKA was 5.6 mEq/l, respectively. These high levels occur because of a shift of potassium from the intracellular to the extracellular space due to acidemia, insulin deficiency, and hypertonicity [1]. The primary treatment of DKA is with intravenous fluids and insulin [3]. Both insulin therapy and correction of acidosis decrease serum potassium levels by stimulating cellular potassium uptake in peripheral tissues [1]. A large part of the shifted extracellular potassium would have been lost in urine because of osmotic diuresis. Hypokalemia (low blood potassium concentration) often follows treatment [2]. Therefore, to prevent hypokalemia, most patients require intravenous potassium during DKA therapy. This increases the risk of dangerous irregularities in the heart rate. Therefore, continuous observation of the heart rate is recommended [2], as well as repeated measurement of the potassium levels and addition of potassium to the intravenous fluids once levels fall below 5.3 mmol/l. If potassium levels fall below 3.3 mmol/l, insulin administration may need to be interrupted to allow correction of the hypokalemia [4]. Replacement with intravenous potassium (two-thirds as potassium chloride [KCl] and one-third as potassium phosphate [KPO4] should be initiated as soon as the serum potassium concentration is below 5.0 mEq/L. The treatment goal is to maintain serum potassium levels within the normal range of 4–5 mEq/L [1].
The implicated nomenclature [5] to recognize the type of junctional rhythms (JR) is based on their rate. They are classified as follows:
Hyperkalemia, sick sinus syndrome, pericarditis, myocarditis, unstable angina, acute myocardial infarction, repair of congenital heart disease, atrial septal defect, tetralogy of Fallot, persistent left superior vena cava, adenosine, digoxin, calcium channel blockers, lithium, amitriptyline, clonidine, reserpine, inhalation anesthetics, cimetidine, isoproterenol infusion, narcotics, beta-blockers, and ivabradine implicated in causing junctional tachycardia [5,9-11].
Case presentation
A 45-year-old single Egyptian male patient presented to the emergency department with dizziness, palpitations, and rapid breathing. The patient had a history of diabetics on oral hypoglycemic glimepiride (3 mg once daily). The mother gave a history of Down syndrome since birth. Upon examination, the patient appeared irritable, confused, sweaty, tachypneic and have Mongolic faces. His vital signs were as follows: the blood pressure of 90/70 mmHg, the heart rate of 140/minute, the temperature of 38.2°C, respiratory rate of 28/min, and the initial pulse oximetry of 97%. The patient was admitted to the intensive care unit (ICU) as diabetic ketoacidosis. The patient initially treated with act-rapid insulin (initial 10 units IVB), normal saline 0.9% (1000 ml IVB in the first hour), hourly vital signs monitoring, hourly blood glucose measurement, and hourly urinary acetone check-up. Maintenance of act-rapid insulin (0.1 u/kg; 10 u/hours) was continued for about 6 hours. Another 1000 ML normal saline 0.9% was added. IV Cefotaxime 1gm/6 hours, and IV ampicillin-sulbactam 1.5 gm/6 hours were prescribed. RBS was 602 on admission and urine analysis (glucose ++++ acetone ++). ABG showed metabolic acidosis. Electrolytes profile showed plasma Na+: 132 mg/dl, plasma Ka+: 5.9 mg/dl, I Ca++: 1.14 mmol/L. Urgent ECG recording (Figure 1A-B) showed junctional tachycardia.
Serial ECG tracings were done for follow up. RBS measures were steadily gradually decreased until RBS become;174 mg/dl, the disappearance of urinary acetone. IVI dextrose 5% added with adjustment of act-rapid insulin to (4 units per hour), and A 250 ml Ringer solution over 2 hours, and 250 ml Ringer solution over 2 hours. Electrolytes profile repeated within 6 hours of management showed normalized plasma Na+: 138 mg/dl, plasma Ka+: 4.8 mg/dl, I Ca++: 1.21 mmol/L. ECG tracing was done within 6 hours of the first one that showed the disappearance of junctional tachycardia with the appearance of superficial T- wave inversion in III, aVF, and V1-5 leads (Figure 2). Later echocardiography was normal. The patient discharged after stability within 24 hours of admission.
Discussion
Overview: A 45-year-old single Egyptian male Mongolic patient presented with diabetic ketoacidosis and junctional tachycardia with associated marked hyperkalemia.
The primary objective for my case study was the diagnosis of both diabetic ketoacidosis and junctional tachycardia.
The secondary objective for my case study was the choice management for diabetic ketoacidosis and junctional tachycardia with associated marked hyperkalemia.
Limitations of the study: There are no known limitations in the study. I can’t compare the current case with similar conditions. There are no similar or known cases with the same management for near comparison.
Study question here; How did the relationship among diabetic ketoacidosis and junctional tachycardia, elevated potassium level, and insulin therapy?
Recommendation
Conclusion
The physician should consider spontaneous recovery of both junctional tachycardia and hyperkalemia on the initial management of diabetic ketoacidosis. So, don’t hurry to treatment, but tight follow up for elevated potassium level is obligatory.
Acknowledgment
I wish to thank the emergency department and critical care unit nurses who make extra-ECG copies for helping me.
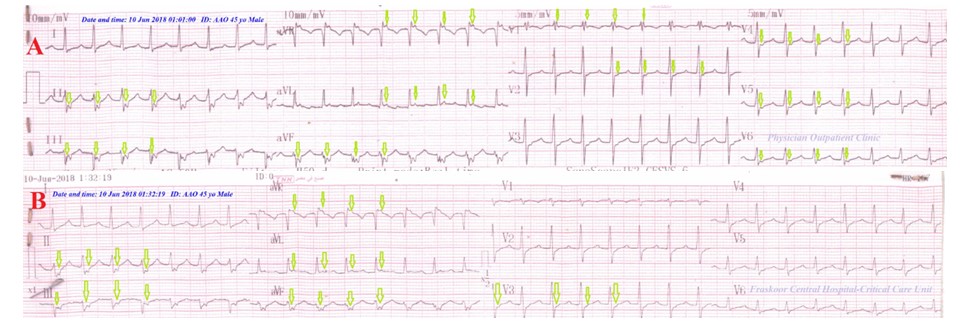
Figure 1: ECG tracings; A. tracing of Physician Outpatient Clinic showing junctional tachycardia “evidenced with retrograde P-wave “II, III, aVF, aVL, aVR, and V1, 2, 4,5,6 leads” (green arrows) and absent P-wave “the remaining leads”. B. tracing of the ICU admission within one hour of management showing junctional tachycardia “evidenced with retrograde P-wave (green arrows) (II, III, aVF, aVL, aVR, and V3) and absent P-wave “the remaining leads”.
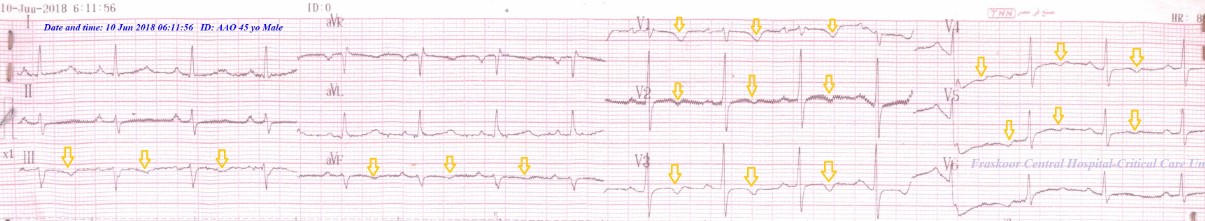
Figure 2: ECG tracings on the ICU following up showing the disappearance of junctional tachycardia with the appearance of superficial T- wave inversion in III, aVF, and V1-5 leads (gold arrows).
Citation: Elsayed YMH (2020) A Case Report in Cardiology, Emergency and Critical Care Ketotic Hyperkalemia-Induced Junctional Tachycardia Reversed with Insulin and Saline; A Case Report. Emerg Med Trauma. EMTCJ-100026