Journal of Diabetes Management and Metabolism
(ISSN 2652-4430)
Research Article
Using Education to Improve Hba1c in Older Adults with Diabetes
Grant CG1, Castillo A2 , Fleck SB3, Lu F1, Kabir UY4 and Mzayek F4
1Qsource, USA
2Centers for Medicare & Medicaid Services, USA
3School of Public Health, The University of Memphis, USA
4College of Social Work, The University of Illinois at Chicago, USA
*Corresponding author: Grant CC, Qsource, The University of Memphis, USA, Tel: 9013402098, Fax: 901-761-3786; Email: cgrant@qsource.org
Citation:Grant CG1, Lu F, Fleck SB, Kabir UY, Mzayek F and Castillo A (2020) Using Education to Improve Hba1c in Older Adults with Diabetes. J Diabetes ManagMetab: JDMM-10009
Received date: 13 February, 2020;Accepted date:18February, 2020;Published date: 26 February, 2020
Abstract
Objective: To provide a preliminary assessment of the effectiveness of a peer-led diabetes self-management Education (DSME) intervention in older adults.
Methods:The study sample included 1,007 older adults with diabetes who participated in a DSME intervention, based on the Diabetes Empowerment Education Program (DEEP) curriculum, between August 2014 and July 2018. Pre- and post-intervention data on several markers of cardio metabolic risk: glycosylated hemoglobin (HbA1c), high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, total cholesterol and triglycerides were collected from participants’ primary care medical records within the 12 months preceding the first class and the 12 months following the last intervention session.
Results:Mean HbA1c improved by 4.3% (mean difference (MD)=-0.33, 95% confidence interval (CI)=-0.48,-0.18).The mean levels of LDL cholesterol (MD= -3.84 mg/dL, 95% CI= -7.60, -0.08), total cholesterol (MD= -5.13 mg/dL, 95% CI= -9.46, -0.80) and triglycerides (-9.41 mg/dL, 95% CI= -18.02, -0.80)decreased significantly.
Conclusion: These findingssuggest that older adults with diabetes can benefit from a community-based, peer-led educational diabetes programand demonstrate the feasibility of implementation of DEEPon a large scale. Given the large number of older adults with diabetes,increased supportfor the DEEP program may be warranted.
Keywords:Cholesterol; Diabetes mellitus;Diabetes Empowerment Education Program;HbA1c;Diabetes self-management education; Older adults
Abbreviations
ADA : American Diabetes Association
CI : Confidence interval
CMS : Centers for Medicare & Medicaid Services
DSME : Diabetes self-management education
DEEP : Empowerment Education Program
HbA1c : Glycosylated hemoglobin
HDL cholesterol : High-density lipoprotein
IRB : Institutional review board
LDL cholesterol : Low-density lipoprotein
MD : Mean difference
QIN-QIOs : Quality Innovation Network-Quality Improvement Organizations
TDM : Type-2 Diabetes Mellitus
Introduction
Approximately 23 million people in the U.S. have diabetes [1]. Diabetes is one of the ten most expensive disease categories [2] and the average medical expenditure among people diagnosed with diabetes is more than two times higher than that for people without diabetes [3]. Adequate control of diabetes reduces the risk of diabetes-related complications and improve the quality of life of the patients [4]. A systematic review showed that the level of glycosylated hemoglobin or HbA1c, a marker of glycemia that can be used to assess the adequacyof diabetes control,is positively associated with overall mortality in diabetes patients [5]. Additionally, the evidence suggests a strong association of HbA1c with diabetes-related complications, with an estimated 21% reduction in risk of complications for each 1% reduction in HbA1c [6]. Therefore, proactive diabetes management to better control glycaemia can reduce the risk of complications,improve the quality of life, and reduce cost.
Health education interventions can improve self-care complianceand significantly increase self-efficacy among diabetes patients leading to areductionofHbA1c levels [7,8]. In 2014,Centers for Medicare & Medicaid Services (CMS), the federal agency responsible for administering Medicare, Medicaid and several other health care programs the Centers for Medicare & Medicaid Services (CMS) launched the Everyone with Diabetes Counts programnationwide in order to improve health outcomes in persons with diabetes through education, especially among underserved Medicare populations. Everyone with Diabetes Counts was carried outby the 14 Quality Innovation Network–Quality Improvement Organizations (QIN-QIOs) in all fifty states and U.S. territories under contract with CMS. Aprimary intervention of this program is the provision of Diabetes Self-Management Education (DSME) using the Diabetes Empowerment Education Program (DEEP) curriculum.
Research has shown the effectiveness of DSME programs in improving outcomes for patients with diabetes [9-12] including enhancing the knowledge and better monitoring of blood glucose and general glycemic control in Type-2 Diabetes Mellitus (T2DM) patients [13]. Several other studies have examined the effectiveness of DSME programs in different subpopulations including T2DM patients living in rural communities, African Americans, and Mexican Americans [14-16].
While the DEEP curriculum is considered as one of the good approaches for DSME [17] no study has assessed the effectiveness of DSME intervention using DEEP curriculum in a large older adult population. In this paper, we examined the clinical impact of the DSME intervention, measured by change in HbAc1 and other metabolic markers of CV risk,in older adults using the pre-posttest approach.
Materials and Methods
Population: The population includesa sample of 1,007 adults 65 years old and older (Figure 1), living with diabetes, who resided in the states and territory of Alaska, Alabama, Georgia, Hawaii, Iowa, Illinois, Indiana, Kentucky, Louisiana, Mississippi, Montana, Nebraska, North Dakota, North Carolina, Puerto Rico, Tennessee, and Wyoming, and who completed DEEP based DSME intervention between August 2014 and July 2018. Data were collected during the same time period. Participants provided written authorization to allow the extraction of their health information.Data were collected and extracted in each state and sent to the QIN-QIO National Coordinating Center Contractor. The work reported in this article represents a quality improvement program that is part of healthcare operations and, therefore, exempt from institutional review board (IRB) approval.
Intervention: The intervention comprised 2½ hours of educational sessions per week for 6-weeks offered by health professionals or peer leaders after they have received three full days of DEEPeducator training. The recommended class size ranges from 10 to 15 participants, and the weekly sessions were held in community venues, including churches and senior centers. The DEEP curriculum aims to “increase diabetes knowledge, develop self-management skills, and facilitate behavioral change” [18]. The curriculum is divided into eight modules corresponding to the areas defined by the American Diabetes Association (ADA): diabetes risk factors, diagnosis, treatment, and complications; nutrition; physical activity; psychosocial aspects; self-care skills; goal-setting; identification of important clinical markers; effective communication with providers; self-advocacy, and utilization of community resources [19].
Study outcomes: HbA1cmeasures the percentage of glycated hemoglobin in the blood. It is used as an indicator of how well the blood glucose is controlled because it represents the average levels of blood glucose within the previous twelve weeks. The acceptable treatment target is <7% [8]. Blood lipids, such aslow-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides are markers of cardiovascular risk and abnormal levels are common in diabetes patients, which contributes to their higher risk of atherosclerotic cardiovascular disease [20].
Data Collection: Blood HbA1c, LDL cholesterol, HDL cholesterol, total cholesterol, and triglycerides, measured during the 12 months before the participant began the intervention,were retrospectively abstractedfrom each participant’s primary care medical record. Post-DEEP measurements were collected during the 12 months following each participant’s final DEEP class. Dates were established according to the date of the test as recorded in the medical record.Attendees completed a registration form on their first day of class to allow collection of key information, includinglevel of education, race and ethnicity, smoking status, history and type of diabetes, and date of birth.
Statistical Analyses: Pre- and Post-DEEP means of the outcome variables were compared using the paired t-test and Wilcoxon signed rank sum test as appropriate. Participants with an HbA1cless than 4% or more than 20%,LDL cholesterol less than 10 mg/dL or more than 400 mg/dL, and HDL cholesterol less than 10mg/dL or more than 150 mg/dL were excluded because they are unlikely and may represent measurement error or severe comorbidities.Alpha level was set at .05 for all analysis. All data analyses were conducted using SAS 9.3 (SAS Institute Inc., Cary, NC).
Results
Demographic and clinical characteristics of the population are detailed in Table 1. Among the 1,007 study participants, 73%were female and their mean age was 72±14 years. Ninety-six percent of the study samplehad Medicare insurance. Approximately, 12% of participants reported pre-diabetes, 5% had Type-I diabetes and 76 % had Type-II diabetes.
Overall, the mean HbA1clevel decreased from 7.59% to 7.26% (mean difference (MD)=-0.33%, 95% confidence interval (CI) = -0.48, -0.18) from pre- to post-DEEP.This represents a 4.3%relative improvement rate.Average LDL cholesterol decreased from 89.32 mg/dL to 85.48 mg/dL (MD=-3.84 mg/dL, 95% CI= -7.60, -0.08), a 4.3% relative improvement. The mean total cholesterol level of the study participants also decreased from 170 mg/dL to 165 mg/dL (MD=-5.13 mg/dL, 95% CI= -9.46, -0.80), corresponding to a 3.0% improvement. Finally, the average triglycerides levels decreased from 158.43 mg/dL to 149.02 mg/dL (MD=–9.41 mg/dL, 95% CI=-18.02, -0.80), a5.7% improvement.Although HDL cholesterol trended favorably, it was not statistically significant(Table 2).
Discussion
To our knowledge, this is the largest, multi-state implementation and evaluation of the effect of DEEP-based DSME intervention on cardio metabolic risk factors among individualswith diabetes in community settings. We found a significant decrease in the averageHbA1clevel among participants during the 12-monthpost-DEEP period. This finding is consistent with [18] which reported a reduction inHbA1cafter DEEP among younger participants, [18] andsuggests that DEEP-based DMSE intervention can be an effective tool for self-control of diabetesin olderpopulations.Research has demonstrated that HbA1c is an independent predictor of several comorbidities such as, hypertension, coronary heart disease and depression, as well as healthcare cost [21]. Reducing glycemic levels delays the development and progression of complications [6, 9,22-24] and, consequently, reduces the medical costs of diabetes care [21,25-26]. Based onprior research that suggested a 1% improvement in HbA1clevel is associated with a 21% reduction in risk of complications [6] and around $995 in cost reduction [26] the apparently modest 4.3% relative improvement that we observed would suggest a noteworthy reduction in the risk of complications and cost savings.
There was also improvement in other cardio metabolic risk factors, albeit small. The clinical significance of these changes, therefore, is hard to evaluate. However, it should be noted that these reductions are on the population average, not on the individual level. This means that some individuals in the sample have more significant reductions that could convey clinical benefits. Moreover, since the improvements wereobserved in severalcardio metabolic markers, the combined effect of these improvements may also have amore positive clinical than that of any individual marker. This is especially true if these changes are sustained over time since all these markers are long-term risk factors.
Although this study has several strengths like large geographical coverage andclinically measured outcomes, the study is not without limitations. Data were collected during the course of regular care to meet CMS quality improvement requirements, not as part of a study specifically designed to assess DEEP curriculum based DSME intervention. As a result, not all participants had information for both Post-DEEPperiods, preventing the ability to evaluate all participantsat both post-tests. Secondly, the participants included those who volunteered to participate in the intervention, which may limit the generalizability of the findings. However, including a large number of states in the analysis minimizes some of the geographical differences and increases the potential generalizability of findings. Finally, the sample size does not allow for subgroup analyses for type 1, type 2 and pre-diabetes.
As with all pre-post studies, this study was also susceptible to various threats to internal validity for the lack of a comparison group. However, other studies published on the implementation of the DEEP based DSMEprogram, including those in clinical settings that are more controlled, corroborate the positive impact of the intervention[9, 10-12].
Conclusion
The purpose of this paper was to assess the impact of DEEP based DSME intervention on cardio metabolic markers of diabetesin the largest implementation of the program in real life scenarios. Our results indicate that the DEEP curriculum impacts key clinical measures that may convey benefits in terms of complication reduction and cost-saving.These results warrant further evaluation of the DEEP program in larger settings because educational interventions for self-management of diabetes may prove to be important tools in tackling diabetes.
Acknowledgement
We wish to acknowledge Zachariah Peterson and the following organizations whose work contributed to this project:Alabama Quality Assurance Foundation, Alliant Quality, Great Plains Quality Innovations Network, Health Services Advisory Group, Information and Quality Healthcare, Mountain-Pacific Quality Health, Quality Insights, Qsource, Telligen and TMF.
The activities described in this article were performed under contract HHSM5002014QIN titled Medicare Quality Innovation Network - Quality Improvement Organization for region 6, funded by the Centers for Medicare & Medicaid Services, an agency of the U.S. Department of Health and Human Services. The content is solely the responsibility of the authors and does not necessarily represent the official views or policies of the CMS.
The authors assume full responsibility for the accuracy and completeness of the ideas presented. This article is a direct result of the Quality Improvement Organization Program initiated by the Centers for Medicare & Medicaid Services, which has encouraged identification of quality improvement projects derived from analysis of patterns of care, and therefore required no special funding on the part of this contractor.
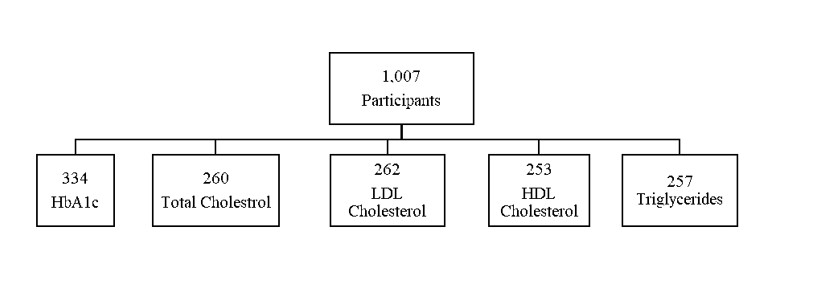
Figure 1: Sample size for each analyzed outcome.
|
Demographics |
Frequency |
Percent |
|
Gender |
||
|
Female |
732 |
72.7 |
|
Insurance status |
||
|
Medicare |
967 |
96 |
|
Race |
||
|
White |
509 |
50.6 |
|
Black |
364 |
36.2 |
|
Asian |
68 |
6.8 |
|
Pacific Islander |
32 |
3.2 |
|
Other |
34 |
3.4 |
|
Education level |
||
|
Some High School/Diploma |
460 |
45.7 |
|
Some College/Degree |
317 |
31.5 |
|
Some Graduate School |
59 |
5.9 |
|
Smoking status |
||
|
Smoker |
50 |
5 |
|
Diabetes type |
||
|
Pre-diabetes |
125 |
12.4 |
|
Type-I diabetes |
53 |
5.3 |
|
Type-II diabetes |
763 |
75.8 |
|
Blood pressure |
||
|
Hypertension |
740 |
73.5 |
|
High cholesterol |
||
|
Hyperlipidemia |
532 |
52.8 |
|
- |
Mean |
SD |
|
Age |
73 |
14 |
Table 1: Demographic and clinical characteristics of study participants.
|
Metabolic Factor |
n |
Pre-DEEP |
Post-DEEP |
MD |
95%CI |
|
HbA1c (%) |
334 |
7.59 |
7.26 |
-0.33** |
-0.48, -0.18 |
|
LDL Cholesterol (mg/dL) |
262 |
89.32 |
85.48 |
-3.84* |
-7.60, -0.08 |
|
HDL Cholesterol (mg/dL) |
253 |
49.36 |
50.01 |
0.65 |
-0.63, 1.93 |
|
Total Cholesterol (mg/dL) |
260 |
170.01 |
164.88 |
-5.13* |
-9.46, -0.80 |
|
Triglycerides (mg/dL) |
257 |
158.43 |
149.02 |
-9.41* |
-18.02, -0.80
|
|
Note:*pvalue<0.05; **pvalue<0.001; n= participants with complete data on metabolic markers; MD= Mean Difference; CI= Confidence Interval |
|||||
Table 2: Mean change between pre-DEEP and post-DEEP values for the main study outcomes.
Citation:Grant CG1, Lu F, Fleck SB, Kabir UY, Mzayek F and Castillo A (2020) Using Education to Improve Hba1c in Older Adults with Diabetes. J Diabetes ManagMetab: JDMM-10009