Journal of Surgery and Insights
Case Report
Transpalatal Distraction as a Method of Maxillary Expansion: A Case Report
Santos LCB, de Sousa Filho GC, Falcão Batista RM, Correia MCB, Marques KMG, Veras SRA, da Silva GSG, da Silva SMS, Lima e NS and Fontes LBC*
Department of Clinical and Preventive Dentistry, Federal University of Pernambuco, Brazil
*Corresponding author: Luciana de Barros Correia Fontes, Department of Clinical and Preventive Dentistry, Federal University of Pernambuco, Brazil, Tel: +558121268000; Email: lu.bc.f@hotmail.com
Citation: Santos LCB, de Sousa Filho GC, Falcão Batista RM, Correia MCB, Marques KMG, et al. (2019) Transpalatal Distraction as a Method of Maxillary Expansion: A Case Report. J Surg Insights: JSI-100006.
Received date: 21 June, 2019; Accepted date: 10 July, 2019; Published date: 19 July, 2019
Abstract
Transverse maxillary deficiency represents one of the most frequent dent facial anomalies. Among the treatment alternatives, the use of transpalatal distractors have deserved emphasis, particularly in patients with consolidated growth. This provides increased structure, through graded tensile forces between surgically separated bone segments. However, there are controversies about the advantages and limitations of this technique. This report describes the case of 26-year-old a male patient treated by surgically assisted rapid maxillary expansion with transpalatal distractor associated with the removal of the third molars.
Keywords: Adult; Osteotomy; Palatal expansion technique
Introduction
Transverse maxillary deficiency is the most prevalent dent facial deformity and requires intervention, as soon as possible, due to the implications of craniofacial growth, harmony and aesthetics, as to the respiratory mode and the performance of stomatognathic functions [1].
This problem can be corrected by slow expansion with orthodontic appliances or by rapid expansion, surgically assisted or not. This depends on the condition presented, its degree of severity and the age range of the affected individual, particularly in relation to the consolidated craniofacial growth. Among the treatment alternatives, there is still controversy regarding the indication of surgically assisted intervention and the use of screws, in the context of Rapid Maxillary Expansion (RME); in particular, with regard to the parameters that should be adopted for their indication, execution and control [2,3].
Maxillary expansion in adults is object of intense controversy and is still considered an unreliable procedure within the orthodontic community. Therefore, the surgically assisted RME is still considered the elective treatment nowadays. Hyrax is the most suitable expander for RME, whether it is surgically assisted or non-surgically assisted. It is considered the use of the palatal distractor, in cases where the dental support is compromised or when some difficulty is found in the installation of the orthodontic appliance. The osteogenic distraction is a surgical method where the principles of Ilisarov are considered; after the osteotomies, it is expected around 7 days to activate the device, in order to lengthen the bone 1 mm a day. Other modality of surgical expansion is obtained by performing Effort I osteotomies, segmented in very reserved situations. In patients over 14-year-old who require palatal disjunction, the indication of surgically assisted expansions should be considered [4-7].
Transpalatal Distraction (TPD) has been established as a technique for Surgical Assisted Rapid Palatal/Maxillary Expansion (SARPE/SARME) in order to correct transverse maxillary deficiency greater than 5mm. and according to the individual needs. TPD is a safe, powerful and reliable procedure and can be recommended as a state of the art procedure for the individually adapted correction of transverse maxillary deficiency if well-known parameters of distraction are respected. Complications are not expected that interfered with that therapeutic aim, particularly with bone anchorage device; but there was a wide variance of parameters which impedes evidence based statements. Therefore, it is necessary to describe and control more cases using this resource [7,8].
The major advantage of TPD is that forces are acting directly to the bone at the me the mechanically desired level. Tooth tipping or necrosis of the palatal gingiva is not to be feared for. The mechanical environment formed in the area of distraction stimulates the differentiation of pluripotent cells, neovascularization, osteogenesis and remodeling of the neoformed bone. Opinions differ regarding the length of the retention period after RME or Rapid Palatal Expansion (RPE). Active root resorption slows significantly after about three months’ retention and alveolar bone remodeling as long as 23 months’ post expansion [9,10]. The aim of this study was to report the case of a young adult patient with severe maxillary deficiency, who presented difficulty for the Hyrax expander installation, treated by Trans palatal Distraction (TPD).
Case report
A 26-year-old male patient, with severe maxillary deficiency, obstructive sleep apnea and oral breathing, presented at the Maxillofacial Surgery Reference Service of Pernambuco, in the city of Recife, northeast of Brazil, with referral for rapid expansion, surgically assisted. His main complaint was aesthetic due to facial asymmetry, he said that the chin was too large. He denied joint pain.
After the initial physical examination and the analysis of the images, it was found that he presented bilateral posterior cross bite, maxillary retrusion, (negative deviation at 5.73mm), effective short maxillary and mandibular length (negative deviations of 19.45mm and 6.21mm respectively), and reduced upper airspace (negative deviation of 7.33 mm), as major changes. Orthognathic surgery was indicated since skeletal changes could aggravate obstructive sleep apnea. However, before advancing the maxilla, transverse expansion was necessary, with installation of the TPD and osteotomies to reduce the areas of resistance, in addition to the exodontia. Figure 1 shows the teeth in occlusion (frontal and lateral view) and the upper and lower arches.
Description of the technique
Patient, under hypotensive anesthesia Conventional osteotomies were initially performed to decrease the resistance in the maxillary pterygoid region to the piriform region, on both sides and from the anterior nasal spine region to the inter-incisal region. Suture was then performed with resorb able 5-0 thread (Figure 2).
After suturing, the distractor was placed in the region without the need for incisions and trans fixation in the palatal region by means of 4 × 1.5 × 10 mm screws. This was activated twice a day (morning and evening) and the resistance break was verified. The distractor is selected according to the existing interpalatal distance and fixed region of the palate, observing the position R and L marked in the distractor.
There was antibiotic prophylaxis, with application of Chlorhexidine Digluconate 0.2% in the immediate preoperative phase. Postoperative phase prescription: Cefalexin 500 mg and Paracetamol 500 mg ? Codeíne 30 mg combinations versus (every 6hours) for 8 days, in addition to mouthwashes with Chlorhexidine Digluconate 0.12% (every 12 hours for 7 days). From the second postoperative day the patient complained continued pain, even with the prescription of Ketorolac Tromethamine10mg (every 12 hours). There was suspicion of infection in the palate, with the supplementation of local irrigation with Chlorhexidine. Complete remission of symptoms occurred at the 14-day control, with the CT performed (Figure 5).
Conclusion
The use of the transpalatal distractor is easy to install and has the advantage of applying force directly to the bone, avoiding overloading of the dental elements. There were discomfortand functional impairment during four days, in the postoperative phase. As a disadvantage we can mention the addition of one more surgical time, although it did not occur in this case. There are also risks inherent in the technique such as infections. We believe that further studies with a comparative comparison with Hyrax should be performed so that we can safely verify the actual indication of this technique.

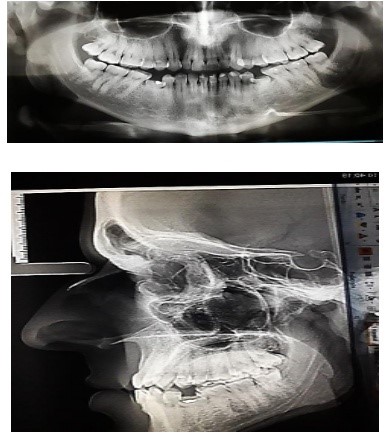
Figure 1: Intraoral and radiographic images.

Figure 2: Sequence osteotomy using piezoelectric and reciprocating saw, application of hemostatic gel during the suture procedure.
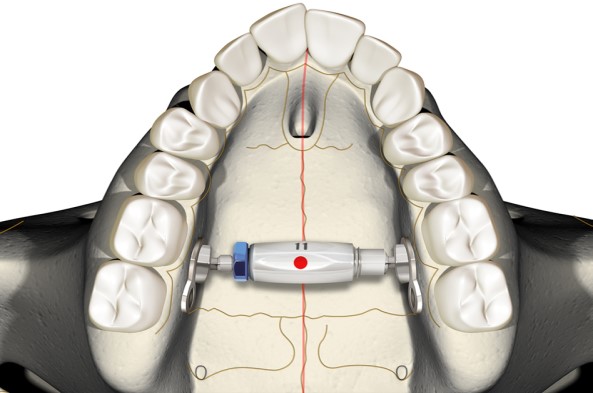
Figure 3: Drawing illustrating the Bone-Borne Distractor device placed on the Maxilla.10.

Figure 4: First activation eight days after surgery and in the following sequence after seven days of activation.
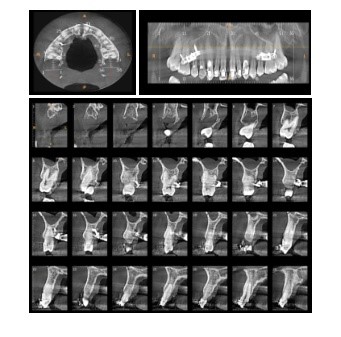
Figure 5: CT scan with axial, coronal and sagittal maxillary images 15 days after surgery.
Citation: Santos LCB, de Sousa Filho GC, Falcão Batista RM, Correia MCB, Marques KMG, et al. (2019) Transpalatal Distraction as a Method of Maxillary Expansion: A Case Report. J Surg Insights: JSI-100006.