Journal of Surgery and Insights
Case Report
Six Years' Outcomes after Long Segment Left Anterior Descending Endarterectomy and Its Reconstruction using Left Internal Thoracic Artery
Mhd Koussai CHOK1, Mhd Yaser HAIDAR2, Marina J ALATA ALLAH2*
1Division of thoracic and cardiovascular surgery, university of kalamoon, Medical city hospital, Dier- Atia, SYRIA
2Faculty of Medicine, University of Kalamoon, Syria
*Corresponding author: Marina J ALATA ALLAH, Faculty of Medicine, University of Kalamoon, Syria, Tel: +9631178 33 999, E-mail: marina.atallah214@gmail.com
Citation: CHOK MK, HAIDER MY, ALLAH MJA (2019) Six Years' Outcomes after Long Segment Left Anterior Descending Endarterectomy and Its Reconstruction using Left Internal Thoracic Artery. J Surg Insights: JSI-100005
Recieved Date: 18 June, 2019; Accepted Date: 24 June, 2019; Published Date: 05 July, 2019
Abstract
Background: Completeness of myocardial revascularization is essential in treatment of coronary artery disease; it is one of the most important factors that influence long-term mortality and morbidity. The number of high-risk and severely diseased patients referred for coronary artery bypass grafting (CABG) has been relatively increasing; the diffusely diseased coronary artery is a challenge for cardiac surgeons. We report a successful case of clinical, echocardiographic, and angiographic outcomes of one patient after 6 years, undergoing coronary endarterectomy of the left anterior descending artery (LAD) with a 98mm long, patch plasty method using the left internal thoracic artery (LITA).
Keywords: Coronary artery bypass surgery; Coronary artery disease
Case Report
A 54-year-old male heavy smoker, with hypertension, was admitted to our hospital for exertional chest discomfort. He had a history of acute coronary syndrome (ACS), 48 hours previously. A preoperative angiogram showed that he had multi vessel disease; severe LMS , proximal LAD, CX, and RCA stenosis (Figure1); with a diffusely diseased LAD. Echocardiography didn’t reveal regional wall motion abnormalities in the LAD, the left circumflex CX, and right coronary RCA arteries territories and good left ventricular systolic function (left ventricular ejection fraction=60%), EuroScores = 7.79%.
He underwent coronary artery bypass grafting via median sternotomy. The left internal thoracic artery (LITA) and long saphenous vein graft were harvested. Cardiopulmonary bypass was instituted using ascending aorta and right atrial appendage cannulations. After cardioplegic arrest, a long coronary arteriotomy was made after the proximal portion of the LAD. The atheromatous core was carefully dissected from the adventitia with a fine spatula and forceps. The proximal atheromatous core was sharply divided, in order to avoid removing the most proximal stenotic lesion. The distal end of the atheromatous core was also divided sharply when it reached the intact intima. The divided intima of the distal LAD was tacked with 8-0 polypropylene sutures. The raw surface of the LAD was flushed with saline and the flaps were removed, taking care not to cause distal embolism with fragments of the incised plaque; the matched length of the LITA was anastomosed to the incised LAD (approximately 98mm) with 7-0 polypropylene sutures. The obtus marginal OM and right coronary artery RCA were bypassed, with a two saphenous vein grafts which were anastomosed proximally to the ascending aorta. The aortic cross-clamping and cardiopulmonary bypass times were 85 and 110 minutes, respectively. Continuous intravenous unfractionated heparin infusion was initiated on the day of the operation Anti-platelet agents (aspirin and clopidogrel) and warfarin (with a target international normalized ratio of 2.0); the patient was discharged on the fifth postoperative day. At clinical follow-up performed yearly until six years later, postoperative; echocardiography and angiography (Figure 2) revealed complete patency of the LITA and the LAD , excellent patient LV function (Figure 3), and the patient was in good condition without angina.
Discussion
In cases involving a diffusely diseased LAD, complete revascularization is not always possible because conventional bypass techniques involving only the distal LAD cannot provide sufficient blood supply to the side branches, including the diagonal branches and septal perforators. The implantation of multiple drug-eluting stents in the diffusely diseased coronary artery has been performed in several institutions. However, stent implantation involves a risk of compromising the flow to the side branches and in-stent restenosis. However, the diffusely diseased LAD remains a challenge for both PCI and CABG. In order to overcome these obstacles, some surgeons have performed the technique of long-patch reconstruction of the LAD with or without endarterectomy, reported clinical and angiographic results [1-8].
Two surgical methods have been developed, known as the closed method (traction technique) and the open method. The closed method is performed by traction of the endarterectomized intima through a small arteriotomy. It does not require much time and the anastomosis is technically easy.
In contrast, the open method involves long arteriotomy and total removal of the atheromas under direct visualization [1]. In this report, we used the open method of performing endarterectomy, as the openings of the septal and diagonal branches and the distal end of the LAD can be directly observed and endarterectomized with confidence. The worst outcomes are associated with incomplete endarterectomy. Any residual intimal flaps should be removed carefully to prevent obstruction of the tributary vessels [1,2].
With respect to the selection of an onlay patch, in general, two options exist: the LITA or a saphenous vein onlay patch. Although Myers et al., have reported that the reconstruction method did not have a significant impact on long-term survival, Japanese investigators recommend using the LITA for reconstruction rather than a saphenous vein graft because of the superior patency rate of the LITA, in our report we used a long skeletonized LITA with about 3 mm of mean diameter and with very good blood flow. Additionally, the use of retrograde cardioplegia is recommended not only for optimal myocardial protection, but also for mechanical flushing and clearance of any debris that may have embolized distally; in this report we used distal SVG anastomosis (SVG-OM, SVG-RCA) for myocardial protection by cardioplegia, during LITA-LAD reconstruction.
The major causes of suboptimal results after coronary endarterectomy are related to triggering of the coagulation cascade by the lack of endothelium in the early stages and myofibrointimal proliferation in the late stages [1,2]. Therefore, strict management with dual antiplatelet therapy and anticoagulation therapy (Anti-vitamin K) AVK should be implemented after endarterectomy.
A search of the literature published in Korea [9], about LSR (long segment reconstruction) of a diffusely diseased LAD, that was reconstructed with long patch angioplasty using the LITA after extensive endarterectomy with outcomes two years after. Therefore, to the best of our knowledge, this case is the first which report longer-term viability (6 years) of this method of reconstruction.
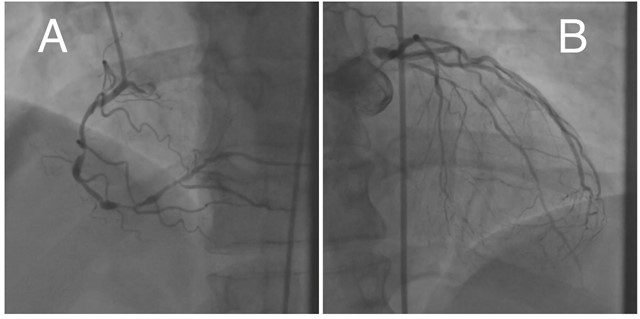
Figure 1: (A) RCA multifocal stenoseis; (B) LMS stenosis > 90 %, LAD multistenosis >80%.
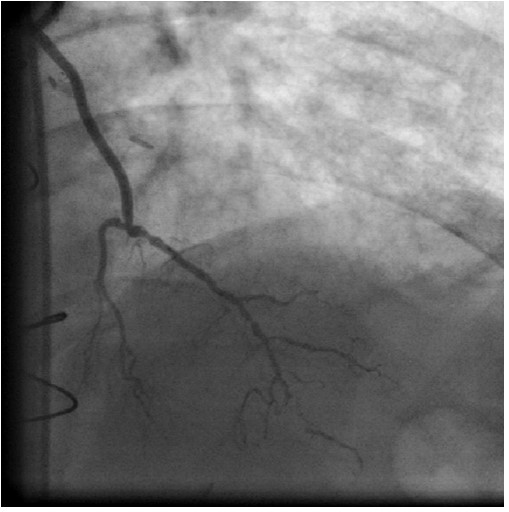
Figure 2: LIMA -LAD Patch angiography.

Figure 3: LV systolic and diastolic.
Citation: CHOK MK, HAIDER MY, ALLAH MJA (2019) Six Years' Outcomes after Long Segment Left Anterior Descending Endarterectomy and Its Reconstruction using Left Internal Thoracic Artery. J Surg Insights: JSI-100005.