Journal of Surgery and Insights
Review Article
A New Electronic Health Record
Anastasiadou S*
Department of Colorectal Surgery, Imperial Healthcare Trust, UK
*Corresponding author: Sofia Anastasiadou, Department of Colorectal Surgery, Imperial Healthcare Trust, UK, Tel: +44 20 3311 3311; E-mail: sofia.anastasiadou@nhs.net
Citation: Anastasiadou S (2019)A New Electronic Health Record.J Surg Insights: JSI-100007
Received date:28 June 2019;Accepted date:05 July, 2019;Published date:18 July, 2019
Abstract
Background: It is well known that contemporary health systems including NHS, face various problems, other very crucial or other of minor significance. One of the problems of NHS is documentation that needs improvement in many ways. Innovative technological features could offer a solution on how the documentation is performed. Indeed, limited elements of the available technology are currently used to improve documentation, and contemporary ways to keep notes are in some cases obsolete and ineffective.
Methods: A new electronic health record (EHR) is described which introduces patient profiles with pictures.
Results: A patient profile based electronic system which includes pictures will result in better patient identification, in reduction of medical error and in a more personalised relationship between doctors and patients.
Conclusion: EHRs, as they form the main documentation system currently and they are becoming increasingly popular, they will be definitely influenced by technology in the future in an attempt for improvement. Introducing photographs as well as a detailed profile that contains all patient information uses current technology and improves in an easy and effective way contemporary EHRs.
Keywords: Electronic health record;Patient safety;Healthcare
Introduction
A vast majority of health services have been revolutionised recently with the use of new technological means and discoveries. Implementation of technology innovation in every aspect of health systems aims to deliver better value healthcare and improve patient safety. From one point of view, technology can offer sustainable electronic networks from which both the healthcare professionals and the patients can benefit. Larry Weed, the father of the problem-oriented medical record, stated a long time ago that “since modern information tools can do things that the unaided human mind cannot do, these tools would show us a picture of medicine we have not seen before[1-5].
Current Documentation Standards
It is well known that contemporary health systems including NHS, face various problems, other very crucial or other of minor significance. One of the problems of NHS is documentation that needs improvement in many ways. Innovative technological features could offer a solution on how the documentation is performed. Indeed, limited elements of the available technology are currently used to improve documentation, and contemporary ways to keep notes are in some cases obsolete and ineffective. The way notes are kept nowadays is complicated and information is not easily retrievable which hides various risks threatening the health care system as well as the good medical practice.To be more specific, a lot of NHS Trusts are still using a mix of paper and electronic notes though some of them they have rejected completely paper notes and they have gone “paperless” using Electronic Health Records (EHR). Even in paperless Trusts, the way documentation is performed is still not ideal and the EHRs are not as easy to use as they ought to. To clarify, the layout of a patient’s page is neutral and exactly the same for everyone resulting in a non-personalized EHR that has no difference from patient to patient. Also, the information regarding each patient is limited and the clinician needs excessive effort to convey it which is not always possible in a busy working environment. Given that current EHRs look more like scanned paper that was transferred on screen rather than a user-friendly page, they do not allow easy navigation and often lead to various kinds of mistakes. Though, technology, electronic systems and user interface innovations have much more to offer nowadays[6-10].
Why is it problematic? -Some reasons highlighted
Wrong patient events
To begin with, preventable medical errors, including facility-acquired conditions, is the third leading cause of death in USA and as it appears, millions of patients may experience errors during their hospitalisation. The above certainly reflects poor quality of care and inadequate measures to prevent medical errors. Some of these errors are related to wrong patient events, which means that the wrong person is having an inappropriate treatment or procedure. These errors could happen during several sectors or they can even be escalated to never events. Many authorities have published that the majority of the events that are reported to them is wrong patient related. For example, the Pennsylvania Patient Safety Authority published that in 2009, 30.1% of all the radiology related reported events had dominant the element “wrong patient” (Pennsylvania Patient Safety Authority, 2011). Another systematic review showed that errors in medication administration is partially because of underlying electronic system factors. Only one change is not likely to improve massively the situation as addressing one cause will not be enough. Nevertheless, technology progression and innovation of the documentation systems could offer an opportunity to at least reduce this kind of mistakes and show the way for further changes and improvements.
Doctor-patient relationship
However, there are also other factors that lead to the need for improvement of the current electronic systems. The introduction of EHR has raised concerns about affecting the personal relationship between patients and doctors, leading to non- personal and less human services. The main issue focuses on the fact that nowadays doctors review more the patient EHR rather than the actual person. Since the EHR contains a variety of information regarding each patient, often doctors concentrate on these rather than talking and examining the patient themselves, therefore if the EHR is ineffective or difficult to use, this can lead to severe consequences. One of the concerns is the potential gap between the patient and the doctor, that could create a kind of barrier that can easily contribute to mistakes and negligence. However, there are a lot of studies that suggest equal patient satisfaction with and without electronic patient record use and papers that even suggest doctor’s increasing satisfaction about them. To conclude, there are still concerns regarding the effect of technology on patient-doctor relationship and there is a lot of research to be done as stated to all previous studies. The importance of the above is that electronic medical records’ significance is acknowledged by both clinicians and patients and their improvement is essential to enhance the performance of the first and improve the experience of the latter[11-15].
Layout of current EHRs is extremely demanding
Another downside of the current EHRs is the great amount of information they contain for each patient that is not always well organised and well presented. Consequently, healthcare professionals such as doctors and nurses that use the systems are getting frustrated and susceptible to mistakes. It is true that the use of the systems is time consuming and not effective, as it requires excessive effort and concentration in an already demanding environment. EHRs though, should be helping doctors and nurses rather than requiring extra strain. This represents a current notion that is arising after the increasing worldwide use of EHRs and research is being held on it. Burnout, which is a common term for doctors’ profession has been recently linked to increasing use of electronic patient record systems. A recent study in Stanford University’s School of Medicine has revealed that more than 50% of physicians practicing in the US are experiencing one or more symptoms of the burnout syndrome. This has variable causes but it appears that electronic medical record use holds the most dominant role among the others (Poll, 2018). The above shows once more the importance of EHRs’ improvement and the need to have a friendlier and more effective system that will ensure higher results with less effort and the least of errors[16-20].
It seems that there is no way back
Another reason why effort and resources should be invested in EHRs to become friendlier and easier to use is just because they are here to stay. Who can imagine going back to paper notes, very long patient files, fax machines and letters? There are already new specialties emerging that consist primarily of virtual features and that exploit only EHRs. The “medical virtualise”, an innovative medical specialty based on interactive systems is not far from reality, and doctors that review patients remotely over various applications are increasing. Thus, it is more than obvious that in this page of human history, technology must improve the way healthcare professionals work and improve their practice through currently used EHRs to coordinate the vast amount of data that exist. Therefore, in collaboration with technology innovation, healthcare organisations could innovate their EHRs to achieve good medical practice as well as to ensure patient safety and confidentiality.
What has been done until recently
There has been a lot of new technology implementation on health systems recently aiming to improve current practice. Previously, notes were kept on long patient files, that were difficult to use, challenging to go through and sometimes impossible to retrieve any information from due to illegible handwriting. There was also a major problem regarding sharing information. In 2015, the majority of data breaches that were reported to the Information Commissioner’s Office were in relation with paper notes. Fax machines, the only way to share paper information apart from letters, are particularly susceptible to human errors [21]. In 2015, in Northumbria Healthcare NHS Foundation Trust, 5 faxes were sent by mistake to a member of public and not to the appropriate healthcare professional during a period of a year [16, 22-27]. As stated above, at the minute, most of the NHS Trusts are using a combination of paper and electronic notes attempting to be completely paperless soon. It was announced that NHS would go completely paperless until 2020 by NHS England, though it is informal that such an attempt should be completed until 2027. A very good example of successful technology implementation in everyday practice is the electronic prescribing and medicines administration software (EPMA) that replaced handwritten prescriptions in a vast majority of Trusts in the UK. Although initially there have been studies that suggested there is no difference between handwritten and electronic prescribing mistakes, that was attributed to the lack of training and the new environment that healthcare professionals were challenged to work. As time passed, there is massive evidence finally that EPMA has contributed in evolution of prescription and also led to less prescription related mistakes for inpatient or outpatient prescriptions. Apart from EPMA though, there are certain Trusts around the UK that have rejected paper medical recordsand everything is documented electronically. Even in this case, patient misidentification issues and mistakes regarding patient IDs are prominent as shown in several studies and surveys that have been conducted recently and they can reach up to 24% of mistakes (Institute, 2016). Several measures have been taken to monitor them such as software monitoring of retract and reorder events which imply patient misidentification [28]that are still under investigation of their efficacy.
There have been numerous attempts to improve these systems in terms of ensuring the patient ID by adding for example biometrics of each patient in their personal page. Biometrics were proven to be helpful in reducing medical mistake frequency, in preventing medical fraud, ID theft and also duplicate medical records as well (Trader, 2016) but need still a lot of improvement [29].Proposals have been made for a health “ATM” system, which will ensure secure and private access for both healthcare professionals and patients on a page where all kind of information will be kept and patients will be also able to alter the existing information. However, these are still solutions that have not yet been implemented massively or investigated thoroughly[30-35].
Planning an innovative change
Introducing an electronic system that will consist of patient profiles that apart from all the relevant information will include patient photographs can also be an idea to improve current electronic documentation. Until very recently, photographs in medical practice were used primarily for three reasons: educational, publication and documentation reasons. Photographs have been used to ease communication between doctors, avoid painful re-examination and also keep records between reconstructive operations.
Patient identification could also be a significant reason why photos should be introduced in electronic medical records of a patient. Since ways such as biometrics or wrist bands have not massively changed the situation, another measure must be implemented to improve patient identification. There are several studies that show the majority of the misidentification events happen on admission and then continue during the whole hospitalization of the patient. Photographs of the patient on admission could help with this issue as face identification is easy and reliable. Given that nowadays, social media are gaining more and more space in contemporary lifestyle, a social media like patient EHR could certainly help with admissions. The new EHR will have the patient photograph in the centre, will include patient demographics, date of birth and hospital number, their location within the hospital, their social history as well as links to their documented and verified allergies, past medical history and medication replacing the existing patient page with a complete patient profile. All this information apart from the photograph, exists already in the electronic health records that are currently used, but it can be found only inside notes or in old scanned paper notes, making it extremely difficult and time consuming for clinicians to have a quick idea of the patient themselves.
The suggestion of this paper is as follows: typing the patient hospital number on the EHR will lead to the patient profile page that can be used afterwards to find more options via hyperlinks, for example investigation results or requests, discharge summaries or ward round notes and reviews by several specialties. However, the first tab will open with the patient profile (photograph and basic information as mentioned above), creating a friendly and more comfortable environment for clinicians to know about their patient. A picture of the existing EHR as well as a sample of the proposed EHR with the patient profile is shown below.
Anticipated outcome
Some attempts have been done recently to add photographs in EHR purely for identification reasons and the results are more than encouraging. In addition, introducing photographs by the patient bed side in ICU wards has proven more engagement of nurses with patients as it prevents the patient loss of their identity. Another study in radiology sector shows that there is great value in patient misidentification prevention if photographs of patients are put next to their radiology films. Consequently, it may worth it trying a patient profile EHR, which will include patient photographs and important information that will form the patient as a human individual and not as a web page. Providing only the name and date of birth of the patient is not helpful for the doctor to form a real person in their mind contrary to providing them with a photograph and a detailed history with all kind of information, such as job and habits, which forms a true human being. In addition to that, having a patient’s photograph as a baseline for their clinical condition is extremely valuable for the clinician to compare with their current one. This has several implementations in various conditions such as weight loss or jaundice where the clinician can recognize changes on the patient’s face. Transforming the EHR in a platform full of real people and not full of web pages that represent individuals can contribute in reducing identification mistakes, improve the relationship between patients and clinicians, aid in differential diagnosis and also make information about each patient easily found and retrievable.
Issues and concerns
Financial cost
There are several issues and concerns rising if a new EHR based on patient profiles is to be implemented. First comes the most popular issue that hides behind every change, the budget. Informatics is an expensive sector and whenever an innovation is needed there are always discouraging factors. A refurbished system requires new software, staff training and new devices such as cameras for patient photographs. Even though the above are resources-consuming, it is evident that an investigation of expenses and benefits is essential. For example, electronic prescribing was proven to reduce the mistakes in such an extent that NHS Trusts were saving money eventually. Also, training in new systems in Chicago Hospitals was proven to reduce staff turnover from 25% to 15% and also to increase patient satisfaction from 83% to 91%. In general, EHRs have been proven to reduce costs compared to paper notes. This will be the case with the improved EHR including patient profiles, as they may increase clinicians’ effectiveness, improve patient care and prevent mistakes that will overall contribute in a more cost-effective environment.
Confidentiality
Another concern will be patient confidentiality and privacy as the principle of this paper is introducing a patient profile that contains a photograph as well as several information regarding each patient.Let’s have a look into current EHRs(Figure 1)and how they work. At the minute, EHRs contain multiple information about each patient and access to them have only clinicians that are responsible for the care of every patient and nobody else. The systems are secure, require a personalised card and a password and prevent any inappropriate person to review details of the patient. The new patient profile will be as well access restricted and it will be only available on certain clinicians that deal with this patient. As a result, photographs are another part of the general patient information that already exists and is used securely in EHRs, so there is no reason for confidentiality concerns.
Time
Time and its precious character in ED, will certainly be another concern. Adequate training of the staff and good quality cameras will resolve this problem soon as it will take seconds for the photograph to be taken. Regarding the information needed for completing the patient profile(Figure 2), this is already being taken by the clerking doctor, though it is not stored in an evident place in the patient’s page causing misunderstandings and confusion. As a result, new EHRs should not result in a more time-consuming patient admission.
Special circumstances
Trauma patients with their face affected or patients with face dysmorphia is another issue as well. This particular group of patients can have a generic non-specific picture on their profile instead of a real photograph and the reason should be highlighted below it. In this way, clinicians will be aware that they need to pay extra attention to identify these patients and when it is possible to equip their profile with a photograph if their condition after their recovery allows them to.
Patient reluctance to change
Patient factors such as hesitation and reluctance, should be rationally respected and taken into serious consideration. It seems by the everyday practice that patients are willing to share their personal information with clinicians to improve their care. But the photograph part of their profile will be new and whatever is new faces questioning. Consequently, benefits of the photo should be discussed and analysed briefly with the patient during their admission procedure. Information leaflets and campaigns before any implementation of the plan could also help patients familiarize with the idea. Nevertheless, when Germany Health System introduced the medical ID card that included the patient’s photo, they were surprised to see that patients were more than happy to accept its use. A trial of the new EHR in the UK that will result in positive changes of the NHS will certainly lead to increasing patient satisfaction and secondarily to acceptance[36-38].
Conclusion
Innovative changes and new plans will be always a trigger for thought not only in Healthcare Systems but in every aspect of sociopolitical activity. Technological advances are a major feature in these changes and transform a thought into an action. In terms of EHRs, as they form the main documentation system currently and they are becoming increasingly popular, they will be definitely influenced by technology in the future in an attempt for improvement. Introducing photographs as well as a detailed profile that contains all patient information uses current technology and improves in an easy and effective way contemporary EHRs. However, excessive attention as well as further research is required in order to achieve an innovative and useful EHR that will ensure patient safety and confidentiality.
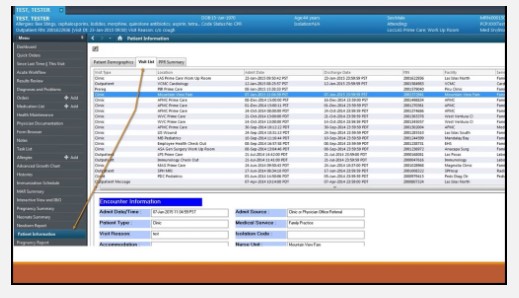
Figure 1 Current cerner system sample (EHR as it looks now), (EHR, 2018).
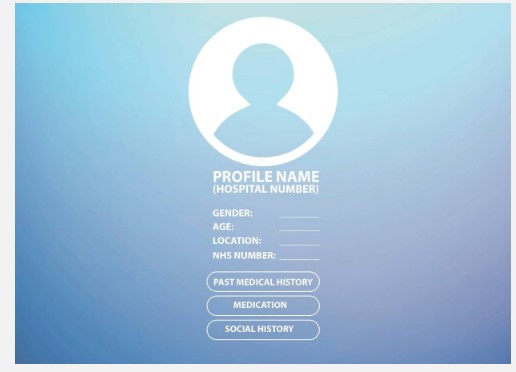
Figure 2: Patient profile (sample).
Citation: Anastasiadou S (2019)A New Electronic Health Record.J Surg Insights: JSI-100007.