Journal of Urology and Renal Problems
Case Reports
Scrotal Skin Cover for Penile Skin Loss Secondary to Penile Cellulitis-A Case Report
Dinesh H Kittur1, Sudhakar Jadhav2, Santosh Patil2, Kant Shah2, Kailas Bhandarkar2,3,*
1Ankur PediatricSurgical Clinic, Rajarampuri Kolhapur, Maharashtra, India
2*SJKC Trust’s Paediatric Surgery Centre & Postgraduate Institute, Sangli, Maharashtra, India
3*Evelina London Children’s Hospital, Westminster Bridge Road, Lambeth, London,United Kingdom
*Corresponding author:Kailas Bhandarkar, Evelina London Children’s Hospital, Westminster Bridge Road, Lambeth, London,United Kingdom.
Citation: Bhandarkar K, Kittur DH, Jadhav S, Patil S, Shah K (2020) Scrotal Skin Cover for Penile Skin Loss Secondary to Penile Cellulitis-A Case Report.J Urol Ren Probl: JURP-100001.
Received Date: 16 November, 2019; Accepted Date: 23 December, 2019; Published Date: 22 January, 2020
Abstract
Penile skin lossusually followsindustrial accident, or fournier’s gangrene. This is a report of an eleven year old boy who presented with Type I diabetes and severe penile cellulitis with sepsis which eventually led to loss of glans and the whole of the penile skin due to gangrene. After control of his diabetes and infection, the penis was given a cover of scrotal skin in two stages, under cover of a suprapubic cystostomy. The patient made an good recovery and had an excellent cosmetic outcome.
At five year follow up, his diabetes is under control and the repaired penile skin cover is healthy. He does not have any urinary symptoms. His main concern is the short penile length, for which he has been counselled.
Keywords:Fournier’s gangrene, Penile sepsis, Penile skin reconstruction, Scrotal skin cover for penile skin loss
Introduction
Penile skin loss is commonly reported in adults following an industrial accident, where the scrotal skin also gets avulsed [1]. Loss of penile skin has been reported both in adults as well as children following fournier’s gangrene[2,3]. Various methods have been used to cover the defect which include skin of the forearm, inguinal region, scrotum and the thigh. We report a case of a type I diabetic child who had loss of glans and penile skin following severe infection and urinary tract infection. The bare penis was provided with a skin cover using the scrotal skin, in two stages using a very simple method.
Case report
This is a report of a circumcised eleven year old boy who was admitted with penile cellulitis and darkeningcolour of the glans and purulent discharge from the penile skin. Investigations revealed that he had type I diabetes, UTI and pus culture revealed E Coli sensitive to Ceftriaxone and Amikacin.
The boy was treated with intravenous insulin, diabetic diet, antibiotics, packed cell transfusion and dressings. After a week, his diabetes was well under control. The glans and the penile skin had become gangrenous. Under general anaesthesia, the penile skin and part of the glans were debrided. The penile shaft was left bare and part of the glans was lost (Figure 1) Suprapubic cystostomy was added. Penile skin was reconstructed in two stages. During the first stage, a rectangular scrotal flap was raised in the midline, under which the penis was buried (Figure 2). The length and the width of the flap was designed bearing in mind the length of penile shaft and half its circumference. The base of the scrotal skin flap was sutured to the penile basal skin from 9’0 clock to 3’0 clock position. Similarly the distal scrotal skin flap edge was sutured to the penile shaft from 9’0 clock to 3’0 clock position. The urethral opening was left exposed. After a week the scrotal skin flap covering the penile shaft was healthy, with no discharge(Figure 3).The patient was sent home for 6 weeks after which he was readmitted for the 2nd stage reconstruction. His haemogram and blood sugar were repeated and confirmed to be within normal limits.
Under general anaesthesia, the flap was raised on either side of the penile shaft and the loose skin wrapped around the ventral side of the shaft and sutured in the midline in two layers with 4.0 polyglactin and polypropylene sutures. The scrotal wound was closed primarily with similar sutures (Figure 4). After ten days when the healing was complete, the suprapubic catheter was removed. The patient did not have any voiding difficulty. He has been on regular follow up and has good control of diabetes. Follow up after 5 years (current age16 years) he has reported good stream of urine and erection episodes. His only anxiety is the small size of his penis. We have counselled him that his penile size is adequate for sexual intercourse.
Discussion
If a child presents with severe sepsis, presence of diabetes though rare should always be entertained. When present, the diabetes should be controlled and debridement should be radical even if it amounts to loss of penile skin. A variety of skin grafts and flaps have been used as a cover for penile skin loss after accidents or iatrogenic injuries[4,5,6].
In our patient a simple flap from scrotal skin was used to cover the bare penis. Scrotal skin has various advantages including proximity, ease of harvesting and laxity which makes it rather ideal for penile skin reconstruction [7]. The method we have described is easy to learn and graft take is also predictable. Scrotal flap is a procedure which is easy and safe, besides providing adequate cosmesis and function. It also offers a large amount of skin with minimal morbidity of donor site.
Conclusion
Penile Skin loss whatever be its cause, needs a skin cover at the earliest. Scrotal skin fulfils all the criteria necessary for an ideal penile flap and can be performed by a Paediatric Surgeon without requiring exceptional skills of a Plastic surgeon.

Figure 1: Intraoperative picture showing the debrided scrotal skin.
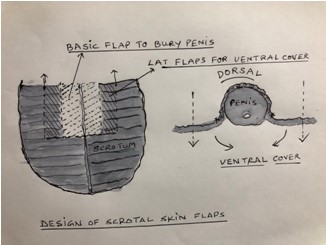
Figure 2: Drawing showing the preparation of skin flaps (see text for details).

Figure 3: Shows early post-postoperative appearance after the first stage procedure.

Figure 4: Intraoperative picture after the second stage.
Citation: Bhandarkar K, Kittur DH, Jadhav S, Patil S, Shah K (2020) Scrotal Skin Cover for Penile Skin Loss Secondary to Penile Cellulitis-A Case Report.J Urol Ren Probl: JURP-100001.