Clinical Oncology Research Journal
(ISSN 2652-4457)
Research Article
Concurrent Procedure of Primary Tumor Biopsy Using Endobronchial Ultrasound Combined with Navigational Bronchoscopy and Lymph Node Stage Using Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration in Lung Cancer Patients with Concomitant Peripheral and Mediastinal Lesions
Otsuki A1*, Misawa M2, Tsuzuki R3, Nakashima K1 and Aoshima M1
1Department of Pulmonology, Kameda Medical Center, Japan
2Department of Pulmonology, Shonan Kamakura General Hospital, Japan
3Department of Allergy and Respiratory Medicine, The Fraternity Memorial Hospital, Japan
1Department of Pulmonology, Kameda Medical Center, Japan
1Department of Pulmonology, Kameda Medical Center, Japan
*Corresponding author: Ayumu Otsuki, Department of Pulmonology, Kameda Medical Center, 929 Higashi-cho, Kamogawa, Chiba, Japan.
Citation: Ayumu O, Masafumi M, Ryuta T, Kei N, and Masahiro A (2019) Concurrent Procedure of Primary Tumor Biopsy Using Endobronchial Ultrasound Combined with Navigational Bronchoscopy and Lymph Node Stage Using Endobronchial Ultrasound-Guided Trans bronchial Needle Aspiration in Lung Cancer Patients with Concomitant Peripheral and Mediastinal Lesions. Clin Oncol Res J: CORJ-100008.
Received date: 24 December, 2019; Accepted date: 31 December, 2019; Published date: 7 January, 2020
Abstract
Objective: Recently, transbronchial biopsy (TBB) using virtual bronchoscopic navigation (VBN) combined with radial endobronchial ultrasound with a guide sheath (TBB with VBN-EBUS-GS) has improved the diagnostic yield of small peripheral lung cancer (PLC). Owing to these procedures, the examination time of TBB for PLC has been shortened in our institution. Further, we have been performing TBB with VBN-EBUS-GS for PLC and EBUS-guided transbronchial needle aspiration (EBUS-TBNA) for lymph node (LN) staging concurrently. However, an evaluation of these procedures performed concurrently has not been reported. Therefore, we aimed to evaluate the effectiveness and safety of this one-stage combined procedure.
Methods: We retrospectively assessed 33 cases of lung cancer patients who underwent TBB with VBN-EBUS-GS for PLC and EBUS-TBNA for LN staging concurrently (one-stage procedure) and 31 cases where the procedures were performed on two days (two-stage procedure) from January 2012 to May 2016. The primary endpoints were the diagnostic accuracy of PLC, total number of LNs sampled, and number of LN stations punctured.
Results: Between the one- and two-stage procedures, patient characteristics, diagnostic accuracy (78.8% vs. 87.1%, p=0.512), and the median number of LN stations punctured (1.0 LN station vs. 1.0 LN station, p=0.218) were not significantly different. Total examination time (41.0 min vs. 52.0 min, p<0.001) and the median dose of midazolam per procedure (2.0 mg vs. 2.5 mg. p=0.013) were significantly different between the groups. There were three complications overall.
Conclusion: The one-stage procedure seemed to be equally effective and safer.
Keywords: Bronchoscopy; Lung cancer; Staging; Transbronchial biopsy
Introduction
The incidence rate of lung cancer is increasing, although recent advances in the treatment of lung cancer are remarkable [1]. Pathological diagnosis and lymph node (LN) staging of lung cancer are crucial for personalized therapy for patients with this disease. In recent years, endobronchial ultrasound combined with a guide sheath (EBUS-GS) for peripheral lung cancer (PLC) has been widely performed, and EBUS-GS has improved the diagnostic accuracy of PLC [2-6]. In addition, virtual bronchoscopic navigation (VBN) has been introduced [7] and transbronchial biopsy (TBB), using VBN combined with EBUS-GS (TBB with VBN-EBUS-GS), has shown a high diagnostic yield for PLC [8,9]. Furthermore, endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) has improved the accuracy of LN staging for lung cancer [10-12]. Thus, TBB with VBN-EBUS-GS and EBUS-TBNA have been widely performed. However, bronchoscopy has the limitation of a long examination time due to the limited duration of anaesthesia and sedatives. Hence, each procedure has typically been performed on different days. In our institution, there are limits on the number of bronchoscopies that are possible to complete in a day, so it is difficult to postpone hospitalization to undergo another bronchoscopic procedure. In addition, some patients are recommended not to undergo bronchoscopic biopsy for two consecutive days because of administration of anticoagulants or antiplatelet agents. These patients are recommended to undergo TBB with VBN-EBUS-GS and EBUS-TBNA concurrently.
In our institution, we started using TBB with VBN-EBUS-GS and EBUS-TBNA in 2010. Since then, the diagnostic accuracy of PLC has been getting better and the examination time of TBB with VBN-EBUS-GS and EBUS-TBNA has been decreasing each year owing to improvements of operators’ skills. The objective of the present study is to evaluate the effectiveness and safety of the one-stage procedure for concomitant PLC and suspected LN metastases by comparing it to results from patients who underwent the two procedures on different days. We summarize our experiences of 64 patients with concomitant PLC and suspected LN metastases, 33 of whom underwent the one-stage procedure of TBB with VBN-EBUS-GS and EBUS-TBNA and 31 of whom underwent both procedures on two different days at Kameda Medical Center in Japan.
Materials and Methods
We retrospectively enrolled 33 patients with lung cancer who underwent TBB with VBN-EBUS-GS for PLC and EBUS-TBNA for LN staging concurrently (one-stage procedure) from January 2012 to May 2016 at the Department of Pulmonology at Kameda Medical Center in Chiba, Japan. For a comparison group, we retrospectively enrolled 31 patients with lung cancer who underwent the two procedures on different days (two-stage procedure). The bronchoscopy operator chose either the one- or two-stage procedure for each patient. Characteristics of the primary lesion, diameter of the major axis of the primary tumor, and the minor axis of the sampled LN were measured using the most recent high-resolution computed tomography (HRCT). This study was performed in accordance with the principles of the Declaration of Helsinki. This human study was approved by the Institutional Review Board of Kameda Medical Center (approval: 16-103). The requirement for informed consent was waived due to the retrospective nature of this study. The authors have no conflicts of interest to declare.
Anaesthesia: First, 8 ml of 2% lidocaine was sprayed as a local pharyngolaryngeal anaesthesia and all patients were then sedated with an individually calculated dose of intravenous midazolam and pethidine. During the bronchoscopic procedure, 2% lidocaine was added through the working channel to the bronchi and intravenous administration of midazolam or pethidine was added as needed.
Diagnostic protocol of TBB with VBN-EBUS-GS: The detailed protocol for TBB using VBN-EBUS-GS was described previously [13]. TBB with VBN-EBUS-GS was performed with a BF TYPE 1T260?R (Olympus Ltd, Tokyo, Japan) or BF TYPE P260?R (Olympus Ltd). A guide sheath kit (K-201?R or K-203?R, Olympus Ltd) were used in combination with a Radial-EBUS (R-EBUS) probe (UM-S20-17S?R, Olympus Ltd). Regarding VBN, either LungPoint?R (Broncus Ltd, Mountain View, CA, USA) (Figure 1) or Ziostation2?R (Ziosoft Ltd, Tokyo, Japan) (Figure 2) was used for navigating the bronchial pathway to the PLC.
After we performed anaesthesia, the video-bronchoscope was inserted under guidance of VBN. When the tip of the video-bronchoscope reached the targeted bronchus near the PLC, the R-EBUS probe was inserted into a guide sheath (GS) and the GS-covered R-EBUS probe was inserted through the working channel. The probe was advanced to the PLC using R-EBUS images and fluoroscopic guidance. When the GS-covered R-EBUS probe reached the PLC, only the R-EBUS probe was removed, and the GS remained in the PLC. Biopsy forceps or a brush was inserted through the GS and we obtained some specimens. R-EBUS images were grouped into 4 patterns: ‘within’, ‘adjacent to’, ‘blizzard’, and ‘invisible’ [14].
Diagnostic protocol of EBUS-TBNA: The detailed protocol for EBUS-TBNA was described previously [15,16]. EBUS-TBNA was performed with BF TYPE UC260FW?R (Olympus Ltd). The single-use EBUS-TBNA aspiration needles that we used were the NA-201SX-4022?R and NA-201SX-4021?R (Olympus Ltd), and the universal ultrasound processor was the EU-ME1?R (Olympus Ltd). Before EBUS-TBNA, we detected the LNs suspected as metastatic using the latest CT and F-18 fluorodeoxyglucose positron emission tomography. After we performed anaesthesia, a convex probe EBUS (CP-EBUS) equipped with a video-bronchoscope was inserted. We assessed each suspected metastatic LN using ultrasound. As a rule, the LN nearest to the PLC should be assessed first (N1 → N2→ N3). When the CP-EBUS equipped with the video-bronchoscope was located near the target LN, we performed a doppler examination and determined the location of needle insertion. Target LNs were punctured with the needle and we obtained some specimens. As a rule, the LN most distant to the tumor must be targeted first (N3 → N2 → N1).
Diagnostic protocol of one-stage procedure of TBB with VBN-EBUS-GS and EBUS-TBNA: First, we performed EBUS-TBNA as described above. Following EBUS-TBNA, the video-bronchoscope was changed and we performed TBB with VBN-EBUS-GS as described above. Local pharyngeal anaesthesia was performed only once before EBUS-TBNA, but intravenous administration of midazolam or pethidine was added as needed.
Diagnostic protocol of two-stage procedure of TBB with VBN-EBUS-GS and EBUS-TBNA: First, we performed EBUS-TBNA as described above. Following EBUS-TBNA, the patients stayed at our institution and the next day we performed TBB with VBN-EBUS-GS as described above. Local pharyngeal anaesthesia and intravenous administration of midazolam or pethidine was performed each day. If we performed TBB with VBN-EBUS-GS on the first day, we performed EBUS-TBNA on the next day.
Study endpoints and statistics: The primary endpoints were the diagnostic accuracy of PLC, total number of LNs sampled, and number of LN stations punctured. The secondary endpoints were the effectiveness, safety of the examination and the dose of midazolam and pethidine per procedure (midazolam/procedure, pethidine/procedure). The effectiveness of the examination was assessed by R-EBUS findings, number of biopsies, and total examination time. Safety was evaluated by the number of complications. Categorical variables are shown as percentages (%) and continuous variables are shown as medians (interquartile range [IQR]). Categorical variables were analysed using Fisher’s exact test. Continuous variables were analysed using the Mann-Whitney U test. A p value of <0.05 was considered statistically significant. Statistical analyses were performed using the R software package.
Results
Table 1 shows the patient characteristics of the one- and two-stage procedures. In the one-stage procedure, the median (IQR) age was 72 (66-74) years; 25 (75.8%) patients were males. In the two-stage procedure, the median (IQR) age was 72 (66-78) years; 20 (64.5%) patients were male. In the one-stage procedure, the most common location of the primary lesion was the right upper lobe; however, in the two-stage procedure, the right lower lobe was the most common location. In both groups, the most common characteristic of the primary lesions in HRCT was a solid appearance and the most common final pathological diagnosis was adenocarcinoma. The median (IQR) diameter of the major axis of the primary tumor was 31.6 (21.8-45.0) mm in the one-stage procedure and 38.0 (24.0-57.0) mm in the two-stage procedure. The median (IQR) diameter of the minor axis of the sampled LN was 10.5 (9.0-13.0) mm in the one-stage procedure and 9.0 (7.8-11.7) mm in the two-stage procedure. There were no significant differences between the groups for patient characteristics.
Categorical variables are shown as number (%) and continuous variables are shown as median (IQR), unless otherwise indicated. HRCT; High-resolusion computed tomography, GGN; Ground-glass nodule, LN; Lymph node IQR; interquartile range
Table 2 shows outcomes between the one- and two-stage procedures. The findings highlighted below are shown as (one-stage vs. two-stage). The differences in diagnostic accuracy (78.8 % vs. 87.1 %, p=0.512) and the median number of LN stations punctured (1.0 LN station vs. 1.0 LN station, p=0.218) between the groups were not significant. But the difference in the median total number of LNs sampled in both groups was significant (2 sampled vs. 3 sampled, p=0.006). The difference in the rate of the ‘within’ pattern in R-EBUS findings was significant (26 [78.8%] vs. 29 [93.6%], p=0.025), but the difference in the median number of biopsies was not significant (5 vs. 6, p=0.133). The difference in the median dose of midazolam/procedure was significant (2.0 mg vs. 2.5 mg, p=0.013). There were three complications (two haemorrhages and one hypotension) in total, but none of these were severe.
Categorical variables are shown as number (%) and continuous variables are shown as median (interquartile range, IQR), unless otherwise indicated.
VBN; Virtual Bronchoscopic Navigation, R-EBUS; Radial Endobronchial Ultrasound, GS; Guide Sheath, TBNA; Transbronchial Needle Aspiration, LN; Lymph Node
Discussion
The difference in the rates of the ‘within’ pattern in R-EBUS findings between the one- and two-stage procedure was significant. In the one-stage procedure, the most common location of primary lesion was the right upper lobe, which was different in the two-stage procedure. The difference in the rates of the ‘within’ pattern in R-EBUS might have occurred because it is difficult to reach lesions and manoeuver in the right upper lobe [17]. However, the ‘within’ and ‘adjacent to’ patterns in the R-EBUS findings were 32 (97.0%) and 29 (93.6%) respectively in this study. The detection rate of PLC was similar in both groups, and the differences in the median number of biopsies and diagnostic accuracy between the groups were not significant. In a previous study, the diagnostic accuracy of a malignant lesion was 85.2% [6]. Altogether, these findings suggest that the one-stage procedure is not inferior to the two-stage procedure in terms of TBB with VBN-EBUS-GS.
Although we did not find a difference in the median number of LN stations punctured, the median total number of LNs sampled was significantly different between the groups. In a previous study, when the average number of mediastinal LNs sampled by EBUS-TBNA was 3, there were no significant differences between EBUS-TBNA and mediastinoscopy in determining the true pathologic mediastinal LN stage [18]. According to our findings, the number of LNs sampled in the one-stage procedure was similar to the two-stage procedure, and there was no case in the one-stage procedure where EBUS-TBNA was discontinued because of the limitation of anaesthesia. Hence it appears that EBUS-TBNA in the one-stage procedure was a feasible procedure.
Regarding premedication during bronchoscopy, the difference in the median dose of pethidine/procedure between the groups was not significant, but there was a significant difference in the median dose of midazolam/procedure. The loading dose of midazolam should be 0.075 mg/kg for men aged <65 years and women aged <70 years, while a dose of 0.05 mg/kg should be administered to men aged >66 years and women aged >71 years [19,20]. The dose of midazolam in our institution was almost less than 0.05 mg/kg, so an overdose was rarely administered.
In the study, there were three complications, but none of them was severe. Among the 64 cases in the study, there were two cases (3.12%) of haemorrhage and one case (1.56%) of hypotension. A previous study noted that haemorrhage can be a complication of bronchoscopy (0.73-2.8%) [21]. The rate of complications in our institution was similar to what has been previously reported. Hence, we concluded that TBB with VBN-EBUS-GS and EBUS-TBNA in the one-stage procedure can be performed safely.
Despite the benefits of the one-stage procedure, there are two main problems. Firstly, the examination time has a limitation because of the duration of anaesthesia. In the one-stage procedure, the exchange time for the video-bronchoscope was included in the examination time in the study. However, the exchange time for the video-bronchoscope was not measured, so we do not know how long its duration was but the video-bronchoscope needed to be exchanged quickly. Before the one-stage procedure, we had to contact the medical technologist and prepare the video-bronchoscope ahead of time. Therefore, it is important that the bronchoscopy is performed by experienced pulmonologists in order to obtain the specimens quickly and precisely in the one-stage procedure.
The second problem involves the health insurance system. In Japan, a flat-fee-payment system called the Diagnosis Procedure Combination (DPC) is applied to individual treatment services. According to this system, EBUS-TBNA is 5500 points and TBB with EBUS-GS (with VBN) is 5300 points. In the one-stage procedure, we performed TBB with EBUS-GS and EBUS-TBNA on the same day, but only the points of EBUS-TBNA were charged, based on a DPC rule. Therefore, with the one-stage procedure, our institution loses an examination fee. This is why we needed to carefully select cases in which the patient underwent TBB with VBN-EBUS-GS and EBUS-TBNA on the same day.
In our institution, there are limits to how many bronchoscopies can be performed in a day, but the number of required bronchoscopy procedures is increasing each year. This makes it difficult to postpone hospitalization to perform another bronchoscopic procedure. Because of this, it is beneficial to perform TBB with VBN-EBUS-GS and EBUS-TBNA on the same day. In older patients, conditions such as cardiovascular disease are more prevalent. These patients are more likely to take anticoagulant agents or antiplatelet drugs. Clopidogrel, for example, increases the risk of bleeding after bronchoscopy [22]. Therefore, the Japan Society for Respiratory Endoscopy recommends that anticoagulant agents or antiplatelet agents be withdrawn before invasive procedures like bronchoscopy. Since the cessation of these drugs can worsen a patient’s condition, the one-stage procedure is recommended in these cases because of its shorter duration.
This study has several limitations. As this study was retrospective, a small number of experienced pulmonologists performed bronchoscopy only in our institution. Different pulmonologists working in other institutions would have an effect on the examination time and the diagnostic accuracy of bronchoscopy. Notably, almost all patients with locally advanced stage ? non-small cell lung cancer who underwent EBUS-TBNA for LN staging, also underwent induction chemo-radiotherapy following surgery. For this reason, we could not assess the diagnostic accuracy of the LN metastases.
Conclusion
This study was the first to evaluate the effectiveness and safety of the one-stage combined procedure compared to the two-stage procedure in bronchoscopy. The one-stage procedure in bronchoscopy seemed to be equally effective and safer. Patients also had the benefit of a pathological diagnosis for PLC and LN staging confirmed simultaneously.
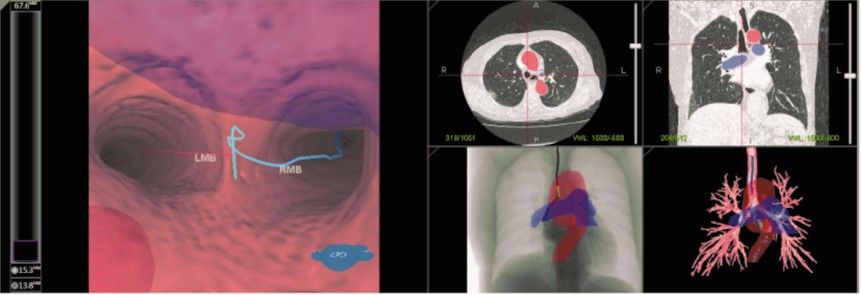
Figure 1: Virtual bronchoscopic navigation (LungPointR) in our institution. These virtual images are from a method which indicates the bronchial path to a peripheral lesion.
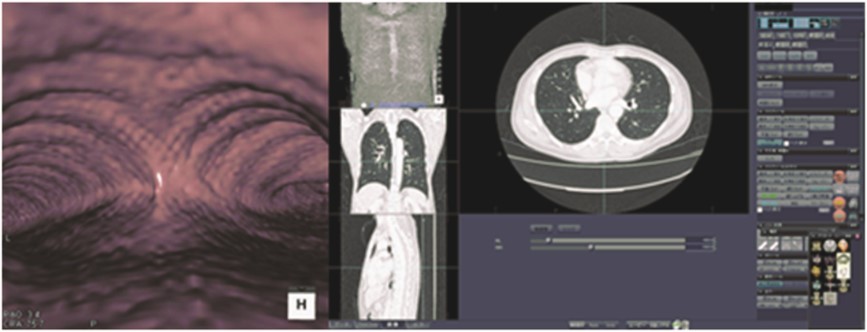
Figure 2: Virtual bronchoscopic navigation (Ziostation2?R).
|
- |
One-stage procedure N=33 |
Two-stage procedure N=31 |
p value - |
|
Age (years) |
72 (66-74) |
72 (66-78) |
0.585 |
|
Gender |
- |
- |
0.415 |
|
Male |
25 (75.8) |
20 (64.5) |
- |
|
Female |
8 (24.2) |
11 (35.5) |
- |
|
Smoking history |
- |
- |
0.614 |
|
Positive |
30 (90.9) |
30 (96.8) |
- |
|
Negative |
3 (9.1) |
1 (3.2) |
- |
|
Location of primary lesion |
- |
- |
0.416 |
|
Right upper lobe |
14 (42.4) |
10 (32.3) |
- |
|
Right middle lobe |
3 (9.1) |
0 (0.0) |
- |
|
Right lower lobe |
9 (27.3) |
11 (35.5) |
- |
|
Left upper lobe |
4 (12.1) |
5 (16.1) |
- |
|
Left lower lobe |
3 (9.1) |
5 (16.1) |
- |
|
Characteristics of the primary tumor in HRCT |
- |
- |
1 |
|
Solid |
30 (90.9) |
29 (93.6) |
- |
|
Pure GGN |
0 (0.0) |
1 (3.2) |
- |
|
Mixed GGN |
2 (6.1) |
1 (3.2) |
- |
|
Other |
1 (3.0) |
0 (0.0) |
- |
|
Diameter of the major axis of the primary tumor (mm) |
31.6 (21.8-45.0) |
38.0 (24.0-57.0) |
0.132 |
|
Diameter of the minor axis of the sampled LNs (mm) |
10.5 (9.0-13.0) |
9.0 (7.8-11.7) |
0.072 |
|
Final pathology |
- |
- |
1 |
|
Adenocarcinoma |
19 (57.6) |
18 (58.1) |
- |
|
Squamous cell carcinoma |
10 (30.2) |
11 (35.5) |
- |
|
Small cell carcinoma |
2 (6.1) |
1 (3.2) |
- |
|
Other |
2 (6.1) |
1 (3.2) |
- |
Table 1: Characteristics of patients who underwent one- and two-stage procedures.
|
- |
One-stage procedure |
Two-stage procedure |
p value |
|
N=33 |
N=31 |
- |
|
|
Outcomes of VBN-EBUS-GS |
|||
|
Diagnostic accuracy (%) |
78.8 |
87.1 |
0.512 |
|
R-EBUS findings |
|
|
0.025 |
|
Within |
26 (78.8) |
29 (93.6) |
- |
|
Adjacent to |
6 (18.2) |
0 (0.0) |
- |
|
Blizzard |
0 (0.0) |
1 (3.2) |
- |
|
Invisible |
1 (3.0) |
1 (3.2) |
- |
|
Number of biopsies |
5 (5-7) |
6 (5-7) |
0.133 |
|
Outcomes of EBUS-TBNA |
|||
|
Total number of LNs sampled |
2.0 (2.0-2.0) |
3.0 (2.0-3.0) |
0.006 |
|
Number of LN stations punctured |
1.0 (1.0-2.0) |
1.0 (1.0-2.0) |
0.218 |
|
Outcomes of procedure |
|||
|
Total examination time (min) |
41.0 (37.0-50.0) |
52.0 (45.5-64.0) |
<0.001 |
|
Pethidine/procedure (mg) |
35.0 (35.0-35.0) |
35.0 (35.0-35.0) |
0.48 |
|
Midazolam/procedure (mg) |
2.0 (2.0-2.0) |
2.5 (2.0-3.0) |
0.013 |
|
Number of complications |
1 (3.0) |
2 (6.4) |
0.607 |
Table 2: Outcomes between patients who underwent one- and two-stage procedures.
Citation: Ayumu O, Masafumi M, Ryuta T, Kei N, and Masahiro A (2019) Concurrent Procedure of Primary Tumor Biopsy Using Endobronchial Ultrasound Combined with Navigational Bronchoscopy and Lymph Node Stage Using Endobronchial Ultrasound-Guided Trans bronchial Needle Aspiration in Lung Cancer Patients with Concomitant Peripheral and Mediastinal Lesions. Clin Oncol Res J: CORJ-100008.