Emergency Medicine and Trauma Care Journal
(ISSN 2652-4422)
Case Report
Anaphylaxis-Induced Kounis Type-I Syndrome Post-Wasp Sting with Dramatic Response to Anti-Shock Measures; A Case Report
Elsayed YMH1*
Critical Care Unit, Fraskour Central Hospital, Damietta Health Affairs, Egyptian Ministry of Health (MOH), Damietta, Egypt
*Corresponding author: Yasser Mohammed Hassanain Elsayed, Critical Care Unit, Fraskour Central Hospital, Damietta Health Affairs, Egyptian Ministry of Health (MOH), Damietta, Egypt, Tel: +00201141292365; Email: dryaser24@yahoo.com
Citation: Elsayed YMH (2020) Anaphylaxis-Induced Kounis Type-I Syndrome Post-Wasp Sting with Dramatic Response to Anti-shock Measures; A Case Report. Emerg Med Truama. EMTCJ-100022
Recevied date: 19 December, 2019; Accepted date: 03 January, 2020; Published date: 10 January, 2020
Abstract
Rationale: Anaphylaxis is a potentially life-threatening, systemic, allergic reaction that requires both immediate recognition and aggressive treatment. Acute coronary syndromes sometimes are allergic in origin that referred to Kounis syndrome. Anaphylactic reactions are usually including; anaphylactic shock and serious allergic mucocutaneous reactions. The most frequent triggers of severe anaphylactic reactions are drugs, insect venoms, and foods.
Patient concerns: A 55-year-old married, housewife, Egyptian female, was admitted to the critical care unit with anaphylactic shock and coronary artery spasm after wasp bite.
Diagnosis: Wasp sting-induced anaphylaxis with coronary vasospasm (Kounis Type-I Syndrome).
Interventions: Echocardiography, ABG, and troponin test.
Lessons: The most interesting point in my case is a dramatic response of an electrocardiographic ST-segment depression for anti-anaphylactic measures. This case report emphasizes both the importance of recognizing the main etiology of coronary vasospasm that was induced by anaphylaxis and manage it. Coronary artery spasm and myocardial injury in the absence of evident preexistent coronary artery disease can occur in the setting of an urticarial reaction. Anti-anaphylactic measures are the known therapy for anaphylaxis but not for coronary artery disease. This case report describes the efficacy of anti-anaphylactic therapies in the normalization of the electrocardiographic coronary artery spasm.
Outcomes: Dramatic response to anti-anaphylactic shock measures with no residuals.
Keywords: Anti-Shock Measures; Anaphylaxis; Induced Kounis type I Syndrome; Wasp Sting
Abbreviations
ABG : Arterial blood gas
CAD : coronary artery disease
ECG : electrocardiography
ICU : intensive care unit
KS : Kounis syndrome
Introduction
Allergic angina: And allergic myocardial infarction are known as Kounis syndrome (KS) [1]. KS first identified by Kounis and Zavras in 1991 [2-4]. Kounis syndrome is a concurrence of acute coronary syndromes associated with mast-cell and platelet activation in the setting of allergic or anaphylactic insults [5]. The pathogenesis of Kounis syndrome is comprising the release of inflammatory cytokines through mast cell activation, which leads to coronary artery vasospasm and/or atheromatous plaque erosion or rupture [3]. Histamine, the main amine released during allergic reactions, can provoke coronary arterial spasm manifested as angina pectoris [2]. Three variants of KS have been described. In type I variant (most common variant, 72.6%), the release of inflammatory mediators induces coronary artery spasm with or without an increase of cardiac enzymes and troponins. In type II variant (22.3%), the release of inflammatory mediators induces coronary artery spasm together with plaque erosion or rupture manifesting as acute MI. Type III variant (5.1%) includes patients with coronary artery stent thrombosis as a result of an allergic reaction. Patients with the type I variant may benefit from the treatment of the allergic reaction, which, by itself, can resolve the cardiac manifestation [6].
Anaphylaxis: Is an acute systemic reaction with symptoms of an immediate-type allergic reaction which can involve the whole organism and is potentially life-threatening [7]. Anaphylactic shock is an unexpected, sudden and sometimes deadly event that affects the patient in 75% of the cases without a pre-existent history of allergy [1]. Anaphylaxis is highly likely when any one of the following three criteria is fulfilled:
The most frequent triggers of severe anaphylactic reactions are drugs, insect venoms, and foods [7]. It is well known that anaphylaxis causes systemic vasodilation and decreased venous return secondary to increased vascular permeability and subsequently may lead to a depressed cardiac output, resulting in coronary hypoperfusion and myocardial damage [4]. Serious allergic reactions may be the cause of acute coronary syndrome in patients with healthy or altered coronary arteries and no cardiovascular risk factors [9]. Coronary artery spasm and myocardial injury in the absence of evident preexistent coronary artery disease (CAD) or concurrent systemic hypotension can occur in the setting of an urticarial reaction. Cardiac mast cell degranulation and release of histamine may lead to coronary artery spasm and myocardial injury [10]. However, depending on the location and number of bee stings, previous history of allergic reactions may increase the possibility of severe life-threatening events [1]. Bees venom contains three main allergens: Phospholipase A to which most patients are sensitive, hyaluronidase to which a smaller number are allergic mellitin which is an important allergen in only a few patients [11]. Bee sting envenomation results in a number of clinical presentations: anaphylaxis, generalized urticaria, angioedema, bronchospasm, hypotension, cardiovascular collapse, loss of consciousness, and cardiac ischemia [1].
Vasoactive amines, including histamine, dopamine, and noradrenaline can provoke ischemia and even myocardial infarction through profound hypotension and arrhythmia, or by increasing oxygen demands through direct inotropic and chronotropic effects in the presence of preexisting ischemic heart disease [12]. The most important drug in the acute therapy of anaphylaxis is adrenaline [7]. Rapid administration of epinephrine is lifesaving [13]. Immediate supply of oxygen via an oxygen mask with a reservoir bag is recommended. The supply of large amounts of fluid within a short time is necessary. Dopamine, noradrenaline, and vasopressin are applied in life-threatening situations. The central role of histamine as a mediator of allergic reactions and the efficacy of H1 antagonists in acute urticaria or rhino-conjunctivitis are evident. The only H1 antihistamines registered for intravenous application in the acute treatment of anaphylaxis are the first-generation substances. However, glucocorticosteroids are effective in the treatment of asthma and against protracted or biphasic anaphylactic reactions [7].
Case presentation
A 55-year-old married, housewife, Egyptian female, was presented to the emergency department with severe epigastric pain, dyspnea, tachypnea, and dizziness. The patient had given a history of exposure to wasp sting at the right thumb since about two hours before arrival to the hospital. The patient started to complaining within about two hours of the sting. The initial immediate ECG tracing in the emergency department showed straight ST-segment depressions in the anterior (V3-6), and sagging ST-segment depressions the inferior (II, III, and aVF) leads (Figure 1). On examination, facial swelling with local sting effects was seen on the right thumb area. Angioedema and generalized urticarial hives were noted. His vital signs were as follows: blood pressure of 90/70 mmHg, pulse rate of 98 b/minute, RR of 34b/minute, the temperature of 37.7°C, and O2 sat. (pulse oximetry) of 92%. Tachypnea, dyspnea, and generalized wheeze were the findings on chest examination. No more relevant other clinical data. She was admitted to the critical care unit as anaphylactic shock and coronary artery spasm. The second ECG tracing on ICU admission showed a gradual extension of ST-segment depressions to V1, and V2 leads (Figure 2 A). The third ECG tracing showed normalization of ST-segment in the anterior (V3-6), and still sagging ST-segment depressions of the inferior (II, III, and aVF) leads (Figure 2 B). The fourth ECG tracing showed complete ECG normalization (Figure 2 C). The main differential diagnosis of Kounis syndrome is Takotsubo or stress-induced cardiomyopathy. But the differential diagnosis of Anaphylaxis may be including Vasovagal syncope, cardiogenic shock, cardiac arrhythmia, pulmonary embolism, hyperventilation syndrome, epilepsy, coma, status asthmaticus, acute tracheal/bronchial obstruction, urticaria and hereditary/ acquired angioedema, and toxic substances eg., ethanol, scombroid poisoning, morphine, and Hoigné-syndrome. The patient workup was: ABG and electrolytes profile was done within 15 minutes of admission and start of therapy that showing mild respiratory alkalosis, and hyponatremia (Na+:131 mmol/l), K+:4.3 mmol/L, ICa++:1mmol/L and slight hypoxia. His hemogram was unremarkable. Normal liver and kidney function; SGPT:13 U/L, SGOT:19 U/L, and s. creatinin:1.1 mg/dl. Both CPK-MB and troponin levels were normal. Random blood glucose: 189 mg/dl. Echocardiography showed an absence of hypokinetic abnormalities with a normal ejection fraction (EF:66%). The patient was managed urgently in the intensive care unit with high flow 100 % O2 inhalation, IM adrenaline 0.5 mg of 1:1000, IV hydrocortisone 200 mg, IV chlorpheniramine maleate 20 mg, IV ranitidine 150 mg and IV normal saline 0.9% 1000 ml, and IV Ringer solution 500 ml. Dramatic response of anaphylaxis to anti-anaphylactic measures with clinical and electrocardiographic ST-segment depressions improvement had happened. Standard anti-ischemic drugs were not given. Complete recovery was achieved within three-hours. IV Hydrocortisone 100 mg BID, oral chlorpheniramine maleate 8 mg BID were prescribed on discharge for seven-days with the recommendation for future immunological consultation and follow up.
Discussion
Overview: The current case is anaphylactic shock and coronary artery spasm after wasp bite. Coronary artery spasm is manifested with straight ST-segment depressions in the anterior (V3-6), and sagging ST-segment depressions the inferior (II, III, and aVF) leads. Extension of ST-segment depressions to V1 and V2 leads may indicate increasing the severity of coronary artery spasm. The anaphylactic shock was outlined in the current case with hypotension, relative sinus tachycardia, generalized hives, wheezy chest, and angioedema.
The primary objective: For my case study was the presence of anaphylactic shock and coronary artery spasm after wasp bite.
The secondary objective: For the case study was the dramatic response of electrocardiographic ST-segment depressions or coronary artery spasm for anti-anaphylactic measures.
Limitations of the study: There are no known limitations in the study. I can’t compare the current case with similar conditions. There are no similar or known cases with the same management for near comparison.
Conclusion
Normalization of typical ST-segment depression in serial ECG tracings indicates the presence of coronary artery vasospasm. Our patient was unique in that he yield dramatic improvement of allergic coronary artery vasospasm or Kounis type I syndrome with anti-shock measures. The priority of mangament should be directed to the etiology. It may be vital and critical. We managed our case as anaphylaxis, not as coronary artery vasospasm, but the anti-shock therapies improved both.
Acknowledgment
I wish to thank the critical care unit nurses who make extra ECG copy for helping me.
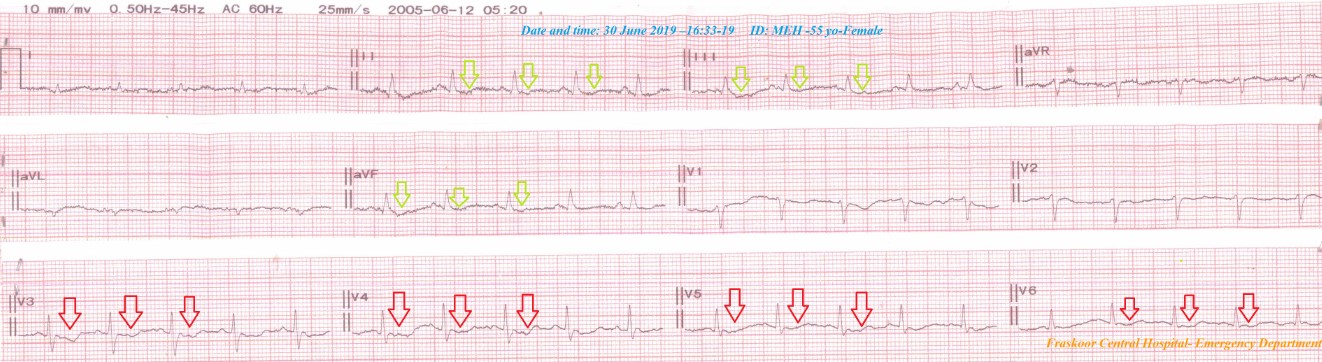
Figure 1: Initial emergency ECG tracing showing straight ST-segment depressions in the anterior; V3-6 leads (red arrows), and sagging ST-segment depressions the inferior; II, III, and aVF (lemon arrows) leads with generalized low-ECG voltage.
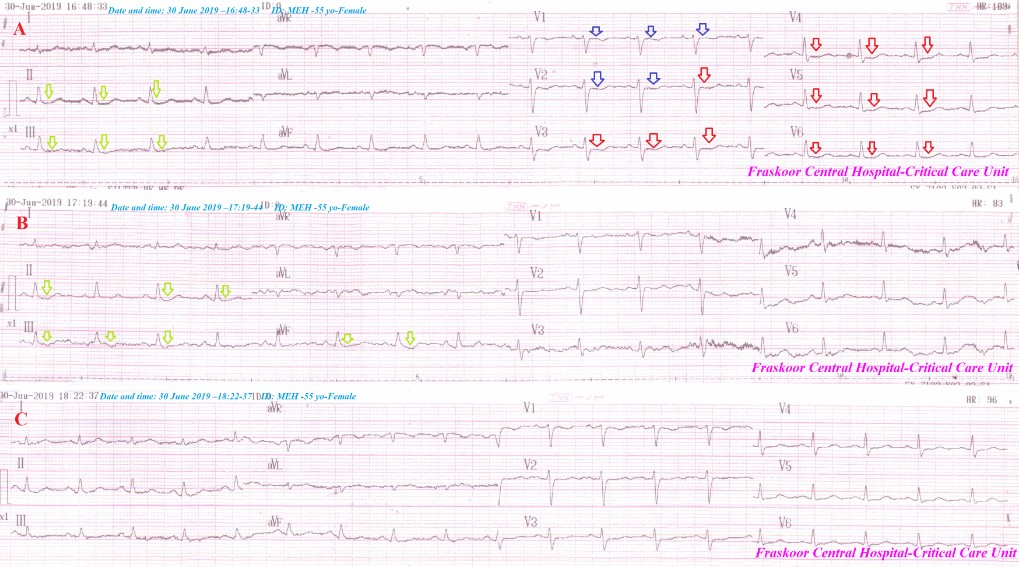
Figure 2: Serial ECG tracings; Initial critical care ECG tracing A was taken within about 15-minutes of emergency ECG tracing; is showing like-figure 1 with the gradual extension of ST-segment depressions to V1, and V2 leads (blue arrows). B; the 3rd ECG tracing was taken within about 30-minutes of starting therapy is showing normalization of ST-segment in the anterior (V3-6), and still sagging ST-segment depressions of the inferior; II, III, and aVF leads (lemon arrows). C; the 4th ECG tracing was taken within about 90-minutes of starting therapy is showing complete electrocardiographic ST-segment depressions normalization.
Citation: Elsayed YMH (2020) Anaphylaxis-Induced Kounis Type-I Syndrome Post-Wasp Sting with Dramatic Response to Anti-shock Measures; A Case Report. Emerg Med Truama. EMTCJ-100022