Emergency Medicine and Trauma Care Journal
(ISSN 2652-4422)
Case Report
Myocardial Perforation Resulting from Implanted Pacemaker Lead
Gould K*
Department of Emergency Medicine, Virginia Commonwealth University, USA
*Corresponding author: Kevin Gould, Department of Emergency Medicine, Virginia Commonwealth University, USA.
Citation: Gould K (2020) Myocardial Perforation Resulting from Implanted Pacemaker Lead. Emerg Med Truama. EMTCJ-100024
Received date: 11 January, 2020; Accepted date: 20 January, 2020; Published date: 27 January, 2020
Abstract
Perforation of the myocardium by a pacemaker lead is a rare but life-threatening complication of an otherwise life-saving device. Ultrasound is an imaging modality that can be utilized in the Emergency Department to help more quickly diagnose this complication. In our case, a 76-year-old male presents with sharp, intermittent chest pain, one of whose pacemaker leads appears to be perforating his right ventricle on ultrasound. This is confirmed with computed tomography and the patient successfully underwent lead revision with Electrophysiology.
Keywords: Electrophysiology; Radiation; Ultrasound
Introduction
A pacemaker can be a lifesaving device in a patient with a bradyarrhythmia. Common side effects include lead dislodgement, device malfunction and infection [1]. An uncommon, but life-threatening adverse event is ventricular perforation due to a pacemaker lead, as exemplified in our case of a 76-year-old individual who presents to our emergency department with chest pain.
Case Report
A 76-year-old gentleman with a history of sick sinus syndrome, and a dual chamber pacemaker implanted one year prior to presentation, who presented to the emergency department with complaints of chest pain. Patient reported two days of chest pain with acute worsening over the last 24 hours. The patient described the pain as an intermittent sharp 10/10 pain over his left chest without radiation. The discrete episodes lasting seconds and occurring twice daily, to several times an hour. The patient reported generalized weakness over the past 2-3 days, but denies associated nausea, vomiting, dyspnea, or abdominal pain. He was last seen in the cardiology clinic one month prior to presentation, and per a review of the electronic medical record, was found to have a high right ventricle pacing burden but overall normal pacemaker function.
Initial exam revealed an elderly Caucasian male lying in bed, uncomfortable but in no acute distress. Patient is afebrile and normotensive, though intermittently bradycardic, with heart rate oscillating between 30s and 60s. Cardiac exam revealed normal heart sounds without murmur, rub or gallop and intact peripheral perfusion with warm lower extremities and intact peripheral pulses. Patient was alert and oriented to person place and situation with no focal neurologic deficits observed. The patient experienced multiple episodes of sharp chest pain lasting 1 to 2 seconds during the exam. The patient identified the pain to be located left lateral to his sternum, just medial to patient’s point of maximum impulse.
In the emergency department an Electrocardiogram (ECG) showed regular sinus rhythm, bradycardia with heart rate decreased to the 30s, and consistent pacer spikes evident, but not consistently triggering a QRS complex. Pacemaker interrogation in the emergency department found his device to be intermittently pacing with an interval capture. Device voltage was increased, which did not result in increasing capture rate see Figure 1. A bedside echo showed a dual chamber device with two visible leads, with the right ventricular lead appearing to terminate beyond the plane of the right ventricular apex, potentially perforating the right ventricle wall see Figure 2. Confirmatory Computed tomography (CT) scan of the chest with contrast revealed a left-sided two lead pacemaker device with one lead terminating in the right atrial appendage, and the second terminating past the right ventricular apical myocardium, with a trace cardiac effusion see Figure 3. The patient was subsequently admitted to the cardiac intensive care unit for further management and underwent pacemaker lead revision with cardiac electrophysiology.
Discussion
Myocardial perforation resulting from pacemaker leads is a rare complication with an incidence of <1% [2]. Early diagnosis is critical, as this condition can lead to pericardial effusion, cardiac tamponade and death [3]. In this case of a 76-year-old gentleman, the identifying factors leading to diagnosis were sharp intermittent chest pain, episodes of significant bradycardia, and initial ECG suggesting interval pacing capture. Choice of imaging modality is important to identify potential pericardial effusions or intra-thoracic bleeding. Studies have shown CT imaging to be superior, with accuracy or 92.9% (sensitivity 100% and specify of 84.5%) compared to transthoracic echo with an accuracy of 62.7% (sensitivity 41.2% and specificity 84.2%) [4].
Conclusion
Here we describe a possible presentation of a patient with rare complication from pacemaker implantation. In the Emergency department setting early diagnosis is critical, and choice of diagnostic modality offers benefits and draw backs. Though CT is shown to have a higher accuracy in identifying potential pacemaker lead complications, bedside ultrasound still has a role in diagnosis, as it is faster to perform and easier to obtain than a CT chest in a patient who may potentially have a myocardial perforation. Definitive treatment is lead revision and replacement.
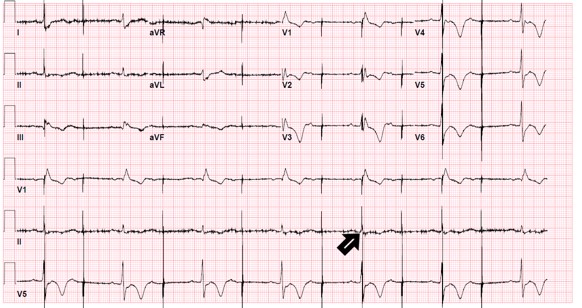
Figure 1: Electrocardiogram showing start of capture.

Figure 2: Ultrasound showing perforation of wire into right ventricle.
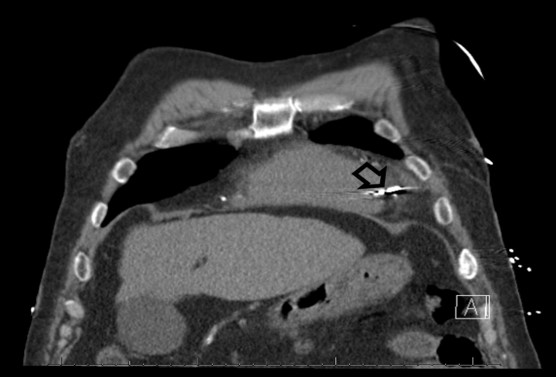
Figure 3: Chest Computed Tomography showing perforation of wire through right ventricle.
Citation: Gould K (2020) Myocardial Perforation Resulting from Implanted Pacemaker Lead. Emerg Med Truama. EMTCJ-100024