Emergency Medicine and Trauma Care Journal
Case Report
Traumatic Nonaxial Proptosis - A Rare Case Managed Well
Kaur K1, Gurnani B2*, Mouttapa F3, Yadalla D4 and Kannusamy V5
1DNB Ophthalmology, Aravind Eye Hospital, Thavalakuppam, Cuddalore main road, Pondicherry, India
2DNB Ophthalmology, Aravind Eye Hospital, Thavalakuppam, Cuddalore main road, Pondicherry, India
3DO, DNB Ophthalmology, Aravind Eye Hospital, Thavalakuppam, Cuddalore main road, Pondicherry, India
4MS Ophthalmology, Aravind Eye Hospital, Thavalakuppam, Cuddalore main road, Pondicherry, India
5DO, DNB Ophthalmology, Aravind Eye Hospital, Thavalakuppam, Cuddalore main road, Pondicherry, India
*Corresponding author: Bharat Gurnani, Aravind Eye Hospital, Thavalakuppam, Cuddalore main road, Pondicherry, India, Tel: +919080523059; E mail: drgurnanibharat25@gmail.com
Citation: Kaur K, Gurnani B, Mouttapa F, Yadalla D, Kannusamy V (2019) Traumatic Nonaxial Proptosis - A Rare Case Managed Well. Emerg Med Truama. EMTCJ-100019
Received date: 03 December, 2019; Accepted date: 10 December, 2019; Published date: 17 December, 2019
Abstract
Proptosis in pediatric age group always gives goose bumps to the treating clinician. It often causes a diagnostic dilemma. It is very important to extract as much history as possible along with best examination to reach to a diagnosis. Here we present a similar case of a 9 years old girl who presented with history of increasing proptosis since 10 days. There was history of blunt trauma to forehead 10 days back following which eye became more prominent. Right eye proptosis with scar on brow area was noted. Rest of anterior and posterior segment findings were within normal limits. Ocular movements were normal except right eye elevation restriction. Non contrast computed tomography revealed an extraconal hematoma. This patient was treated with oral steroids and resolution in terms of proptosis and elevation restriction was noted.
Keywords: Diagnosis; Optic nerves; Traumatic nonaxial proptosis
Introduction
Proptosis in children can often present with a diagnostic dilemma [1]. It is important for the examining ophthalmologist to keep in mind a categorised differential diagnosis so that only relevant investigations may be ordered. The first most important part is interaction with patient about onset, progression, any preceding relevant history. Ocular as well systemic examination is important as this might often give an important lead to diagnosis.
Case report
A 9 years old girl who presented with complaints of prominence of right eye (OD) since 10 days associated with pain since 2 days. There was a history of blunt trauma to forehead 10 days back. There was history of gradually increasing prominence of right eye following trauma. Best corrected visual acuity in both eyes (OU) was 6/6. On examination, OD had mild nonaxial proptosis and restricted extraocular movement was noted in upgaze (Figure 1). The lids and rest of adnexa were normal, except abrasion involving brow area. The rest of the ocular examination revealed no abnormality. Colour vision and central fields were normal. Systemic and neurological examination revealed no abnormality.
Non Contrast enhanced Computed Tomography revealed right superior orbital extraconal hematoma measuring 24*12*25mm with compression of right superior rectus and superior oblique muscles with proptosis (Figure 2).
Sagital view showed a clear space between the hematoma and the optic nerve (Figure 3). No destruction of adjacent bones, no intraconal or intracranial extension. Optic nerves showed normal signal intensity, thickness and course.
A diagnosis of extraconal hematoma sparing the optic nerve was made and patient was advised oral cefotaxime (50mg/kg body weight in divided doses 12 hourly) and oral steroids (5mg prednisolone twice daily) under close observation. Patient showed marked improvement within 5 days. The proptosis improved, elevation restriction resolved and patient was symptom free in next 10 days (Figure 4). Oral steroids were slowly tapered over next 1 month.
Discussion
Intraorbital haematoma is a rare clinical entity which can be caused by orbital traumas, neoplasms, surgeries near sinuses and orbit, vascular malformations, systemic abnormalities, barotrauma and valsalva maneuver [2] Subperiosteal hematomas can occur after facial and head trauma and involves rupture of orbital subperiosteal vessels. Spontaneous hematomas are seen in patients with bleeding diathesis [3] or secondary to orbital venous congestion. Rarely they are secondary to frontal sinusitis [4] Most patients present with dystopia, double vision and painful eyeball movement. Our patient had atypical presentation with no such complaints. Based on the imaging findings a diagnosis of extraconal hematoma was made and the patient was managed conservatively on oral antibiotics and steroids, [5] without any active surgical intervention. Why should an emergency physician be aware of this?
Sudden proptosis with a history of trauma and pre-existing prominence can be confusing for the emergency physician. Familiarity with this clinical entity and appropriate investigations can decrease apprehension among patients as well treating physician. Also it is important to note that though presentation might be alarming, careful assessment will help preventing unnecessary intervention.

Figure 1: Clinical photograph of patient showing proptosis of Right eye and restriction of elevation in supraduction.
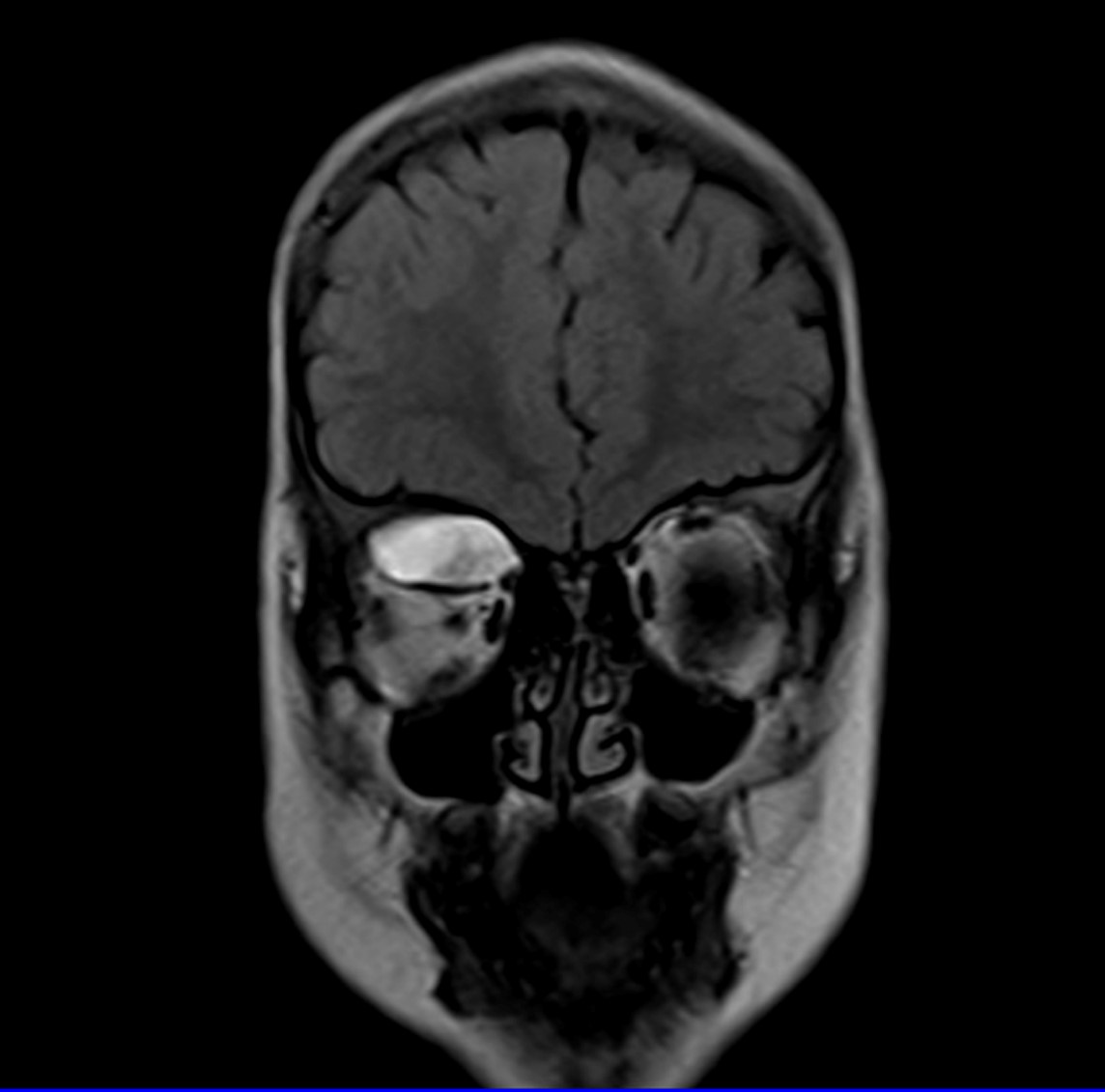
Figure 2: Coronal section MRI scan showing right superior orbital hyperintense well defined mass measuring 24*12*25mm with compression of right superior rectus and superior oblique muscles.
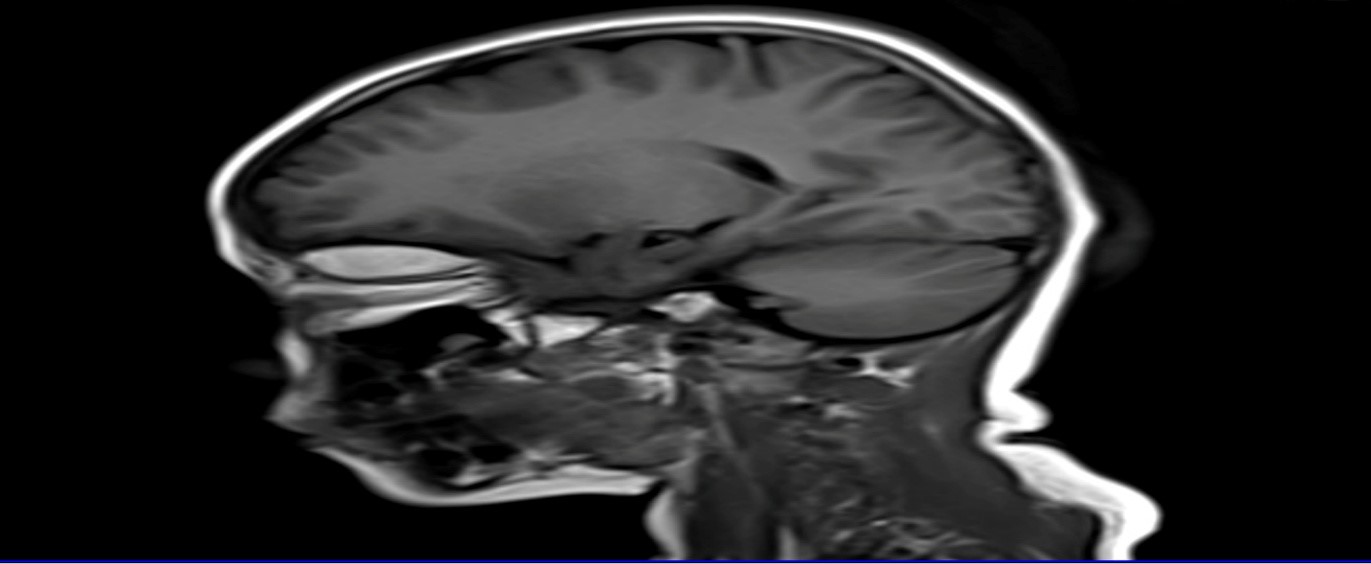
Figure 3: Sagital section of MRI scan showing a well-defined hyperintense mass and a clear intervening space signifying spared optic nerve.

Figure 4: Clinical post treatment photograph of patient showing improvement in supraduction.
Citation: Kaur K, Gurnani B, Mouttapa F, Yadalla D, Kannusamy V (2019) Traumatic Nonaxial Proptosis - A Rare Case Managed Well. Emerg Med Truama. EMTCJ-100019