Journal of Surgery and Insights
Review Article
Quality Improvement in Surgery-An Innovative Project
Anastasiadou S*
Department of Colorectal Surgery, Imperial Healthcare Trust, United Kingdom
*Corresponding author: Sofia Anastasiadou, Department of Colorectal Surgery, Imperial Healthcare Trust, United Kingdom, Tel: +442033113311; Email: sofia.anastasiadou@nhs.net
Citation: Anastasiadou S (2019) Quality Improvement in Surgery-an Innovative Project. J Surg Insights: JSI-100008
Received date: 28 June 2019; Accepted date: 05 July, 2019; Published date: 15 July, 2019
Abstract
Background: Quality improvement is an extremely rapidly evolving science with several aspects to be closely associated with healthcare domain. Especially in surgery, quality improvement projects have been more and more popular in Western World countries. These kinds of projects, offer a basic element of research as well as substantial improvement of how everyday life works in a surgical ward. They ensure patient safety and examine any aspects of care that require review. However, a quality improvement project needs to be well designed and very well communicated to the members of the team in order to be functional. This is where quality improvement science comes to help with various tools and processes to ensure a successful implementation.
Methods: The abscess pathway was observed in Charing Cross Hospital, Imperial Healthcare London and was found inadequate. The article describes a new pathway, based on quality improvement science principles and it discusses how these can be used in various other projects in surgery.
Results: The new abscess pathway is presented and designed with process mapping diagrams, various images and step by step procedures all based on quality improvement science. Eventually, the new pathway is useful and from a quality improvement point of view successfully communicated and implemented.
Conclusion: There is always space for better quality and better designed quality improvement projects. It is extremely important to follow certain rules in order to ensure correct implementation of the project. In this way, patient safety is preserved and their care improvement can be monitored.
Keywords: General anaesthetic; Patient safety; Surgery
Introduction
An abscess is a collection of liquified tissue which is known as pus and it can accumulate anywhere in the human body [1]. Abscess patients are frequent patients in Charing Cross Hospital, Imperial NHS Trust. They can be of both sexes, of various ages with or without comorbidities presenting in different stages of the disease. All patients that present in A&E department of our hospital are seen first by A&E doctors and afterwards they are referred appropriately to the general surgery Senior House Officer (SHO) for review. In continuation, the general surgery SHO decides if the patient needs conservative management or if they require surgical treatment according to their general condition and the progression of the disease. In case the patient requires surgical treatment, they might need an incision and drainage (I+D) under local anaesthetic in which procedure they don’t require admission. However, most of the times the indicative treatment is I+D under general anaesthetic in which case patients need a surgical bed, a pre-operative assessment by the anaesthetic team as well as pre-operative medications and management. They also need to be informed about the details of the operation, sign a consent form and be marked correctly in terms of the surgical site. Post-operatively, they will need time in the recovery area, they will return to their surgical bed and if there are no complications they will be discharged on the same day or later if any unusual event occurs. On discharge, the follow up is done by the general practitioner which means that the patient is discharged completely from the Charing Cross Hospital surgical team care.
Problem Identification
The problem of the abscess management in Charing Cross Hospital is the absence of an abscess pathway. This results in a lot of confusion and problems regarding these patients’ treatment. After it is decided that a patient needs definitive surgical treatment which I+D of the abscess under general anaesthetic, there is no clear guideline regarding the next step to reach this procedure. Indeed, two different paths can be followed after this decision is made. The patient can either be admitted directly or go home and return the next day for their operation (Diagram 1). Both paths have several disadvantages and the application of a global abscess pathway which will show the appropriate management of the abscess patients is necessary. Many surgical units faced the same issue in the past around the UK and there is evidence showing that an abscess pathway has far better results [2,3]. Merging the existing protocols and redesigning a pathway according to Charing Cross Hospital needs ensures better quality of care as well as maintenance of resources.
Background
Let’s have a closer look in what is happening after the general surgery SHO decides on the I+D of an abscess. Most of the patients are in a very good general condition and they are able to go home as they don’t need overnight observation and assessment. However, there are cases in which patients present septic and need immediate admission. These patients join the abscess pathway later on as they are already admitted. In this paper we are discussing the well enough to go home patients which pathway is not determined at all. Normally, they are advised to return to the hospital the following day in early morning hours to wait for a bed as there is no service to book beds in advance. This results in long waiting hours for the patient, who is starved in order to have their operation. They might also not get a bed on that day, they are asked to go home once more and come back two days after their initial presentation in A&E. As a consequence, delays in treatment cause increased risk of sepsis as well as patient frustration and disappointment [4]. This path also puts a lot of pressure to the health professionals responsible for the abscess patients who have returned to the hospital but there is no bed available to accommodate them. It results in highly stressed doctors who are attempting to find a bed urgently in the hospital and are contacting bed managers and senior nurses to make sure they do their best for their patient’s care. Despite that effort, there are still patients who don’t get a bed and need to return twice to the hospital as stated before.
Another aspect of the issue is that the I+D of the abscesses is done in between the emergency cases of Charing Cross Hospital. Consequently, if the patient is not admitted in the hospital, a slot in the emergency operational list cannot be booked for them and they face further delays because of that. As they need anaesthetic assessmentpre-operatively as well, if the patient has no bed, they cannot be assessed causing even more trouble to their treatment. Last but not least, a consent form needs to be filled for each patient, which again needs to be filled after the patient has an allocated bed to ensure that it remains in the patient notes.
This complicated situation has led recently the general surgical SHOs to admit abscess patients on their first presentation even if they don’t need admission, in order to avoid the next day confusion with the available beds, consent forms and slots in the emergency operation list. This solution is not sustainable as it results in unnecessary occupation of valuable surgical beds in a very busy hospital as Charing Cross Hospital. It is not cost effective either as the minimum of one-night stay cost is calculated up to 238£ on a surgical ward [5], which can be easily avoided as most of the abscess patient don’t require admission.
Recommendation
This project introduces an improved abscess pathway, which will include all kinds of abscess patients that present in A&E and are also referred to the general surgery SHO. In order to do that, we need to set specific 1) measurements regarding the baseline before and the outcomes following our intervention. After we have identified the improvement opportunity and having set the measurements, the next step is defining the specific 2) project’s objectives, engaging important 3) stakeholders and inform them regarding the imminent change. 4) A process mapping diagram is vital to enable us to visualise the main pathway steps and identify potential 5) issues that might present while implementing it. In addition, a 6) driver diagram will be designed but an action-effect diagram needs to be considered as well, since there is evidence that the latter is more effective in terms of designing a quality improvement project than the former with regards to healthcare sector [6]. A simple and easily conceivable pathway is essential in order to achieve implementation in every day practice. Appropriate visualisation, basic training on the implementation of the pathway and maybe redesign specific pathway parts according to the stakeholders’ or users’ feedback might be useful on a later stage. The involvement of their feedback will be done according to the alignment model in quality improvement science. The alignment model requires involvement of multiple team members of different teams in decision making and implementation of the project and claims that this encourages teams to maintain the change in practice which makes the actual change much more effective [7]. After completion of the above, the next step is the actual pathway’s use, multiple 7) PDSA cycles and monitoring of the project’s process. Re-auditing the main measurement factors to assess the new intervention is also essential. Data analysis and 8) charts will follow to visualise the effectiveness if any. Taking into consideration the above results, the abscess pathway will be reconsidered, directly applied or even rejected completely.
Measurements
It is important to set the measurements of the intended intervention. All the abscess patients that present in Charing Cross Hospital in a period of a month will be included in an audit which will be focused on quantitative as well as qualitative data. Their length of stay in the hospital (days) and time between their first presentation in A&E and their actual I+D will be measured. Whether or not there was immediately an allocated bed for them when they presented the following day to have their I+D will be also measured. Approximate cost of their treatment will be calculated as well, excluding patients that had post-operative complications which their length of stay will be inevitably prolonged. In addition, they will be given a questionnaire on their discharge to measure the patient satisfaction after their operation is finished. Same measurements will be performed a month after the introduction and use of the abscess pathway and outcomes will be compared. Healthcare professionals involved will be given a questionnaire after the end of the trial period to express their thoughts as well. Consequently, combining the above, the efficacy and value of the abscess pathway will be monitored, and its implementation will be ensured or rejected.
Project’s objectives
The abscess pathway will have a clear objective which is described by the intended outcomes above. It should shorten the length of stay of abscess patients and therefore reduce the costs of their treatment but also increase patient and healthcare professional satisfaction.
Stakeholders
The stakeholders of the abscess pathway are several across the hospital, either from the managerial staff or the doctors and patients themselves. People with high influence and high interest to the project will be the trainees of various levels as well as consultants which will benefit the presence of a proper protocol. High interest but low influence has the financial department which will benefit from shorter hospital stays and shrunk expenses. High interest and moderate influence have the abscess patients themselves, whose care will be optimised with the new pathway, however they can influence it only with their feedback. Considering the stakeholders with low interest and high influence, these are the manager and director of the surgical department who need to approve the change and the implementation of the new pathway in cooperation with the audit department. Last but not least, bed managers, theatre staff and nurses involved in abscess patients care will be notified regarding the new pathway and will be part of the change without major interest or influence. For a graphic description of the above, please refer below to (Table 1).
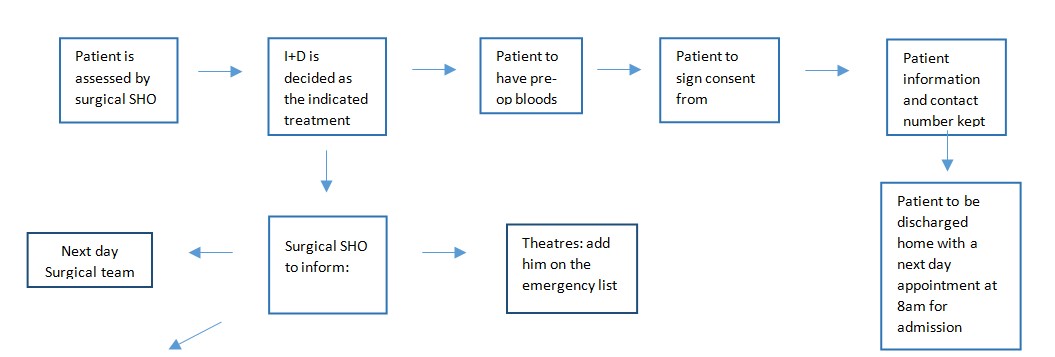
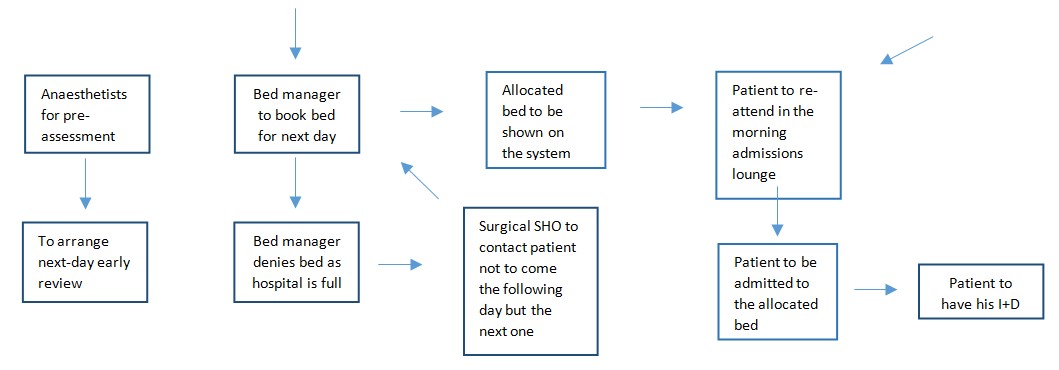
Process Mapping
The abscess pathway intervention requires a process mapping visualisation of the model recommended. The abscess pathway will be designed in an A4 page as a process map and it will include in detail the steps needed for an abscess patient to have his operation promptly. Process mapping is innovative in healthcare quality improvement and provides detailed insights of how systems work, gives information regarding the problematic procedures and points out sections for improvement [8]. The abscess pathway is a very good example of a process mapping implementation in healthcare quality improvement and vice versa, the process mapping is a very effective tool to design and present an abscess pathway [8]. Please refer to the (Diagram 2) below which represents an exact copy of the actual abscess pathway that will be distributed. Copies will be shown in A&E, theatres and surgical wards and they will be also distributed to the managerial staff such as bed and theatre managers at the beginning of their shifts. This will ensure that every person involved is aware of the change that is being implemented.
Potential issues and problems
It is very important to take into consideration common pitfalls and problems that may emerge while trying to make this intervention. To begin with, the existence of the pathway needs to be communicated very well so that everybody that could be involved is aware. This can be achieved by announcing its implementation in surgical meetings in the hospital, managerial gatherings that happen every week and by ensuring that even locum healthcare professionals who do not regularly work in our units know about the protocol. It can be also communicated with printed pathways colourful and catchy for the eye in busy areas around the hospital. Electronic means, such as the intranet home page or computer screensavers when computers are in the waiting mode are also a useful place to announce implementation. Another part of the pathway that needs attention is the patient’s contact information which is essential to notify the patient if eventually there is no bed to accommodate them. In addition, the consent form needs to be signed and kept in the patient’s folder to be ready for the next day emergency operational list. To ensure that, empty consent forms should be available in the surgical assessment units as well as in A&E. Another important part that could be problematic in its implementation is the location of the patient file so that it can be easily found the next day by the surgical team. An allocated shelf only for abscess patients should be named as such in the doctors’ office so that all the filesare accumulated there. Last but not least, communication between the members of all the teams must be ensured for the successful implementation of the pathway. Bed managers should be informed promptly by the SHO and anaesthetists must add early the patient on their assessment list. A slot in the emergency operational list should be booked, even though it can fluctuate afterwards according to the severity of the cases booked. All the above are displayed on the Drivers’ diagram below X.
Driver Diagram
In order to ensure the successful implementation of the abscess pathway we need multiple PDSA (Plan-Do-Study-Act) cycles.
Plan: Identifying the main aspects of the problem, analysing the principle points, understanding the importance and plan the actions to improve the current condition.
Do: Introduce the new abscess pathway, make all the related health professionals aware and start implementation
Study: Audit the new abscess pathway with regards of patient satisfaction and objective measurements such as hospital stay and hospital expenses.
Act: proceed in changes of the pathway if needed and then according to results, implement permanently.
A very simple example of one PDSA cycle is displayed below:
Chart to measure results
All the observed results before and after the implementation of the change will be analysed and visualised on various charts. In this way, data analysis will be simpler and consequently effectiveness of the new abscess pathway will be easily monitored and assessed. A presumed chart which could show the effectiveness of the pathway in terms of length of stay in the hospital and cost before (1) and after the abscess pathway implementation (2) could be as follows:
Conclusion
The abscess pathway is a quality improvement intervention extremely important and necessary for Charing Cross hospital function. It is well known that several pathways are implemented in various hospitals around the country. Having observed some of them and having read reports about others, significant advantages and disadvantages of each one have emerged. After studying the above and analysing their different aspects and their points of failure or success, an observation of the current state-of-art in Charing Cross Hospital was necessary. Ensuring that there is definitely need for change, this specific abscess pathway, summarises all the main steps which are required for an effective abscess treatment. To conclude, quality improvement such as the discussed abscess pathway is crucial for the healthcare sector and has one single critical role; to ensure best quality of care.
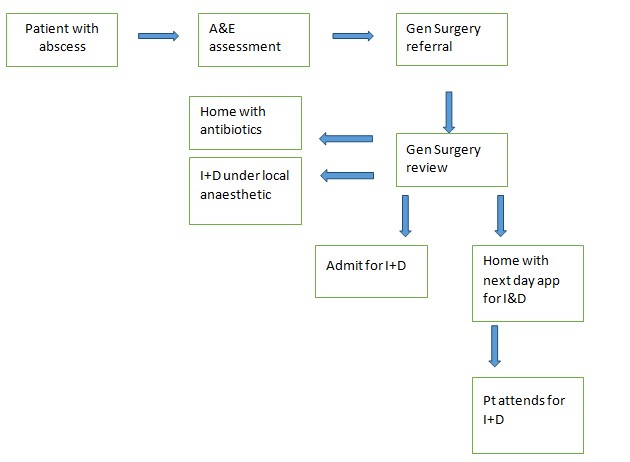
Diagram 1: Current overview of abscess pathway in Charing Cross Hospital.
Plan: All the files should be stored in the allocated shelf in the doctors’ office so that they can be easily found by the next day team. File should include patient notes and the signed consent form.
Do: Inform all the SHOs on shift that the files should be kept in the allocated shelf
Study: Observe if every day the files are in the shelf or forgotten elsewhere and difficult to find (possible that SHO leaves them in A&E because of the stress and load of work).
Act: If everything works according to the plan, no change needs to be done, if thought there are issues regarding the location of the files, reconsideration of the shelf should be done and maybe need to be located elsewhere easier to find.
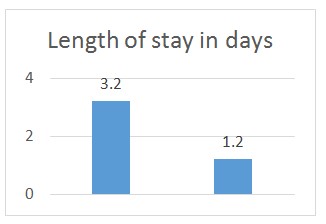
Chart 1: Length of stay
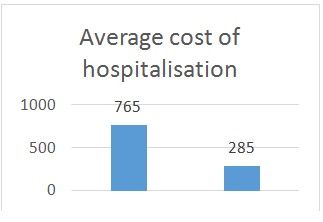
Chart 2: Average cost
|
|
Low interest |
High interest |
|
High influence |
Director of surgical department, Manager of surgical department, Audit department |
Surgical trainees, Surgical consultants |
|
Low influence |
Bed managers, Theatre staff, Nurses involved in abscess care |
Abscess patients Finance department |
Table 1: Principle Stakeholders of the abscess pathway.
|
Outcome |
Primary Drivers |
Secondary Drivers |
|
- |
Bed booked prior to patient arrival |
General surgery SHO Bed manager Admissions lounge |
|
-
|
Consent form in the notes
|
General surgery SHO A&E personnel |
|
Reduce hospital stay and cost Increase patient and healthcare professional satisfaction
|
Notes in the allocated shelf
|
General surgery SHO Next day surgical team |
|
Anaesthetic pre-assessment |
General surgery SHO |
|
|
promptly
|
Anaesthetist
|
|
|
Emergency theatre booking
|
General surgery SHO Theatre manager |
|
|
Call to postpone I+D if no bed available |
General surgery SHO |
Citation: Anastasiadou S (2019) Quality Improvement in Surgery-an Innovative Project. J Surg Insights: JSI-100008.